

Review Article - Year 2021 - Volume 36 -
Telemedicine applied to plastic surgery: an integrative review
A telemedicina aplicada à cirurgia plástica: uma revisão integrativa
ABSTRACT
Introduction: Telemedicine refers to providing medical services through information technology and communication between patients and service providers. Plastic surgery is a field especially favorable to the application of telemedicine since visual inspection of the patient guides both diagnosis and clinical follow-up.
Methods: An integrative review was performed in the articles published in telemedicine in plastic surgery in the PubMed database, using the terms MeSH: "telemedicine" AND "plastic surgery." After tracking and applying eligibility criteria, the remaining articles' full text were digitized, with their data extracted for detailed analysis.
Results: A total of 134 articles were identified, all in English, in the initial search for PubMed. After screening and application of the exclusion criteria, 12 studies were included for the integrative review. The articles found in this review demonstrated benefits in the use of telemedicine applied to plastic surgery. Especially in the postoperative follow-up of patients, in the reduction or extinction of the need for face-to-face visits, in the satisfaction of patients in the consultations carried out by telemedicine, in the reduction of financial costs and response time for referrals, in the diagnostic accuracy similar to the face-to-face assessment and in improving access to specialized care in remote places, both geographically and socially unfavorable. Four articles discussed barriers and limitations, observed or potential, to the use of telemedicine in plastic surgery, such as data security, legislation, costs and perception of negative influence on doctor-patient communication.
Conclusion: The analyzed studies show an expressive gain in knowledge about telemedicine applied to plastic surgery in recent years.
Keywords: Telemedicine; Plastic surgery; Telesurgery; Patient care; Review.
RESUMO
Introdução: A telemedicina refere-se à prestação de serviços médicos pelo uso da tecnologia da informação e comunicação entre pacientes e prestadores de serviços. A cirurgia plástica é um campo especialmente favorável à aplicação da telemedicina, dado que a inspeção visual do paciente orienta tanto o diagnóstico como o acompanhamento clínico.
Métodos: Foi realizada revisão integrativa nos artigos publicados em telemedicina em cirurgia plástica na base de dados PubMed, utilizando os termos MeSH: "telemedicine" AND "plastic surgery". Após rastreamento e aplicação de critérios de elegibilidade, o texto completo dos artigos remanescentes foi digitalizado, com seus dados extraídos para análise detalhada.
Resultados: Foram identificados 134 artigos, todos em inglês, na busca inicial no PubMed. Após rastreamento e aplicação dos critérios de exclusão, foram incluídos 12 estudos para a revisão integrativa. Os artigos encontrados nesta revisão demonstraram benefícios na utilização da telemedicina aplicada à cirurgia plástica, de forma mais pronunciada no acompanhamento pós-operatório dos pacientes, redução ou extinção da necessidade de visitas presenciais, satisfação dos pacientes nas consultas realizadas por telemedicina, redução de custos financeiros, redução de tempo de resposta para referências, acurácia diagnóstica semelhante à avaliação presencial e melhoria ao acesso de cuidado especializado a lugares remotos, tanto geográfica quanto socialmente desfavoráveis. Quatro artigos discutiram barreiras e limitações, observadas ou potenciais, ao uso da telemedicina na cirurgia plástica, como: segurança dos dados, legislação, custos e percepção de influência negativa na comunicação médico-paciente.
Conclusão: Os estudos analisados demonstram ganho expressivo nos conhecimentos acerca da telemedicina aplicada à cirurgia plástica nos últimos anos.
Palavras-chave: Telemedicina; Cirurgia plástica; Telecirurgia; Assistência ao paciente; Revisão
INTRODUCTION
The consolidation of the information age, with its exponential increase in new and advanced technologies and its electronic sophistication, also brings a new reality to the health área1-4, with its arsenal reaching practically all the processes involved in this area, from management, passing to the doctor’s office - a place previously safeguarded, almost inviolable, from the doctor-patient relationship - until the teaching process. Although the proliferation of technologies is still criticized for threatening the traditional doctor-patient relationship, the potential benefits derived from this relevant matrix deserve consideration by everyone involved in this area1,2,5-8.
Telemedicine refers to providing medical services through the use of information technology and communication between patients and service providers, separated by geographical distances1) that may make personal encounters impractical. Given the rapid development of telecommunications technologies, the concept of telemedicine has grown to cover a wide range of applications1. Previous studies have shown that telehealth technology improves the results in several areas, including the management of diabetes, hypertension and chronic obstructive pulmonary disease5,9,10. There is a description of a reduction in hospital admission rates in patients using telemedicine11.
Plastic surgery is an especially favorable field for the application of telemedicine, given that the visual inspection of the patient in this specialty greatly guides both the diagnosis and the clinical monitoring of the patient2,6,12,13. Although the advantages of telemedicine are widely applied to all professionals, recent advances in accessibility, quality and transferability of photo and video media are of particular relevance for plastic surgeons, given the highly visual nature of their work14,15.
As demonstrated in this review, the new articles show that telemedicine has a special potential in increasing the efficiency of evaluation and postoperative follow-up in plastic surgery, both reparative2 and aesthetics7,8. It improves coordination and facilitates interprofessional collaboration in time and space1,2, eliminates a significant number of unnecessary referrals16) and connects patients located far from large medical centers to experienced professionals1,2,14, without compromising - and even improving7) - the quality or accuracy of the care provided1,2,17,18. Besides, it can be applied to several areas of plastic surgery, such as complex wound18,19, burns16,18) and their sequelae18, cleft lip and palate15) and pediatric plastic surgery15. Nevertheless, it must be considered that the implementation of telemedicine can be challenging and costly20,21. Some factors can limit the broader adoption of these systems, such as the cost of initial audio, video, network and storage installations, licensing problems with suppliers, non-standard electronic systems for medical records, absence or poor coverage by insurance companies and health care operators and lack of standardized legislative regulations3.
It is also important that historical observation is made during the period in which this review was carried out. Not only geographic factors are the reason for implementing telemedicine-based systems. On January 30, 2020, WHO declared the outbreak of COVID-19 a public health emergency of international interest and, in March 2020, began to characterize it as a pandemic to emphasize the seriousness of the situation and urge all countries to take action to detect infection and prevent spread22,23. In this scenario, the new coronavirus may have been a catalyst for a movement in several spheres of products and services, including the health area, towards digital23.
Given the rapid pace of technological advances in the 21st century, associated with the possible effects of social isolation imposed by the pandemic by COVID-1923,24, the authors considered it appropriate to publish an update of a review by Vyas et al. (2017)4, to synthesize the new evidence available in the literature since its presentation in June 2016.
METHODS
Similarly, to the methodology described in the review by Vyas et al. (2017)4, an integrative review was carried out on articles published in telemedicine in plastic surgery in the PubMed database, using the following MeSH terms: “telemedicine” AND “plastic surgery”, in an advanced search. From the references obtained, those not directly related to plastic surgery or that did not have a summary available in the database were excluded by the title. They were excluded case reports or case series with n <10, texts that did not relate to the guiding questions (telemedicine, plastic surgery and assistance), review studies and those published before June 2016, date of submission to the magazine4) of the last systematic review on the theme, which was published in June 2017, provided that they had a citation in the references. The authors extracted data on a subspecialty in plastic surgery, purpose, study design, intervention, results and conclusions. The references of the included articles were scanned for additional studies.
RESULTS AND DISCUSSION
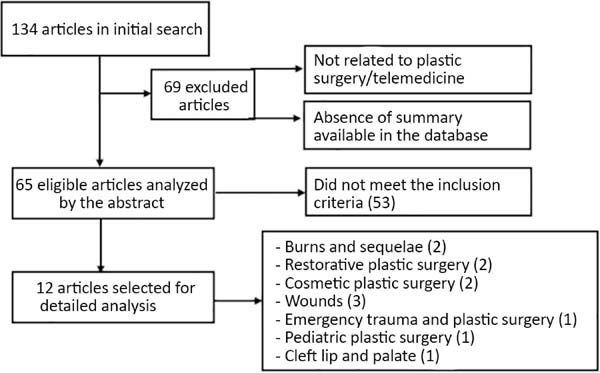
One hundred thirty-four articles were identified, all in English, in the initial search on PubMed. Although language filters were not stipulated, all references found contained text in English. Sixty-nine were excluded for not being directly related to plastic surgery and telemedicine or for not having a summary available in the database. Of the 65 remaining articles, 53 were excluded by reading the abstracts because they are case reports or case series with n <10, have texts that are not related to the guiding questions (telemedicine and plastic surgery), are review studies or have published before June 2016. In this last issue of the publication date, there were two articles with a publication date before June 2016; however, as their inclusions were not identified in the analysis carried out in the last review of the topic, sent for publication by Vyas et al., in 2016 and published in 20174, these were included in the present review. Therefore, 12 articles were included and reviewed in detail. The twelve articles focused on telemedicine in plastic surgery included: 2 in the treatment of wounds, 3 in the treatment of burns and their sequelae, 1 in trauma and emergencies in plastic surgery, 1 in cleft lip and palate, 1 in pediatric plastic surgery, 2 in plastic surgery aesthetic and 2 in evaluation and follow-up in reconstructive plastic surgery (Figure 1).
All twelve articles selected for this review were analyzed in detail, and their objectives, methods, results and conclusions are described in Chart 1.
| Reference (Year), Country | Primary Objective | Methods | Findings | Conclusions |
|---|---|---|---|---|
| Douglas et al.1 (2018), United States | Review the video teleconsultation (VTC) experience in the Connecticut VA health system and research patients' attitudes toward telemedicine services in this context. | Cross-sectional study through the application of qualitative and quantitative questionnaires to assess patient satisfaction with the medical service. | In a score scale that goes up to 10 points, patients positively evaluated the overall quality of interaction with their physician (note: 9.2), their ability to communicate (note: 9.3) and their overall satisfaction (note: 9.2). Patients classified video and sound quality with grades 8.6 and 9.0, respectively. 83% stated that they would prefer the consultation of telehealth to personal visits for future plastic surgery problems, and 7 patients (17%) said they would prefer a personal visit. | Live interactive telemedicine consultation with a plastic surgeon in the VA health care system results in substantial patient satisfaction with the convenience of accessing medical care in remote communities. |
| Funderburk et al.2 (2019), Lebanon | Develop a process of clinical efficiency improvement and offer optimal patient satisfaction, in the postoperative scenario, through a technical health tool. | Patients living in a predefined area were given the option of monitoring by telehealth and follow-up for 1 year. Cosmetic surgeries were excluded. | Preoperative studies revealed that 73% of patients preferred follow-up visits in person, while satisfaction after the meeting by telehealth was 95%. 96% of patients said they had their questions answered and 97% would use the service again. | Telemedicine is associated with increased patient satisfaction and potentially improved clinical outcomes, without prejudice to follow-up. |
| Pozza et al.7 (2017), UNITED STATES | Evaluate the effectiveness of a smartphone-based plastic surgery postoperative follow-up program. | Retrospectively reviewed, during the period of 1 year, the clinical records of patients undergoing cosmetic surgeries of the face, as well as data from questionnaires and postoperative photographs sent by patients' smartphones. | 50 (96,2%) patients reported that the process improved the quality of their postoperative experience. The protocol allowed the detection of early complications in 3 cases, but complications were detected outside the deadline stipulated for early submission of photographs. | The plastic surgeon can provide virtually early postoperative patient surveillance. Although early photography failed to identify complications, they were detected by later photographs. |
| Westra et al.8 (2015), Netherlands | Investigate whether online consultation is a satisfactory alternative to traditional face-to-face consultation in the postoperative period of face-to-face plastic surgery. | Randomized clinical trial with inclusion of eligible patients in two 6-week postoperative evaluation arms: face-to-face consultation or video consultation, with subsequent completion of scientifically validated questionnaires (PSQ-18, PEQ and TSQ) of satisfaction and evaluation of doctor-patient communication | 31 patients participated. Overall satisfaction was the same in both groups, but there was a significant difference in the dimensions "general satisfaction" (online most satisfied consultation group, P=0.02) and "accessibility and convenience" (less satisfied online consultation group, P=0.01) in the PSQ-18 questionnaire. | Patients were also satisfied with traditional or real-time video consultation in plastic surgery. Online consultation is considered a time-saving alternative to traditional consultation, although it may be perceived by some patients as a negative influence on communication with the doctor. |
| Rimal et al.14 (2017), Australia | Share the experience of authors using technology for the provision of services and care in a geographically challenging environment | Retrospective study of data from patients' medical records for a period of 1 year, including all patients registered in the plastic surgery technical service. | 194 rural patients (66 men and 128 women), 26 of whom were elective cases and 358 follow-up visits in telehealth. 10 patients were treated only via telehealth; 24 patients had their first face-to-face clinical review and additional follow-up via telehealth, and 99 patients were postoperative. The etiology of cases ranged from skin lacerations to complex soft tissue and bone lesions, as well as elective cases of postoperative craniofacial follow-up of the hands. | Telemedicine in plastic surgery can also be used in the pediatric population, especially in remote locations, with minimal access to specialists. |
| Sood et al.17 (2016), France | Analysis of the wound treatment system by telemedicine. | Review of data from the CICAT network (Home Hospital Healing Network), including 5,794 patients, between January 2005 and October 2015. Clinical efficacy and medical-economic results were analyzed. | In the experience of the CICAT wound network, the results showed that 75% of the wounds improved or healed, a 72% reduction in the number of hospitalizations and a 56% reduction in ambulance transfers to healing centers. | Telemedicine can be beneficial in the treatment of wounds, although it is important to note that in some countries legal restrictions can make telemedicine extremely complicated. |
| Rennekampff et al.19 (2015), Germany | Examine the intra- and inter-examiner variability of remote photographic wound closure analysis, as well as the reliability of remote photographic wound analysis with direct clinical evaluation. | Blind analysis by panel of high-resolution image evaluators from two randomized clinical trials. The validity of the photographic image analysis was correlated with clinical evaluations of the time for recovery. | The mean intraclass correlation coefficient of the four examiners was excellent (r = 0.79; 95% confidence interval (CI), 0.61, 1.00). The correlation coefficient between evaluators was good (r = 0.67; 95%, 0.57, 1.00)). The agreement between remote visual evaluation and clinical evaluation at the time of healing was good (r = 0.64; 95%, 0.52, 0.76)). | Remote photographic analysis of skin wounds is a viable tool in clinical studies to assess the time to wound closure. |
| Hughes et al.15 (2017), USA and Ecuador | To evaluate the reliability of remote digital video in the preoperative diagnosis of cleft lip and palate in environments with few resources in rural Ecuador, as well as to evaluate the possible economic gains generated with the adoption of this technology. | Retrospective analysis of video data during preoperative evaluations by a craniofacial surgeon in patients in February 2015, with classification of each patient with the same objective criteria. Analysis of the percentage of agreement between the two groups and the reliability among evaluators. | A 95.7% agreement was found among the observers for cleft lip, with substantial reliability (k = 0.78, P< 0.01). There was agreement of 82.6% among the observers for cleft palate, with moderate reliability (k=0.55, P< 0.01). We found agreement of 47.8% among the observers for alveolar cleft, with a weak and non-significant kappa agreement. | Remote digital evaluations are a reliable way to diagnose labial and palatine cleft preoperatively in the context of interventions in plastic surgeries in low- and middle-income countries. |
| Martinez et al.16 (2017), South Africa | Evaluate the WhatsApp application to facilitate burn treatment and resource allocation. | Review of all queries that used WhatsApp for 18 months, received by two senior doctors from a burn center | 833 communications and 1562 clinical doubts were evaluated. 486 interactions (58%) from inside the hospital. There was no change in the number of surgical interventions, but they reduced outpatient consultations. | WhatsApp has contributed to the reduction of unnecessary referrals and outpatient consultations. |
| Cai et al.18 (2016), Nepal and USA | Test the reliability of the Patient and Observer Scar Assessment Scale (POSAS) using videoconferencing. | Prospective study conducted with three independent observers. They evaluated 85 burn scars from 17 individuals. | Reliability for single evaluator was acceptable (ICC> 0.70). The reliability of the mean of the three evaluators was acceptable (ICC> 0.70). In the general opinion score, patients consistently reported worse opinion. | Evaluation of burn scars using the POSAS scale can be accurately performed through videoconferencing. |
| Boccara et al.26 (2018), France | Evaluate the quality of method for telemedicine. | Retrospective study with 323 patients. The purpose of using telemedicine was to evaluate the need for surgery. | Correct initial diagnosis in 94.4% (305/323) of cases. Eleven patients (3.4%) were transferred unnecessarily and seven patients (2.2%) were not transferred, despite the need for surgery. | The results encourage the development of telemedicine based on digital photography, although it never replaces clinical examination. |
| Paik et al.25 (2016), UNITED STATES | Evaluate the response of telehealth through an application for consultations related to plastic surgeries. | Quality Assurance/Improvement Study of a trauma center. The study used an application to send images and brief history to plastic surgery teachers. | 42 consultations performed. The agreement between teachers and consultants was 85.7% for face-to-face consultations and 100% for telephone consultations. In four cases of telephone consultations, emergency department providers incorrectly placed splints on injured patients. | The results show that telehealth consultations were able to produce timely and accurate responses in an emergency care unit. |
The pandemic underway for the new SARS-CoV-2 has accelerated the search for the use of medical services at a distance. In this scenario, it is imperative to look for what is in the scientific literature about advances in telemedicine in plastic surgery to promote improvements, exclude failures, and implement innovations, seeking a better adaptive response to the current challenge.
Vyas et al. in 20174) an excellent review of 23 articles focused on telemedicine in plastic surgery. They used the following Terms MeSH: “surgery, plastic; general surgery; surgical procedures, operative; surgery; burns; wounds and injuries; soft tissue injuries; dermatology; teledermatology; teledermatological; maxillofacial injuries; hand; hand injuries; microsurgery; breast; cell phones; orthopedics; telesurgery; remote consultation”. Since then, advances in this area have been notorious, either by the exponential expansion of mobile technology or by the growing familiarity and accessibility to the average consumer. In this context, new articles have emerged and are not included in the review by Vyas et al. (2017)4.
The articles found in this review demonstrated benefits in the use of telemedicine applied to plastic surgery. They were more pronounced in the postoperative follow-up of patients2,7,8,14, reduction or extinction of the need for face-to-face visits1,14,16-19, satisfaction of patients in telemedicine consultations1,2,8, reduction of financial costs1, reduction of response time for referrals25, diagnostic accuracy similar to face-to-face assessment15,17-19,25,26) and improvement in access to specialized care in remote places, both geographically and socially unfavorable1,2,14,15,25. Despite the vast majority of studies showing significant patient satisfaction, it is worth highlighting the selection bias present in these studies. The method of attracting volunteers, willing to be consulted by telemedicine, favors patients’ selection more receptive to this approach1,2,8,25.
In 2015, Westra and Niessen8 conducted a randomized clinical trial comparing the assessment of patient and physician satisfaction in a postoperative follow-up consultation through a real-time video connection and traditional personal consultation, using validated questionnaires of measures of different aspects of health care doctor-patient communication and satisfaction with telemedicine. The results showed that, in general, patients are equally satisfied with traditional consultation or video conferencing. However, online consultation was perceived by some patients as a negative influence on the doctor-patient relationship. Still, even in a study with higher statistical robustness, a small sample size was observed, which was potentiated by the loss of 30% of the initial sample of eligible patients, which may have generated attrition bias.
Four articles discussed barriers and limitations, observed or potential, to the use of telemedicine in plastic surgery, which were: data security, with the need for sophisticated and protected software and hardware so that patient data storage can be free from fraud1,7; regulation and legislation, both in the governmental sphere and in the sphere of private health, for wider adoption of telemedicine in the propaedeutic arsenal1,17; initial financial costs, which can be high, of installing audio, video, data transmission and storage equipment1, perception of negative influence on doctor-patient communication and the probable need for specific training dedicated to doctors and other health professionals in the improvement of their online communication skills8.
Some studies show that the technology present in current smartphones is sufficient to allow an accurate assessment of various pathologies in the field of plastic surgery2,7,8,16,17,25,26. Even apps for routine use can be used as demonstrated by Martinez et al. in 201816, who used the WhatsApp app for communication between various burn patients’ treatment levels. Pozza et al., in 20177, using smartphones, preferred to employ a very specific and protected network for data transmission called HIPPA. This is a sophisticated network with great data security. The use of smartphones reduces the cost of implementing the system and facilitates real-time communication with specialists7,16,25. Specifically in the work of Paik et al., in 201725, the time of face-to-face response and the time of response through virtual communication between emergency services and specialists was measured, finding a significant difference in time, with a great advantage for virtual consultation. Time and cost savings are critical to patient satisfaction and hospital financing.
Douglas et al. (2018)1, Sood et al. (2016)17 and Rennekampff et al. (2015)19, on the other hand, used complex communication networks associated with their own technologies with specific software in the development of telemedicine in their work. These authors were able to find excellent results regarding the reliability of the method, reliability of information, satisfactory clinical judgment, population coverage and reduction of costs with hospitalization and transportation. Further studies would be needed in order to determine the best tool for performing telemedicine, whether through smartphones or some other specific technology for this purpose.
CONCLUSION
The analyzed studies demonstrate the significant gain in knowledge about telemedicine applied to plastic surgery in recent years. The technological incorporation has the power to reduce distances, facilitate the interaction of the doctor-patient binomial without prejudice to care, even in areas where interaction is as fundamental as the health sector.
The focus is not to have these technologies as substitutes for face-to-face care, but as tools to expand and improve care for patients who need evaluation with the plastic surgeon.
Such tools have become more relevant in the pandemic scenario by COVID-19, where social distance has proved to be the most effective measure to slow down contagion due to its potential to prevent direct physical contact, provide continuous service to the community and, possibly, reduce morbidity and mortality due to the disease27.
Much of what has been developed in studies is not yet fully implemented in the different health systems. The challenge of a non-exclusive technological development persists, which is accessible to anyone who needs this care. It is expected that in the adversities caused by the coronavirus, it will be possible to improve the ability to care, either in person or mediated by technologies.
REFERENCES
1. Douglas S, Geiger E, McGregor A, Norwich A, Abbate D, Hsia H, et al. Telehealth in plastic surgery: a veteran's affairs hospital perspective. Plast Reconstr Surg Glob Open [Internet]. 2018 Out; 6(10):e1840. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/30534478
2. Funderburk CD, Batulis NS, Zelones JT, Fisher AH, Prock KL, Markov NP, et al. Innovations in the plastic surgery care pathway: using telemedicine for clinical efficiency and patient satisfaction. Plast Reconstr Surg [Internet]. 2019 Ago; 144(2):507-16. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/31348369
3. Sclafani AP, Romo T. A brave new world: telemedicine and the facial plastic surgeon. Facial Plast Surg [Internet]. 1999; 15(2);153-9. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/11816128
4. Vyas KS, Hambrick HR, Shakir A, Morrison SD, Tran DC, Pearson K, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg [Internet]. 2017 Jun; 78(6):736-68. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/28328635
5. Hersh WR, Helfand M, Wallace J, Kraemer D, Patterson P, Shapiro S, et al. Clinical outcomes resulting from telemedicine interventions: a systematic review. BMC Med Inform Decis Mak [Internet]. 2001; 1:5. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/11737882
6. Gardiner S, Hartzell TL. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg [Internet]. 2012 Mar; 65(3):e47-53. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/22178033
7. Pozza ED, D'Souza GF, DeLeonibus A, Fabiani B, Gharb BB, Zins JE. Patient satisfaction with an early smartphone-based cosmetic surgery postoperative follow-up. Aesthet Surg J [Internet]. 2017 Dez; 38(1):101-9. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29117293
8. Westra I, Niessen FB. Implementing real-time video consultation in plastic surgery. Aesthetic Plast Surg [Internet]. 2015 Out; 39(5):783-90. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26169952
9. Balas EA, Jaffrey F, Kuperman GJ, Boren AS, Brown GD, Pinciroli F, et al. Electronic communication with patients. Evaluation of distance medicine technology. JAMA [Internet]. 1997 Jul; 278(2):152-9. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/9214532
10. Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, et al. Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare [Internet]. 2010; 16(3):120-7. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/20197355
11. Noel HC, Vogel DC, Erdos JJ, Cornwall D, Levin F. Home telehealth reduces healthcare costs. Telemed J E Health [Internet]. 2004; 10(2):170-83. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/15319047
12. Trovato MJ, Scholer AJ, Vallejo E, Buncke GM, Granick MS. eConsultation in plastic and reconstructive surgery. Eplasty [Internet]. 2011; 11:e48. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/22140594
13. Hoppe IC, Lee Y, Granick MS, Scott SS. Digital store and forward imaging as a quality assessment tool for emergency plastic surgery consultations. Eplasty [Internet]. 2014; 14:e1. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/24501615
14. Rimal D, Huang-Fu JH, Gillett D. Our experience in using telehealth for paediatric plastic surgery in Western Australia. ANZ J Surg [Internet]. 2017 Abr; 87(4):277-81. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/28219124
15. Hughes C, Campbell J, Mukhopadhay S, McCormack S, Silverman R, Lalikos J, et al. Remote digital preoperative assessments for cleft lip and palate may improve clinical and economic impact in global plastic surgery. Cleft Palate Craniofac J [Internet]. 2017 Set; 54(5):535-9. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27427933
16. Martinez R, Rogers AD, Numanoglu A, Rode H. The value of WhatsApp communication in paediatric burn care. Burns [Internet]. 2018 Jun; 44(4):947-55. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29395403
17. Sood A, Granick MS, Trial C, Lano J, Palmier S, Ribal E, et al. The role of telemedicine in wound care: a review and analysis of a database of 5,795 patients from a mobile wound-healing center in Languedoc-Roussillon, France. Plast Reconstr Surg [Internet]. 2016 Set; 138(3 Supl 1):248S-56S. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27556769
18. Cai LZ, Caceres M, Dangol MK, Nakarmi K, Rai SM, Chang J, et al. Accuracy of remote burn scar evaluation via live video- conferencing technology. Burns [Internet]. 2016 Dez 05; [Epub ahead of print]. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27931764
19. Rennekampff HO, Fimmers R, Metelmann HR, Schumann H, Tenehaus M. Reliability of photographic analysis of wound epithelialization assessed in human skin graft donor sites and epidermolysis bullosa wounds. Trials [Internet]. 2015 Mai; 16:235. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26018577
20. Atiyeh B, Dibo SA, Janom HH. Telemedicine and burns: an overview. Ann Burns Fire Disasters [Internet]. 2014 Jun; 27(2):87-93. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/26170782
21. Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med Inform Decis Mak [Internet]. 2012 Jan; 12:1. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/22217121
22. Güner R, Hasanoglu I, Aktas F. COVID-19: prevention and control measures in community. Turk J Med Sci [Internet]. 2020 Abr; 50(SI-1):571-7. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/32293835
23. Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill [Internet]. 2020 Abr; 6(2):e18810. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/32238336
24. Ahn DG, Shin HJ, Kim MH, Lee S, Kim HS, Myoung J, et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J Microbiol Biotechnol [Internet]. 2020 Mar; 30(3):313-24. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/32238757
25. Paik AM, Granick MS, Scott S. Plastic surgery telehealth consultation expedites Emergency Department treatment. J Telemed Telecare [Internet]. 2017 Fev; 23(2):321-7. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/27056907
26. Boccara D, Bekara F, Soussi S, Legrand M, Chaouat M, Mimoun M, et al. Ongoing development and evaluation of a method of telemedicine: burn care management with a smartphone. J Burn Care Res [Internet]. 2018 Jun; 39(4):580-4. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/29789857
27. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health [Internet]. 2020 Ago; 20(1):1193. Disponível em: https://www.ncbi.nlm.nih.gov/pubmed/32738884
1. Universidade Federal de Sergipe, Programa de Pós-Graduação de Gestão e Inovação
em Saúde, Aracaju, SE, Brasil.
2. Universidade Federal de Sergipe, Programa de Pós-Graduação de Ciências da Saúde,
Aracaju, SE, Brasil.
Corresponding author: Kênya de Souza Borges Avenida Doutor José Machado de Souza, 220, Sala 304, Ed. Neo Office, Jardins, Aracaju, SE, Brazil. Zip Code: 49025-740. E-mail: kenyaborges08@yahoo.com.br
Article received: August 25, 2020.
Article accepted: November 10, 2021.
Conflicts of interest: none
COLLABORATIONS
KSB Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Methodology, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing
VOBO Analysis and/or data interpretation, Conception and design study, Data Curation, Final manuscript approval, Methodology, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing
JBCF Analysis and/or data interpretation, Conception and design study, Data Curation, Final manuscript approval, Methodology, Project Administration, Writing - Original Draft Preparation, Writing - Review & Editing
SMS Conception and design study, Final manuscript approval, Supervision
AAO Conception and design study, Final manuscript approval, Supervision
CAL Conception and design study, Final manuscript approval, Supervision





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter