

Original Article - Year 2021 - Volume 36 -
The dorsal scapular artery in the lower third of the trapezius muscle
A artéria dorsal da escápula no terço inferior do músculo trapézio
ABSTRACT
Introduction: The dorsal scapular artery angiosome (DSAA) has aroused growing interest among repairing surgeons, although the most common applications of the trapezoid muscle (TM) are by the arc of rotation of the transverse cervical artery (TCA) and its angiomoses, more cephalic, sufficient for reconstruction purposes in the head and neck. The possibility of obtaining flaps of large cutaneous territory for reconstructions on the back stimulates the study of DSAA angiomoses.
Methods: Eight sides of four fresh cadavers were dissected for DSAA investigation, and 60 sides of 30 volunteers were examined by color Doppler echo in search of DSAA.
Results: Two patterns were described in the course of DSAA in dissections, both irrigating the region of the lower third of the TM. Doppler echo-examination detected emergence and course of DSAA for the lower third of The TM bilaterally in 27 of the volunteers, in two only on the left and was not identified anywhere in one of the volunteers.
Conclusion: There may be two patterns in the course of DSAA irrigating the region of the lower third of the TM. The color Doppler echo-examination determined the emergence and the Path of the DSAA on 56 of the 60 sides examined.
Keywords: Surgical flaps; Blood irrigation; Diagnostic imaging; Regional anatomy; Plastic surgery.
RESUMO
Introdução: O angiossomo da artéria dorsal da escápula (ADE) tem despertado crescente interesse aos cirurgiões reparadores embora as aplicações mais habituais do músculo trapézio (MT) sejam pelo arco de rotação da artéria cervical transversa (ACT) e seu angiossomo, mais cefálico, suficiente para propósitos de reconstrução em cabeça e pescoço. A possibilidade de se obter retalhos de grande território cutâneo para reconstruções no dorso estimula o estudo do angiossomo da ADE.
Métodos: Oito lados de quatro cadáveres frescos foram dissecados para a investigação da ADE e 60 lados de 30 voluntários foram examinados por meio de eco-Doppler colorido, em busca da ADE.
Resultados: Foram descritos dois padrões no curso da ADE nas dissecções, ambos irrigando a região do terço inferior do MT. O exame por eco-Doppler detectou a emergência e o curso da ADE para o terço inferior do MT bilateralmente em 27 dos voluntários, em dois somente à esquerda e não foi identificada em nenhum lado em um dos voluntários.
Conclusão: Pode haver dois padrões no curso da ADE irrigando a região do terço inferior do MT. O exame por eco-Doppler colorido determinou a emergência e o trajeto da ADE em 56 dos 60 lados examinados.
Palavras-chave: Retalhos cirúrgicos; Irrigação sanguínea; Diagnóstico por imagem; Anatomia regional; Cirurgia plástica
INTRODUCTION
Initial studies on the lower portion of the trapezius muscle (TM) in the 1980s gave importance to irrigation by the transverse cervical artery (TCA) 1,2. In the following decade, new studies considered possible variations in the blood supply of TM through the dorsal scapular artery (DSAA) 3. Although underutilized by the conventional way for repairing the head and neck, the applicability of the lower third of the TM has been recommended by applications in the proximity or by free transfer4. The variations in the origin of the pedicle of the DSAA are not important and do not interfere with the procedures in the proximity5. Yet, studies have warned of the importance of preserving DSAA even in flaps based on TCA, for the safety of the lower extremity of these flaps6 The constancy of DSAA branches for the lower third of the TM was found, as well as anastomoses between arterial branches on opposite sides 7,8. However, considering new knowledge about the role of DSAA and its musculocutaneous perforators in the blood supply to the descending portion of the TM and the description of two patterns of irrigation9, the authors felt the need for greater safety for surgical dissections and flap dimensions.
OBJECTIVE
Obtain familiarity with the anatomy of irrigation of the lower third of the TM by anatomical dissections and doppler echo examination.
METHODS
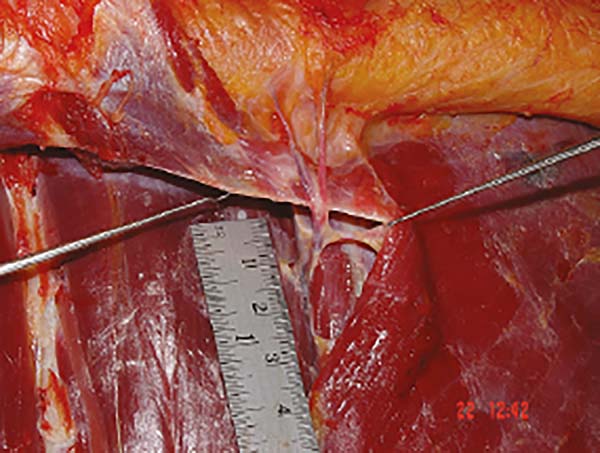
The research protocol was submitted to the research ethics committee of the University of Vale do Sapucaí and approved under number 169/02 on August 20, 2002. The study was carried out from 2002 to 2012. The two sides of four fresh corpses with no injuries or scars on their backs have been studied. A U-shaped incision from the skin to the muscular fascia of the latissimus dorsi muscle was performed from a posterior axillary line to the opposite side, contouring the back at the level of the third lumbar vertebra. This large patch of skin was raised along with the TM on both sides. On each side, the muscle’s origin was carefully separated from the vertebrae and the underlying muscles; the DSAA was identified and preserved. The vessels that ran through the fascia on the deep surface of the flap, outside the limits of the TM and those that emerged from the DSAA were identified and preserved. The flap elevation was conducted to the level of the scapular spine (Figure 1).
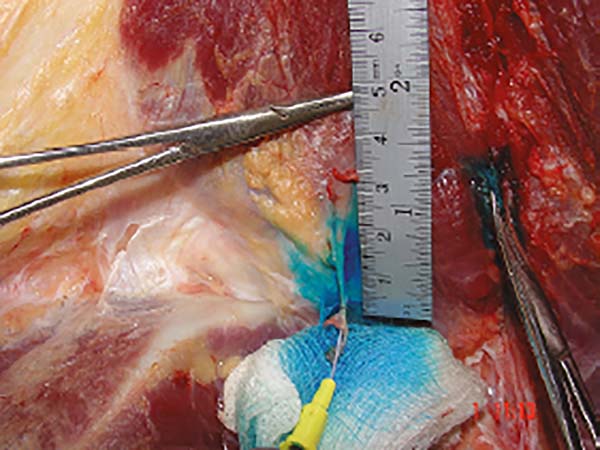
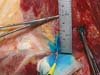
Alternatively, in each corpse, one of the DSAA was catheterized and, by the catheter, injected 20 ml of vital dye (Patent Blue V, Guerbet) to better register and documentation the vessels. Simultaneously, after examining four volunteers by eco-Doppler searching for DSAA as a pilot study, thirty adult volunteers were examined bilaterally. DSAA was studied by a collaborating examiner who specializes in imaging. The equipment used was the Envisor model (Phillips, Bothell, WA, United States) with multifrequency linear transducer (3-12MHz) adjusted for visualization of superficial peripheral vessels. The volunteers were placed in the prone position with the arm on the side being examined along the trunk and with the palmar face of the hand oriented dorsally. The opposite arm was positioned with the hand at the level of the head, and the head was kept with the face turned to the opposite side. The transducer was positioned just below the spine of the scapula and directed medially to search the artery.
RESULTS
About the anatomical study
ADE was present on all eight sides of the corpses studied. Variation in the course of the artery was found. Its emergence from the deep plane to the rhomboid (MR) muscles occurred in two locations: on four sides on the auscultation triangle (triangular space delimited by the lateral margin of the TM, inferior medial margin of the scapula and the medial margin Great Dorsal Muscle GDM), with cephalocaudal course and dimension that varied from 3.5 to 4 cm from the emergency until penetration in the TM, emitting direct branches to the overlying skin, always more than 5 cm caudally to the lower scapular angle ). On the other four sides, in the upper portion of the RM, perforating it at the height of the scapula spine and running caudally along the deep face of the TM, up to the lower third of the muscle. In this conformation, no direct branches to the skin were observed (Figure 3).
About image study
The 8-sided pilot exam of 4 volunteers was sufficient to familiarize the examiner with the findings, and the average exam duration was 20 minutes. On 56 sides, DSAA was found and well described. On two sides (from different volunteers), the artery was visualized on only one side. In a volunteer, the artery was not seen anywhere. In all views, it was present at the level of the scapular spine, medially distant from 0.3 to 2 cm with an average of 1.1 cm, varying in depth, always accompanied by a vein, in a caudal course in the topography of the TM (Figure 4).
DISCUSSION
About the anatomical study
The DSAA irrigates the middle and lower portion of the TM. For some authors, its applicability as a pedicle for flaps in the lower portion of the TM is unlikely due to the reported inconsistency. Some publications do not guarantee its use or limit the dimensions of its skin territory 1,2,8. Other authors describe DSAA as dominant for the lower third of the TM on one third of the sides with a constant path of branches that pierce the RM and enter the deep surface of the TM, supplying its middle and lower portions9. In another study with 15 corpses, through classification based on size, DSAA was the dominant vessel on half of the sides5. It was also the dominant vessel in 15 of 30 dissections3. According to another publication, there are branches of DSAA constant for TM supplying the skin up to more than 10 cm below the lower margin of the muscle7. In a more recent publication, secured by a previous study with portable eco-Doppler, the authors treated ten patients with a flap based on DSAA perforators and TM preservation, six of which were pedicled flaps and four were free4. The present study identified the presence of DSAA on the eight sides studied, with variations that allow the planning of flaps in the lower third of the TM. The variation of the emergence on the auscultation trine offered evidence of the existence of branches for the skin that seems to ensure a cutaneous territory that exceeds the limits of TM. The variation of the emergency through the perforation of the RM makes intimacy with the deep surface of the TM in a caudal course. It emits branches to the muscle that also irrigates the skin. The dye injection allowed the identification of the vessels and their path but did not allow the determination of the cutaneous territory. Both variations irrigate the lower third of the TM.
About image study
The image examination by eco-Doppler is harmless, has low cost, agility, and high sensitivity for detecting arterial vessels 4,10. The DSAA exam required a quick familiarization with the characteristics of the route. The path was constant from the axial plane of the scapular spine, varying the course in depth, which is consistent with the anatomical findings, being able to reach the muscle by emergency in the middle of the RM and go through the deep face of the TM or travel deep to RM and emerge at the auscultation trine. According to the study, there is a possibility of not being identified on some sides. On these sides, there was no way to establish the real absence of the vessel. Still, considering publications that suggest its inconstancy, it is recommended the preoperative examination by echo-Doppler in the flap planning based on DSAA 1,2,8,9.
CONCLUSION
The DSAA was constant on the eight sides studied in cadaver dissections and presented two course variations in the irrigation of the lower portion of the trapezius muscle through penetration at the level of the scapula spine on four sides and the level of the auscultation trigone on four sides. The variation can occur in the same individual. The echo-Doppler examination proved to be feasible and recommended to describe the presence and path of the DSAA. Visualization was possible in 56 of the 60 sides studied.
ACKNOWLEDGMENT
To the then academics Danielle M. Moura and Natali A. Rodrigues and the imagologist Prof. Sizenildo Silva Figueirêdo of the Medicine Course at the Federal University of Rondônia, for his dedication to the study.
REFERENCES
1. Baek SM, Biller HF, Krespi YP, Lawson W. The lower trapezius island myocutaneous flap Ann Plast Surg. 1980 Ago;5(2):108-14.
2. Maruyama Y, Nakajima H, Fujino T, Koda E. The definition of cutaneous vascular territories over the back using selective angiography and the intra-arterial injection of prostaglandin E1: some observations on the use of the lower trapezius myocutaneous flap. Br J Plast Surg. 1981 Abr;34(2):157-61.
3. Netterville JL, Wood DE. The lower trapezius flap. Arch Otolaryngol Head Neck Surg. 1991 Jan;117(1):73-6.
4. Sadigh PL, Chang LR, Hsieh CH, Feng WJ, Jeng SF. The trapezius perforator flap: an underused but versatile option in the reconstruction of local and distant soft- tissue defects. Plast Reconstr Surg. 2014 Sep;134(3):449e-56e.
5. Urken LM, Naidu RK, Lawson W, Biller HF. The lower trapezius island musculocutaneous flap revisited. Arch Otolaryngol Head Neck Surg. 1991 May;117(5):502-11.
6. Cormack GC, George B, Lamberty BGH. The arterial anatomy of skin flaps. 2nd ed. New York: Churchill Livingstone; 1994.
7. Weiglein AH, Haas F, Pierre G. Anatomic basis of the lower trapezius musculocutaneous flap. Surg Radiol Anat. 1996;18(4):257-61.
8. Mathes SJ, Nahai F. Reconstructive surgery: principles, anatomy and technique. New York: Churchill Livingstone; 1997.
9. Yang D, Morris SF. Trapezius muscle: anatomic basis for flap design. Ann Plast Surg. 1998 Jul;41(1):52-7.
10. Berg WA, Chang BW, DeJong MR, Hamper UM. Color Doppler flow mapping of abdominal wall perforating arteries for transverse rectus abdominis myocutaneous flap in breast reconstruction: method and preliminary results. Radiology. 1994 Ago;192(2):447-50.
1. Federal University of Rondônia, Laboratory of Operative Technique, Department of
Medicine, Porto Velho, RO, Brazil.
2. Hospital de Clínicas, Rehabilitation and Assistance Program for the Fissured Face,
Rio Branco, AC, Brazil.
3. Clínica Paiva & Rocha, Surgery, Pouso Alegre, MG, Brazil.
Corresponding author: João Lorenzo Bidart Sampaio Rocha, Avenida Alberto de Barros Cobra, 717, Nova Pouso Alegre, Pouso Alegre, MG, Brazil. Zip Code: 37553-459 E-mail: joaolorenzorocha@gmail.com
Article received: August 10, 2020.
Article accepted: April 23, 2021.
Conflicts of interest: none
COLLABORATIONS
JLBSR Conception and design study, Investigation, Methodology, Realization of operations and/or trials, Writing - Original Draft Preparation
GRP Analysis and/or data interpretation, Data Curation, Investigation, Realization of operations and/or trials, Writing - Review & Editing
LCSR Analysis and/or data interpretation, Investigation, Writing - Review & Editing








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter