

Articles - Year 1998 - Volume 13 -
Contribution to the Reduction Mammaplasty in "L"
Contribuição à Mamaplastia Redutora em L
ABSTRACT
The author maim a brief literature revision on the reduction mammaplasties in "L" presenting after that his personal technique for this procedure. The demarcation used starts like in the c1assical reductions in inverted "T", using, however; a mould modified by the author; (from the one of VVise). Within the demarcation of what would be the inverted "T" surgery, the author makes another demarcation in "L". The skin incisions and removals will follow this second mark, but the glandular tissue excision is made subcutaneously, following the demarcation in "T". The areolomammilar complex is transposed by means of a monopedicled flap with medial base, which permits great excisions, the CAM repositioning with no distortion, and the total preservation of the mammary physiology. With this, a quite satisfactory shape for the new breast is obtained, with minor extension of the final scars and without the medial horizontal branch, more evident with bathing costumes and low necked dresses.
Keywords: reduction mammaplasty; reduction mammaplasty in "L".
RESUMO
O autor faz uma breve revisão da literatura sobre as mamaplastias redutoras em L, apresentando, em seguida, a sua técnica pessoal para esse procedimento. A marcação que utiliza inicia-se como nas reduções clássicas em T invertido, porém utilizando um molde modificado pelo autor, daquele de Wise. Dentro de marcação do que seria a cirurgia em T invertido, faz uma nova marcação em L. As incisões e remoções de pele seguirão essa segunda marca, porém a ressecção do tecido glandular é feita subcutaneamente, seguindo a marcação em T. O complexo aréolo-mamilar é transposto por meio de um retalho monopediculado de base medial que permite grandes ressecções, o reposicionamento do CAM sem qualquer distorção e a total preservação da fisiologia mamária. Com isso, obtém uma forma bastante satisfatória para a nova mama, com cicatrizes finais de menor extensão e sem o ramo horizontal medial, mais evidente com roupas de banho e decotes.
Palavras-chave: mamaplastia redutora; mamaplastia redutora em L
The concern with the incisions size diminution, in reduction mammaplasties, comes from a long time. As of the surgery with final scar in inverted "T", of LEXER(11) in 1912, and the periareolar technique of KAUSCH (9) in 1916, many attempts were made, being that the totality of scar of reduced size, suitable form, preservation of the mammary physiology, and procedure safety, were always the main concerns of all who were devoted to this procedure. HOLLANDER(7) in 1924 was the tirst to perform a mammary reduction, leaving an "L" as a final scar, with the exclusion of the medial scar, always visible in more accentuated low necked dresses. DOUFOURMENTEL and MOULY(6) in 1961, and afterwards in 1968, presented a technique also with "L" final scar, where the operated breast obtained a quite satisfactory shape. MYR and MYR(l3) in 1968, REGNAULTI(15) in 1974, MEYER and KESSELRING(12) in 1975, and SCHATTEN et col.(16) in 1975, also offered important contributions for this procedure. In our milieu, HORIBE et col.(8) in 1976, SEPULVEDA(17) in 1981, BOZOLA et col.(1) in 1982, CHAVEZ et col.(2) in 1988, and CHIARI(3) in 1992, presented technique variations, a few with quite geometrical demarcations and full of calculations, sometimes raising difficulties to its application.
LEJOUR(10) in 1994 published a book showing the association of lipoaspiration with mammaplasties, thus obtaining reduced scars and good results.
for more than 20 years, we have been using the mammaplasties in "L", especially for the pexies with no reduction. But also in many cases of moderated reduction, in young patients, we use the technique in "L" with excellent results.
With a greater control of the technique and with the ample experience obtained in the CAM transposition through monopediculated flap of medial base, that permits the removal of larger amount of glandular-adipose tissue and the CAM repositioning with no distorsion, besides preserving totally the breast physiology as we published in 1982 and in 1991 (4 and 5), adding up to the concepts so well exposed by PEIXOTO(14) in 1979, of breast skin retraction, and contirmed by TARANTO(18) experiences, transmitted in 1995, in personal presentations and not published, we have defined a final form form this technique execution, which we present next.
TECHNIQUE DESCRIPTION
The demorcation is made with the patient standing up, using a modified Wise's mould, with the opening of the lower points of the new areolar arch 7 cm apart (Fig. 1). With this, we tried to have a larger area of skin excision in the periareolar region.
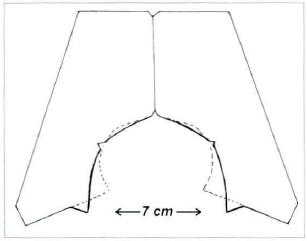
Fig. 1 - Scheme of our persona1 mould, based on Wise's mould. The broken line beyond our mould represents the original mould drawing for comparation.
The basic points follw the classic principles of the STRÖMBERG or SKOOG type mammaplasties, needing no greater details. Once the breast is demarked, as if we were going to make an inverted "T" mammaplasty, with no concern to shorten its horizontal branch, which will be rigorously placed in the submammary groove, we make a second demarcation, now in "L" within the former mark, taking care to place the "L" horizontal line about 2 to 4 cm above the existing mammary groove (Fig. 02a and b).
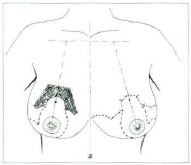
fig. 2a - Demarcation of the basic points and lines, with the patient standing up and with her arms along the body. The mould is placed 1,5 cm above the future mammilar location, corresponding to the submammary groove projection.
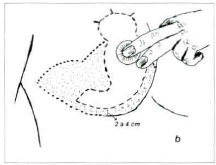
Fig. 2b - View of the marked breast lower part, showing clearly the demarcation as if it was a surgery in "T" (in high dots), and the demarcation for our surgery in "L" (in small lines), that is 2 to 4 cm above the submammary groove. The part to be subcutaneously excised is in fine dots.
In this manner, we will have two demarcations: one in "L", that will determine the cutaneous incisions, and another in "T" that will determine the subcutaneous excisions of the glandular-adipose tissue for the breast volume reduction.
The surgery may be performed under loco-regional or general anesthesia, depending of the surgeon preference and the patient wishes. The dorsum must stay elevated at 30°. A wide infiltration, with 500 ml very cold physiological serum solution, 20 ml of Pupivacaina 0.5 %, and one Adrenalin vial, will help to reduce bleeding and will provide a postoperative analgesia protracted and confortable for the patient.
We wait for 10 minutes for a greater action of the infiltred solution and the surgery is started with the SCHWARZMANN classical maneuver, only in the delimitated area to obtain the medial base flap for the CAM transposition (Fig. 3a).

Fig. 3a - With the breast "stangled" by the assistant, we make the flap deepithelization, that will transpose the medial base CAM. The areole has its diameter reduced to around 4 cm.
We make the cutaneous incisions in the whole "L" mark, detaching after that the skin in the 2 to 4 cm band of the submammary groove, between the "L" and "T" marks, until we reach the muscular plane (Fig. 4).
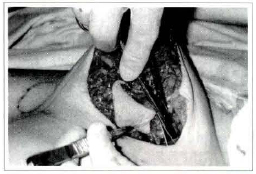
Fig. 4 - Scissors detaching the skin, in a very superficial plane, up to the limit of the inverted "T" demarcation. This detachment may also be made with the number 22 scalpel.
The whole breast is derached in the pectoral supra-aponeuretic plane, which will allow more mobilization and elevation of the breast, when we start its molding. Once concluded these detachments, with a 22 blade scalpel we made the vertical incision of the adipose-glandular tissue subcutaneously, as if it was a mammaplasty in "T", until the muscular plane. In the same piece, the adipose glandular tissue is removed around the medial base flap, wich will conserve all its thickness of the glandular tissue, assuring the breast physiology maintenance.
The removed volume will correspond to the desired reduction. Everything is removed in a single piece (Figs. 3b, 3c, 5 & 6).
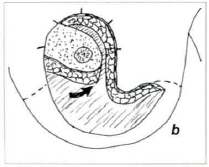
Fig. 3b - The adipose-glandular tissue removed in the muscular plane, together with the skin in the "L" mark, and subcutaneousy in the inverted "T" mark, the thick medial base flap has ample mobility to rotate upwards, to its new position.
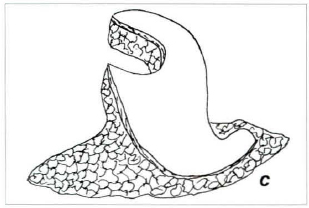
Fig. 3c - Piece removed in one single block, containing the skin in "L" and the subjacent adiposeglandular tissue, including the lower, lateral and medial prolongations removed subcutaneously.
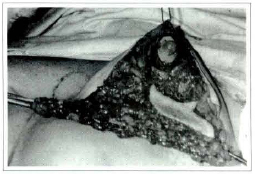
Fig. 5 - Adipose-glandular tissue of the lower, medial and lateral prolongations, exposed after its subcutaneous detachment and in the aponeurotic-muscular plane.

Fig. 6 - Excision around the medial base flap, in continuity to the subcutaneous excision of the lower, medial, and lateral prolongations, in a single piece.
This removal may be made with lipoaspiration, however in very dense breats the result obtained is not satisfactory and, with the surgica1 excision, a greater precision is possible in this procedure, with much less trauma and greater safety.
When the excision of the excedent adipose glandu1ar tissue is completed, a criterious hemostasia is made - since we never use drains - and we start the breast molding. The areole is placed in its new position, through the three upper cardinal points, with the upwards roration of the medial base flap (Fig. 3b). After that, the assistam pulls the breast upwards, through the point given in the areolar north or by means of a hook or Hallis clamp placed there, exposing and positioning the breast medial and lateral columns, that will be fixed among themselves with absorbable 4-0 stitches (Fig. 7), which will give the breast the conical and projected shape. However, we now do not make its fixation in the muscular aponeurosis, since it may cause undesired adhesions, more evident when the patient raises her arms (Fig. 11e).

Fig. 7 - Pulling the breast by its upper pole, together with the medial base flap, we achieve the approach of the medial and lateral colunms that are joined together by means of stitches with slow absortion thread, 4-0. We do not make now the fixing of its base to the pectoral muscular aponeurosis, by the reasons exposed in the text.
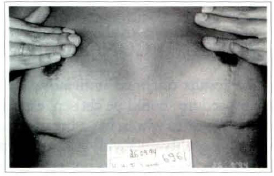
Fig. l1e - View of the submammary scar, showing a small point of adherence and retraction in the right latera horizontal scar, due to a fixing point of the columns on the muscular aponeurosis.
After that, absorbable stitches are applied in the subderna, with the due compensations for the length difference of the lateral and medial flaps. In this moment, we have a view of the very firm and well projected breast (Fig. 8). The thinner skin, where subcutaneous adipose-glandular excisions were made, shows a seeming flabbiness which, within a few days, disappears due to its retraction, in the greater number of cases.
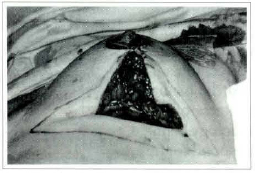
Fig. 8 - Practically molded breast, keeping a pleasant new conical shape, quite firm, with no traction. Observe the "collapsed" skin, here the subcutaneous excision was made.
A careful intradermic continous suture, with quick absorption number 5-0 thread, completes the skin closing (Fig. 9).

Fig. 9 - After finishing the skin intradermic suture, with absorbable thread 05, we can see the demarcation of what would be the skin removal if the classic mammaplasty had been performed in inverted "T". The scar size was reduced.
With adhesive microporous ribbons, afrer that we make a discrete molding and only in the lower half of the breast, that will be left just for one week.
The dressing is made with smooth gauze and placing a suitable brassière.
The patient is advised to wair for 3 days, when she may remove the dressing herself, without removing the adhesive ribbons molding, and start her normal baths, without rubbing the operated area.
The postoperative cares are the same as in any mammaplasty.
CASE HISTORY
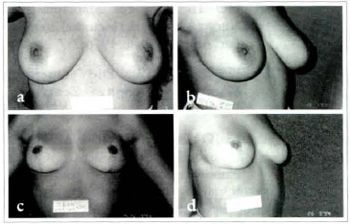
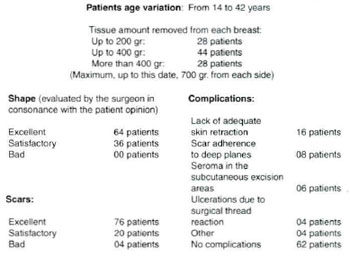
This technique, such as we presented, has been used since 1993 and, in a survey of the last 100 cases with control of more than one year of evolution, from which we have chosen three for this paper illustration (Figs. 10, 11 and 12), we had the following results:
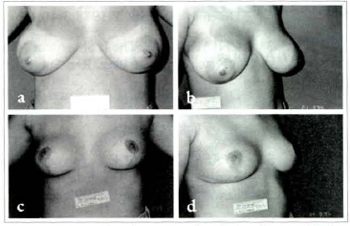
Figs. lOa & 1Oc; lOb & 10d - Patient SCL, 20 years old. Pre operatory and 1 year postoperatory 480 g removed from the left side and 500 g from right.
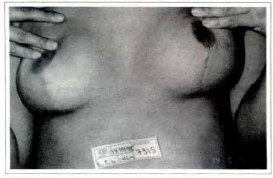
Fig. 1Oe - View of the submammary scar. Good quality and no skin residue.
Figs. 11a & 11c; 11b & 11d - Patient MHF, 16 years old. Pre operatory and 1 year postoperatory. 260 g were removed from left side and 280 g from right.
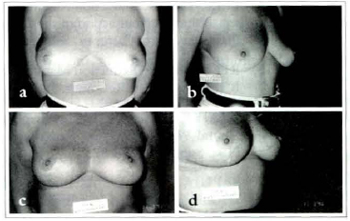
Figs. 12a & 12c; 12b & 12d - Patient MMSC, 39 years old. Pre operatory and 1 year postoperatory. 220 g were removed from left side and 260 g from right. A small breast sliding in the thorax is noticed, giving a greater volume in the lower pole. However, the patient did not complain and nothing was done.
DISCUSSION AND CONCLUSIONS
Revaluating the results obtained until now, we believe that this procedure should be chosen, especially for younger patients or to whom has a breast cutaneous lining of good quality and with good resilience.
In patients with flaccid skin, we do not take the risk of performing this surgery, as the possibility of not occurring the skin retraction and being necessary a revision surgery to remove it, becomes quite probable.
The demarcation is extremely simple and without many geometric calculations. And the fact of making it previously does not signify stereotipy of the surgeries, since it involves references taken in function of the right breast type and of the patient's thorax. Besides, during the surgery, the surgeon sensibility will determine de breasts final shape and not the mould that directed the surgery beginning.
The medial flap, for transposition of the areolomammilar complex, that we have proposed a few years ago, allows the indication of this techique even in cases of great breast volumes, without loss of the shape final quality.
REFERENCES
1. BOZOLA AR et col. Mamoplastia em L: Conrribuição Pessoal. R. AMRIGS 1982;26:207.
2. CHAVES L et col. Mastoplastia em L: um Novo Desenho. Rev. SBCP 1988;3:40.
3. CHIARI JR. A. The L Short-scar Mammaplasty. A New Approach. Plast. Rec. Surg. 1992;90:233.
4. D'ASSUMPÇÃO EA. Tactical Modifications in the Skoog Reduction Mammaplasty. Aesth. Plast. Surg. 198;26:179.
5. D'ASSUMPÇÃO EA. Adenectomia Mamária com Reconstrução Imediata sem Uso de Prótese. Rev. Bras. Mastologia. 1991;1:65.
6 DUFOURMENTEL L & MOULY R. Plastie Mammaire par la Méthode Obliqúe. Ann. Chir. Plast. 1961 ;6:45.
7. HOLLANDER E. Die Operation der Mammahypertrophy und der Hagebrust. Deutsch Med. Wochenschr. 1924;50:1400.
8. HORIBE K et col. Mamaplastia Reductora: Nuevo Abordaje del Método Lateral-obliquo. Rev.
Lat. Am. Cir. Plast. 1976;2:7.
9. KAUSCH W. Die Operationen der Mammahypertrophy. Zentralbl F. Chir. 1916;43:713.
10. LEJOUR M. Vertical Mammaplasty and Liposuction of the Breast. Quality Medical Publishing. St.Louis, Missouri, 1994.
11. LEXER E. Hypertrophiebei der Mammae. Munch Med. Wochenchr. 1912;59:2702.
12. MEYER R & KASSELRING VK. Rduction Mammaplasty with an L Shaped Suture Line. Plast. Rec. Surg. 1975;55:139.
13. MYR Y MYR L. Reduction Mammaplasty. Plast. Rec. Surg. 1968;41:352
14. PEIXOTO GR. Reduction Mammaplasty: a Personal Method. Transaction of the 7th Inter. Cong. Plast. Rec. Surg. Cartgraft, São Paulo, 1979.
15. RGNAUÇT P. Reduction Mammaplasty by the B Tecnique. Plast. Rec. Surg. 1974;53:19.
16. SHATTEN W et col. Further Experiences with Lateral Wedge Resection Mammaplasties. Brit. Plast. Surg. 1975;28:37.
17. SEPULVEDA A. Assimetria Mamária: Tratamento Cirúrgico. Rev. Bras. Cir. 1981;71:11.
18. TARANTO T. Comunicação pessoal. 1995.
I - Senior Member of SBCP and lSAPS. Member of Academia Mineira de Medicina. Plastic Surgeon of Instituto de Cirurgia Plastica de Minas Gerais, Hospital Mater Dei and CIRPLAST.
Address for Correspondence:
Evaldo Alves D'Assumpção, MD
R. Tenente Rcnato Cesar, 48 - Cidade Jardim
30380-110 - Belo Horizonte - MG - Brazil
Phone: (55 31) 296.7420


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter