

Case Report - Year 2021 - Volume 36 -
Mandible microsurgical reconstruction with osteocutaneous fibular flap, with the assistance of a 3D model, in a trauma patient: case report
Reconstrução microcirúrgica de mandíbula com retalho osteocutâneo de fíbula, com auxílio de modelo 3D, em paciente vítima de trauma: relato de caso
ABSTRACT
This is a case report of the mandible microsurgical reconstruction with osteocutaneous fibular flap in a 16-year-old patient. A victim of an assault with a firearm projectile and blunt trauma to the face, resulting in a comminuted mandible fracture, loss of dental elements, and extensive soft tissue injuries. After treatment of the acute phase, we chose microsurgical reconstruction with a free fibula flap due to the mandibular defect's extension and the possibility of dental rehabilitation. The use of three-dimensional models of the mandible and fibula was exceptionally helpful in making the best surgical planning of the osteotomy areas, decreasing the surgery flap's ischemia time.
Keywords: Mandibular reconstruction; Fibula; Microsurgery; Three-dimensional printing; Jaw; Mandibular fractures
RESUMO
Trata-se de um relato de caso de reconstrução microcirúrgica de mandíbula com retalho osteocutâneo de fíbula em um paciente de 16 anos, vítima de agressão com projétil de arma de fogo e trauma contuso em face, acarretando em fratura cominutiva de mandíbula, com perda de elementos dentários e lesões extensas de partes moles. Após tratamento da fase aguda, optou-se pela reconstrução microcirúrgica com retalho livre de fíbula, devido à extensão do defeito mandibular e possibilidade de reabilitação dentária. O uso de modelos tridimensionais da mandíbula e fíbula foram excepcionalmente úteis para tornar possível o melhor planejamento cirúrgico das áreas de osteotomia, com diminuição do tempo de isquemia do retalho da cirurgia.
Palavras-chave: Reconstrução mandibular; Fíbula; Microcirurgia; Impressão tridimensional; Mandíbula; Fraturas mandibulares
INTRODUCTION
The mandible occupies the most considerable bone portion of the facial skeleton1. It plays a crucial role in chewing, swallowing, phonation, speech, and smiling, providing shape, contour, and vertical height of the lower third of the face2. It is the second most common site of fracture of the facial bones3. Mandible fractures, if not identified or treated correctly, can lead to severe sequelae1.
An ideal mandible reconstruction should be similar in structure, geometry, and tissue in the absent area2. The fibular osteocutaneous flap with osteotomies to mimic the mandibular shape was initially described in 1989. Since then, the fibula-free flap with microsurgical anastomosis has become an excellent weapon for mandibular reconstruction4. This flap has the advantage of reconstructing large defects (up to 30 cm), a long vascular pedicle, and the application of osteointegrated dental implants5,6.
With the assistance of computed tomography and the manufacture of models on 3D printers, it is possible to obtain a better aesthetic and functional result of the reconstructed organ, reducing the surgical time and its complications7.
Our objective is to describe a microsurgical reconstruction of the mandible with osteocutaneous fibular flap, in a trauma patient, with the assistance of 3D printing for pre and perioperative planning.
CASE REPORT
Patient, PGLO, 16 years old, smoker, admitted to the Risoleta Tolentino Neves Hospital (HRTN) emergency after being found on a public road, victim of aggression firearm projectile and blunt trauma in the face. Urgent tracheostomy was performed due to airway obstruction.
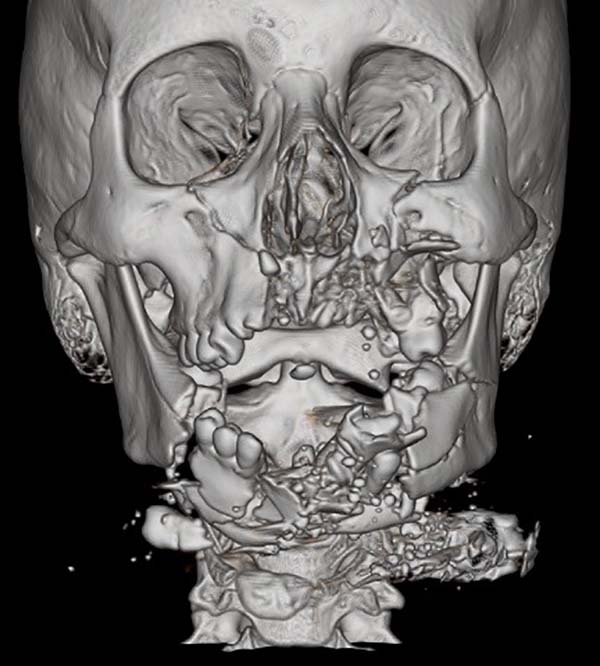
The patient had an open fracture of the mandible, lower dental elements, and several lacerations on the face. Computed tomography of the face showed a comminuted fracture of mandibular bodies and branches, left maxilla with rhinopharynx and oropharynx obstruction due to soft tissue edema (Figure 1).
The patient underwent debridement of devitalized tissues and repair of the lacerations. New debridement was performed on the 20th postoperative day (POD), with fracture fixation using a straight 4-hole plate on the left and a trans-gap reconstruction plate with three screws on each side of the 2.0 system. Facial vessels were identified and preserved. He was discharged on the 3rd POD of the second surgical approach, with good evolution and adequate acceptance of a liquid/pasty diet orally. He was referred to the outpatient clinic to schedule mandibular reconstruction.
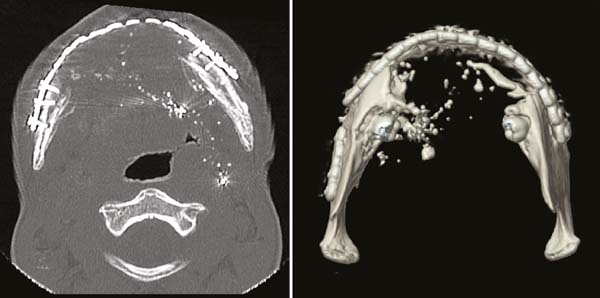
A new face tomography showed the reconstruction plaques joining the mandibular bodies and branches, with a bone loss with an estimated distance of 8 cm between the parts, thus indicating a reconstruction with fibrosurgical osteocutaneous flap of the fibula (Figure 2).
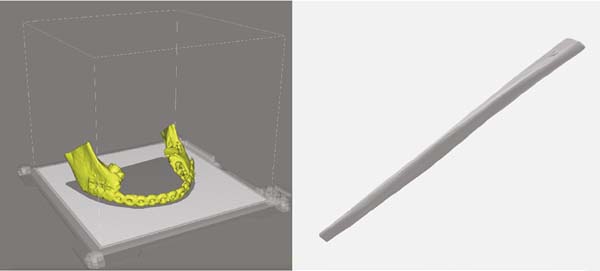
A three-dimensional model of the mandible and plate was made using a polylactic acid filament printer. With it, the surgical team could determine the distance to be filled by the flap, define the side that the pedicle should be positioned in, identify bone spicules to be removed, and program the holes’ positioning for fixing the plate. A fibula model was also created to program where and how osteotomies would be performed on the procedure’s day. During the surgical planning, the functions of each limb were defined (Figures 3 and 4).
Microsurgical reconstruction of the mandible with an osteocutaneous fibular flap occurred five months after the trauma. The 10x5 cm skin island was located 6 cm distal from the fibular head and 5 cm proximal to the lateral malleolus. The perforators in the lateral intermuscular septum were identified. The long and short fibular muscles, anterior intermuscular fascia, finger extensor, and interosseous membrane were dissected, preserving 2-3mm of these structures attached to the fibula; there was no injury to the skin perforators. The gastrocnemius and soleus muscles were dissected, keeping the muscle layer adhered to the bone. Proximal and distal osteotomies were performed in the subperiosteal plane, identifying and ligating the fibular vessels distally. The posterior tibial and flexor hallucis longus muscles were dissected, identified, and linked to the fibular artery at its origin, accompanied by two fibular veins. Osteotomies were performed in the subperiosteal plane using the 3D model of the mandible and fibula as a guide. The models did not contact the patient. The donor area was closed by plans with cutaneous synthesis and partial skin grafting in an area of cutaneous island removal. The transverse cervicotomy was performed, identifying the internal jugular and external carotid veins, isolated the right facial artery, and vein isolated to perform the microsurgical anastomosis. The reconstruction plate was dissected, and it was fixed with new screws. The fibula was fixed to the reconstruction plate’s inner face with three monocortical screws of 2.4x8.0 mm. Microsurgical anastomosis between fibular vessels and right facial vessels was performed with separate points of prolene 8.0 with the assistance of magnifying glasses. The skin flap was fixed in the cervical region for postoperative control of the flap (Figure 5).
The surgical times were simultaneous due to the subdivision of the teams. The surgery lasted eight hours, and the time of total ischemia of the flap was three hours.
The patient was kept in orotracheal intubation (OTI) for 48 hours at the ICU. Mean arterial pressure was maintained above 70 mmHg, without the use of vasoactive amines. Omeprazole 20mg, fixed-dose 8 mg between 8/8 hours for three days. Antithrombotic prophylaxis with enoxaparin 40mg, with the introduction of ASA 100mg orally after the 3rd POD. Amoxicillin antibiotic therapy with clavulanate 500mg + 125mg for ten days. The diet was initiated by nasoenteral tube (NET) at the POI and progressed to the oral route (liquid/pasty) after extubation. Walking with crutches started on the 9th postoperative day (POD) and without restriction after the 14th POD. The flap perfusion was evaluated with a serial clinical examination of the cutaneous island, in addition to an evaluation with Eco-doppler showing good flow in the anastomosis. The patient progressed well and was discharged on the 15th postoperative day.
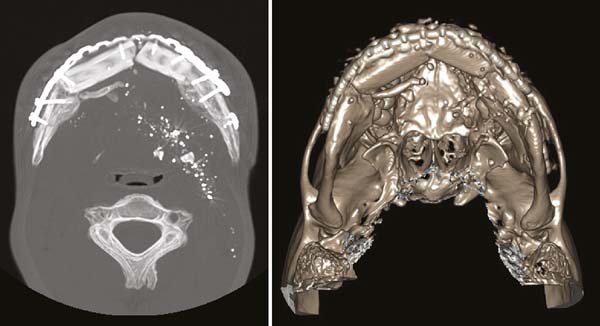
He was followed up on an outpatient basis, maintaining a liquid/pasty diet for 45 days. Control tomography was performed at 40º POD, showing a good-looking flap with no bone resorption signs (Figures 6 and 7).
The patient remains outpatient but did not undergo dental implants due to the financial difficulty and slowness of the public health system’s process.
DISCUSSION
Currently, the technique of choice for mandibular reconstruction is made using vascularized bone flaps.
The fibula-free flap is characterized by being an autogenous graft, segmented and removed from the donor area. Its vascularization is preserved to nourish this tissue when in the recipient bed, from its anastomosis with the recipient region’s vascular system.
Reconstruction planning with prototyping and three-dimensional printers optimizes microsurgical reconstruction with fibula autotransplantation8,9. The association of 3D technology showed several gains for better surgical results and for the patient. There is a shorter surgical time, increased perioperative efficiency, better accuracy in reconstruction in cases of greater difficulty, better osteointegration, and occlusion after implants10.
The planning cost depends on the piece’s size, difficulty processing the image, printing time, and the material used. Nevertheless, because it is a pre-surgical model (does not include guides or molds), it can be developed with printers and non-specific software (non-medical), and this type of technology is more accessible with a price ranging between R $ 900.00-R $ 1,500, 00.
The material used (PLA) requires a temperature of 185-205 ºC for printing, but tests have not yet been carried out on whether the model would suffer distortions during sterilization.
Validated sterility tests and sensitivity tests are also required to allow risk-free contact for the patient. These are being carried out to improve the model and allow greater versatility in its use.
CONCLUSION
The fibular osteocutaneous flap remains the gold standard for the reconstruction of complex mandible defects.
In our experience, we realized the importance of the 3D model, especially in surgical preparation, and the surgical time for flap osteotomy was shortened.
We believe that three-dimensional printing is an essential weapon in reconstructive surgery and should be used in complex cases intraoperatively and as a surgical planning and discussion tool.
It is crucial the interaction of medical professionals and industry to popularize and develop this type of product to bring gains to patients.
REFERENCES
1. Busuito MJ, Smith Junior DJ, Robson MC. Mandibular fractures in an urban trauma center. J Trauma. 1986 Sep;26(9):826-9.
2. Neligan PC. Plastic surgery: craniofacial, head and neck surgery and pediatric plastic surgery. Amsterdam: Elsevier; 2013.
3. Zachariades N, Papademetriou I, Rallis G. Mandibular fractures treated by bone plating and intraosseous wiring. Rev Stomatol Chir Maxillofac. 1994;95(5):386-90.
4. Pellini R, Mercante G, Spriano G. Step-by-step mandibular reconstruction with free fibula flap modelling. Acta Otorhinolaryngol Ital. 2012 Dez;32(6):405-9.
5. Mehta RP, Deschler DG. Mandibular reconstruction in 2004: an analysis of different techniques. Curr Opin Otolaryngol Head Neck Surg. 2004 Ago;12(4):288-93.
6. Pereira MD, Marques AF, Brenda E, Castro M. Immediate reconstruction of the central segment of the mandible using the masseter osteomuscular flap. Plast Reconstr Surg. 1997 May;99(6):1749-54.
7. Jacek B, Maciej P, Tomasz P, Agata B, Kuczko W, Radoslaw W, et al. 3D printed models in mandibular reconstruction with free bone flaps. J Mater Sci Mater Med. 2018;29(3):23.
8. Braga-Silva J, Martins PDE, Román JA, Gehlen D. Reconstrução do segmento ósseo mandibular: comportamento dos implantes ósseo-integrados nos retalhos vascularizados de crista ilíaca e fíbula. Rev Bras Cir Plást. 2005;20(3):176-81.
9. Portinho PC, Jungblut CF, Bonilha LZ, Berteli JR, Collares MVM. Reconstrução microcirúrgica de mandíbula com retalho livre de fíbula. Rev AMRIGS. 2015 Jan/Mar;59(1):39-54.
10. Merick AF, Shaverien MV, Hanasono MM, Yu P, Largo RD, Villa MT, et al. Using a second free fibula osteocutaneous flap after repeated mandibulectomy is associated with low complicantion rate and acceptable functional outcomes. Plast Reconstr Surg. 2017 Aug;140(2):381-9.
1. Hospital Risoleta Tolentino Neves, Plastic
Surgery, Belo Horizonte, MG, Brazil.
ACM Conception and design study, Conceptualization, Final manuscript approval, Methodology, Project Administration, Realization of operations and/or trials, Resources, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
BMF Conception and design study, Data Curation, Project Administration, Realization of operations and/or trials, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
CTF Realization of operations and/or trials, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
GAC Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing
WOC Conception and design study, Project Administration, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
MMC Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Funding Acquisition, Methodology, Project Administration, Realization of operations and/or trials, Resources, Writing - Original Draft Preparation, Writing - Review & Editing
DRFD Final manuscript approval, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing
LGB Investigation, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing
Corresponding author: Marcelo Martins Casagrande, Rua Herculano de Freitas, 905 , Apto 1402, Independência, Ribeirão Preto, SP, Brazil. Zip Code: 14076-300. E-mail: marcelocasagrande1@gmail.com
Article received: July 04, 2019.
Article accepted: October 21, 2019.
Conflicts of interest: none













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter