

Original Article - Year 2021 - Volume 36 - Issue 1
Epidemiological study of patients treated at the outpatient clinic of the Burn Treatment Center of the Hospital Municipal do Tatuapé between January 2019 and January 2020
Estudo epidemiológico dos pacientes atendidos no ambulatório do Centro de Tratamento de Queimaduras do Hospital Municipal do Tatuapé entre janeiro de 2019 e janeiro de 2020
ABSTRACT
Introduction: Burns are in fourth place as the most common type of trauma globally, generating a challenge due to the severity of patients' injuries. This study investigates the epidemiological profile of patients treated at the Burn Treatment Center (BTC) outpatient clinic of the Hospital Municipal do Tatuapé (HMT/SP).
Methods: Data obtained from the outpatient records of the BTC outpatient clinic of the HMT/SP were analyzed from January 2019 to January 2020, using the following variables: gender, age, causal agent, burn extension, and affected region.
Results: Higher predominance of burns in males (55.3%). There was a higher percentage in the population between 21 and 30 years (15.9%), followed closely by children under 10 years of age (15.8%). The leading causative agent was scalded/heated liquids (56.8%); followed by contact burn (14.7%), the vast majority of patients were affected by medium-sized burn (90.1%), i.e., between 11 and 20% of the burned body surface and the thorax/abdomen the most affected region.
Conclusion: The epidemiological profile demonstrated in this study was compatible, in most data, with the profile found in other centers specialized in treating burns.
Keywords: Burns; Burn units; Epidemiology; Outpatients; Epidemiological studies.
RESUMO
Introdução: As queimaduras encontram-se em quarto lugar como o tipo de trauma mais comum do mundo, gerando um desafio pela gravidade das lesões apresentadas pelos pacientes. Este estudo tem como objetivo rastrear o perfil epidemiológico de pacientes atendidos no ambulatório do Centro de Tratamento de Queimaduras (CTQ) do Hospital Municipal do Tatuapé (HMT/SP).
Métodos: Foram analisados os dados obtidos a partir das fichas de atendimento do ambulatório do CTQ do HMT/SP, no período de janeiro de 2019 a janeiro de 2020, utilizando as seguintes variáveis: sexo, idade, agente causal, extensão da queimadura e região acometida.
Resultados: Maior predomínio de queimadura no sexo masculino (55,3%). Houve porcentagem maior na população entre 21 a 30 anos (15,9%), seguidos de perto pelos menores de 10 anos (15,8%). O principal agente causador foi escaldo/líquidos aquecidos (56,8%); seguido de queimadura por contato (14,7%), a grande maioria dos pacientes foram acometidos por queimadura de médio porte (90,1%), ou seja, entre 11 e 20% de superfície corpórea queimada e o tórax/abdome a região mais acometida.
Conclusão: O perfil epidemiológico demonstrado nesse estudo, mostrou-se compatível, na maioria dos dados, com o perfil encontrado em outros centros especializados em tratamento de queimados.
Palavras-chave: Queimaduras; Unidades de queimados; Epidemiologia; Pacientes ambulatoriais; Estudos epidemiológicos.
INTRODUCTION
Burns are defined as skin lesions caused by an external agent, with the partial or total destruction of the same, to a certain extent of the body surface, due to thermal, electrical, chemical, or radioactive trauma1.
They are fourth as the most common type of trauma in the world. They are among the main external causes of death recorded in Brazil, second only to other violent causes, including traffic accidents and homicides2.
According to WHO data, burns are a global public health problem, causing about 180,000 deaths a year, mostly in low- and middle-income countries and nearly two-thirds in African and Asian regions( 3).
According to the Sociedade Brasileira de Queimaduras, there are 1 million cases of burns per year in Brazil, of which 200,000 are treated in emergency services and, of these, 40,000 require hospitalization. There are 57 burn therapy units (BTUs) registered throughout the national territory( 4).
In the municipality of São Paulo, with about 20 million inhabitants, there are six BTUs in public hospitals accredited to the Sociedade Brasileira de Queimaduras (SBQ), for an estimated local annual incidence of ten thousand new cases per year( 4).
The burns treatment is a challenge due to the severity of patients’ lesions and many complications that this type of trauma can trigger². Epidemiology is essential since it acts directly in the creation of public policies, as it provides elements for evaluation and contributes to the formation of treatment programs and prevention campaigns, besides helping to understand the causation factors; there is still a lack of epidemiological studies in our country that addresses this subject4.
In September 1975, the Hospital do Tatuapé had the first Burn Treatment Center in the municipality, inaugurated with 42 beds. The Burn Treatment Center of the Hospital Municipal Dr. Cármino Caricchio (Tatuapé) covers a physical area of 1,000 square meters exclusive for the care of burn-victim patients. It has an occupational therapist, physiotherapist, psychologist, social worker, and the medical and nursing team. It is a hospital inside the hospital because it has an emergency room, outpatient clinic, surgical center, ICU, post-anesthetic recovery, and ward on a single floor. It is a reference for the municipality of São Paulo, neighboring municipalities, and states. Currently, it has 22 infirmary beds and four ICU beds.
OBJECTIVES
The purpose of this study is to trace the epidemiological profile of patients treated at the outpatient clinic of the Burn Treatment Center of the Hospital Municipal do Tatuapé from January 2019 to January 2020.
METHODS
A descriptive observational epidemiological study was carried out to determine the distribution of individuals who are victims of burns according to the causative agent, individuals’ characteristics, and burns, totaling 1,844 new patients seen at the outpatient clinic during the period studied.
Data obtained from the outpatient records of the Burn Treatment Center of the Hospital Municipal do Tatuapé from January 2019 to January 2020 were analyzed. We excluded from this study patients admitted to the outpatient clinic before the beginning of the studied period and hospitalized patients. The collected data are recorded and stored in the attendance control registry and are subsequently sent to the municipal, state, and health departments and will be part of DATASUS.
In this study, aspects related to age, gender, burn causes, burn extension, and affected region were considered. Regarding the age group, the following data were divided into: (1) between 00-10 years, (2) 11-20 years, (3) 21-30 years, (4) 31-40 years, (5) 41-50 years and (6) 51-60 years and over 61 years. The burns’ causative agents were divided into physical, chemical, and biological, and from there subdivided into flammable liquids, heated/scalded liquids, heated solids, chemistry, fire/heat, radiation, electricity, and others.
The extent of the burn on the burned body surface (BBS) was based, which is calculated by the Lund-Browder scheme. At work, we considered second and third-degree burns and was divided into three categories: (1) small burned (up to 5% in less than 12 years or 10% of BBS in those over 12 years), (2) medium burned (5-15% of BBS in children under 12 years or 10-20% of BBS in those over 12 years of age) and (3) large burned (greater than 15% of BBS in children under 12 years of age and greater than 20% of BBS over 12 years of age or burn of more than 5% in children under 12 years of age or 10% in those over 12 years of age).
The project was forwarded to the Hospital Municipal Dr. Cármino Caricchio’s research ethics committee under protocol number: 334402203 00000073.
RESULTS
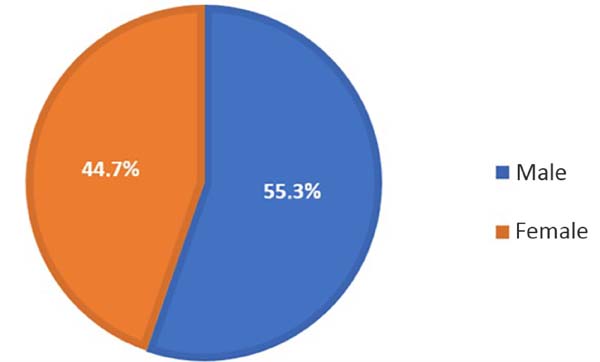
Regarding gender, there was a higher predominance of males (55.3%), over females (44.7%), in a ratio of 1.24:1 (Figure 1).
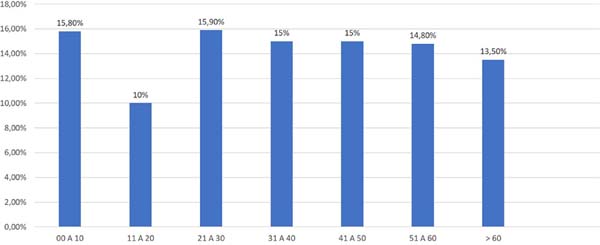
Regarding the age group, despite the very egalitarian distribution, we observed a higher concentration of burns in the age group between 21 and 30 years (15.9%), followed closely by patients between 00 and 10 years (15.8%), then we have tied patients between 31-40 years and 41-50 years, both of which make up about 15% of the cases. The age group with fewer cases was between 11 and 20 years, only 10% of the total. The mean age was 35.27 (Figure 2).
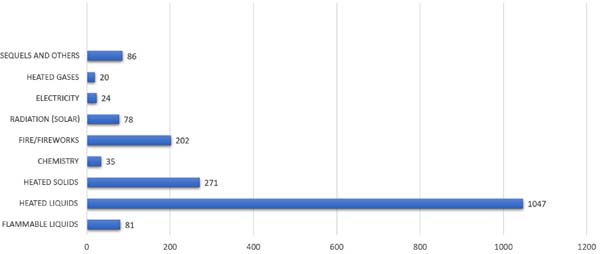
Regarding the burn’s causative agent, we have the heated/scalded liquids being the main one, with about 56.8%, followed by contact burn (14.7%). Next, the exposure of data related to the etiological agents responsible for burns (Figure 3).
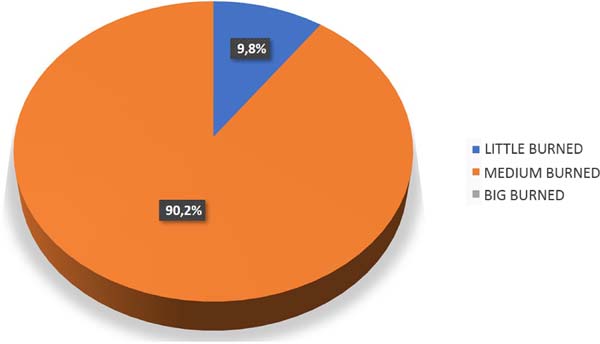
Regarding the burned area extent, it was found that 9.9% of the patients had minor burns (less than 10% of BBS), and 90.1% of the victims were considered to have medium-sized burns (between 11 and 25% of BBS). No patient had a large burn, as they were hospitalized (16% of the emergencies) and, in this study, we considered only the patients seen in the outpatient clinic (Figure 4).
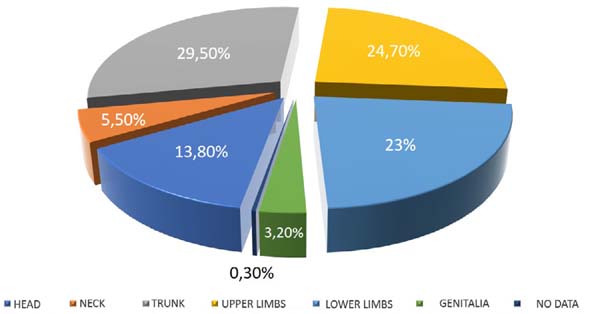
Finally, according to the affected region, we saw that the most affected area was the trunk, including the abdomen with 29.5%, followed by upper limbs (24.7%), lower limbs (23%), head (13.8%), neck (5.5%) and genitalia (3.2%). In the other 0.3%, there was no access to the data (Figure 5).
DISCUSSION
Burns can result in severe deformities, limiting deficiencies, and adverse psychological reactions with social repercussions, which affect patients and their families. The epidemiology of these lesions varies from one part of the world to another over a given time and is related to cultural practices, social crises, and individual circumstances5.
In this study, the highest incidence of burns occurred in males, data compatible with other national and international studies regarding the prevalence of burns among males6-8.
There was an increase in outpatient care after the new year, mainly caused by fireworks.
The most affected age group corresponds to 21-30 years (15.9%), data similar to other studies( 7,9,10, )proving the economic impact that this trauma has because they are the ones that concentrate the most significant productive labor force, that is, the economically active population. Next, with the number of cases very close to the most incident, we have patients under ten years of age (15.8%). In most cases, it was observed that accidents occurred at home and with heated liquid causing agents, a fact that can be explained by the vulnerability of the victims linked to the fact of the precarious living conditions. Costa et al., in 1999(11, )affirm in their study that the poor conditions of household items, in which the stove replaces the stove, favors the accident. The child, curious and impelled to exercise his natural right to explore the environment, is the primary victim in this dramatic social marginality situation. It is worth highlighting the burns incidence in the elderly group (13.5%), who need special attention, due to the differentiated conditions of these patients, exposing them to the higher risk of this trauma, and
We have the scalding or burn by overheated liquids as the leading cause (56%). Suppose there is an agreement with the literature with some studies, such as Silva et al., in 201913, which point out the primary aggressor agent for the patients studied, with an expressive number of 55.77% of people, being by scalding liquids, including water, oil, milk, coffee and tea at high temperatures. However, there was a divergence of Leitão et al., in 20147, who observed that most of the injuries were caused by fire (58.5%), followed by scalding by hot liquids (19.5%); and, Lacerda et al., in 20109, being the main agents causing burning the flammable liquid with 41 patients (40.6%) and the heated fluid with 26 patients (25.7%). Alcohol was the principal causative agent of an accident, classified as a flammable liquid, and represented 31.3% of all cases9.
In the present study, we had a particularity, bringing the contact burn as the second with the highest service incidence (14.6%). However, the world literature places heat/fire as the first agent, followed by scalding and contact injuries with heated solids14-16.
Regarding the extent of the burned area, we observed that the vast majority (90.2%) had between 10-20% of the body surface burned, medium burned, as it is not compatible with the study by Lacerda et al., in 20109. In this study, there was a predominance of minor burns in 62 cases (61.4%), and 27 (26.7%) and 12 (11.9%) classified, respectively, as medium and major burns. This can be attributed to the fact that this study did not cover patients who underwent hospitalization, the vast majority of whom were severely burned, but only those treated at the BTC outpatient clinic of the Hospital Municipal Hospital do Tatuapé. Soares et al., In 201617, demonstrated that the patient with SCQ> 20% represented 48.21% of the cases surveyed, with a mean burned area of 15% and a higher prevalence of SCQ <10%.
Considering the region affected by the burn, the trunk had the highest incidence, followed by upper limbs and lower limbs. This differs from Soares et al., in 201617, which showed that the majority (72.3%, n=81) presented burns in more than one body area, with higher prevalence in the upper limbs (70.5%, n=79), followed by the head region (46.4%, n=52) and burns in the lower limbs (45.5%, n=51), which can be explained by the fact that in our study, there was no separation between the thorax and abdomen at the time of data collection, thus making up about 29.5%.
CONCLUSION
The epidemiological profile demonstrated in this study for visits to the Burn Treatment Center outpatient clinic of the Hospital Municipal do Tatuapé, proved to be compatible, in most data, with the profile found in other centers specialized in the treatment of burns, with some divergences, because the study is only intended for outpatient care. There was a higher incidence of burn in males, in the age range of 00 to 10 years and 21 to 30 years; with scalding as the leading causative agent, the body surface between 10 and 20% the most affected and the chest/abdomen the most affected region.
REFERENCES
1. Dias LDF, Oliveira AF, Juliano Y, Ferreira LM. Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo: estudo epidemiológico. Rev Bras Cir Plást. 2015;30(1):86-92.
2. Vale ECS. Primeiro atendimento em queimaduras: a abordagem do dermatologista. An Bras Dermatol. 2005;80(1):9-19.
3. World Health Organization (WHO). Burns fact sheet [Internet]. Genebra: WHO; 2018. Disponível em: https://www.who.int/es/news-room/fact-sheets/detail/burns
4. Cruz BF, Cordovil PBL, Batista KNM. Perfil epidemiológico de pacientes que sofreram queimaduras no Brasil: revisão de literatura. Rev Bras Queimaduras. 2012;11(4):246-50.
5. Asuquo ME, Ekpo R, Ngim O, Agbor C. A prospective study of burn trauma in adults at the University of Calabar Teaching Hospital, Calabar (South Eastern Nigeria). Eplasty. 2008 Jul;8:e36.
6. Bessa DF, Ribeiro AL, Barros SE, Mendonça MC, Bessa IF, Alves MA, et al. Perfil epidemiológico dos pacientes queimados no Hospital Regional de Urgência e Emergência de Campina Grande, PB, Brasil. Rev Bras Ciência Saúde. 2006 Jul;10(1):73-80.
7. Leitão EPC, Gomes HFC, Silva VAT, Santana RV. Estudo epidemiológico de pacientes internados na unidade de tratamento de queimados do Hospital Geral de Vila Penteado - São Paulo. Rev Bras Cir Plást. 2014;29(2):264-8.
8. Greco Junior JB, Moscozo MVA, Lopes Filho AL, Menezes CMGG, Tavares FMO, Oliveira GM, et al. Tratamento de pacientes queimados internados em hospital geral. Rev Soc Bras Cir Plást. 2007;22(4):228-32.
9. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. Rev Bras Queimaduras. 2010;9(3):82-8.
10. Miranda RE, Pacannaro RC, Pinheiro LF, Calil JA, Gragnani A, Ferreira LM. Trauma elétrico: análise de 5 anos. Rev Bras Queimaduras. 2009;8(2):65-9.
11. Costa DM, Abrantes MM, Lamounie JA, Lemos ATO. Estudo descritivo de queimaduras em crianças e adolescentes. J Pediatr (Rio J). 1999;75(3):181-6.
12. Serra MCVF, Sasaki AL, Cruz PFS, Santos AR, Paradela EMP, Macieira L. Perfil epidemiológico de idosos vítimas de queimaduras do Centro de Tratamento de Queimados Dr. Oscar Plaisant do Hospital Federal do Andaraí - Rio de Janeiro-RJ. Rev Bras Queimaduras. 2014;13(2):90-4.
13. Silva TBL, Oliveira CM, Felisberto D, Nigro MVAS, Kusano LDC, Mialski JR. Caracterização epidemiológica de pacientes queimados atendidos no Serviço de Queimados do Hospital Universitário Evangélico Mackenzie de Curitiba no ano de 2017. Rev Bras Cir Plást. 2019;34:70-2.
14. Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Crit Care. 2010;14(5):R188.
15. Oladele AO, Olabanji JK. Burns in Nigeria: a review. Ann Burns Fire Disasters. 2010 Sep;23(3):120-7.
16. Garg AK, Uppal S, Garg R, Gupta A, Pal R. A clinico-epidemiologic study of 892 patients with burn injuries at a tertiary care hospital in Punjab, India. J Emerg Trauma Shock. 2011 Jan/Mar;4(1):7-11.
17. Soares LR, Barbosa FS, Santos LA, Mattos VCR, Paula CA, Leal PML, et al. Estudo epidemiológico de vítimas de queimaduras internadas em um hospital de urgência da Bahia. Rev Bras Queimaduras. 2016;15(3):148-52.
1. Hospital do Servidor Público Municipal de São
Paulo, São Paulo, SP, Brazil.
2. Brazilian Society of Plastic Surgery, São
Paulo, SP, Brazil.
3. Hospital Municipal do Tatuapé, São Paulo, SP,
Brazil.
4. Hospital Municipal Professor Dr. Alípio Correia
Netto, São Paulo, SP, Brazil.
5. Hospital Municipal de Urgências de Guarulhos,
Guarulhos, SP, Brazil.
Corresponding author: Maycon Lucas Barbosa Rua José Getúlio, 109, Liberdade, São Paulo, SP, Brazil. Zip Code: 01509-001 E-mail: mayconlucasb1@gmail.com
Article received: May 20, 2020.
Article accepted: January 10, 2021.
Conflicts of interest: none







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter