

Case Report - Year 2020 - Volume 35 -
Augmentation mammoplasty and mastopexy with somersault flap from reverse abdominoplasty
Mamoplastia de aumento e mastopexia com retalho em cambalhota a partir de abdominoplastia reversa
ABSTRACT
Introduction: The breasts and abdomen undergo significant
morphological changes with massive weight loss. Breast
augmentation is one of the most commonly performed
procedures in plastic surgery, unlike reverse abdominoplasty,
which has been little described. However, in patients with
upper abdominal flaccidity who want breast augmentation,
breast augmentation through reverse abdominoplasty
(AMBRA) makes it possible to improve the breasts and
abdominal contour simultaneously. This work aims to
describe a case of breast augmentation and mastopexy using
a somersault flap from reverse abdominoplasty.
Case Report: Female patient, brown, with a history of massive weight loss
and previous mammoplasty and abdominoplasty, evolved
with breast ptosis and lipodystrophy in the upper abdomen.
She underwent reverse abdominoplasty using an epigastric
dermofat flap for breast projection. The patient had a good
postoperative evolution, with satisfactory surgical results.
Discussion: Massive weight loss can result in deformities
in the breasts and abdomen that require reparative surgery.
Breast remodeling is arduous and may require the use
of adjacent tissues. Abdominoplasty, in turn, is the most
established technique for rejuvenating the trunk; however,
when sagging mainly affects the upper abdomen, reverse
abdominoplasty becomes an option. In cases where the
desire for breast augmentation is associated with excess
supraumbilical volume, AMBRA should be considered. Breast
augmentation using reverse abdominoplasty proved to be a
viable technique in this case, with a satisfactory final result.
Keywords: Breast; Abdomen; Weight loss; Mammoplasty; Abdominoplasty.
RESUMO
Introdução: As mamas e o abdômen passam por grandes modificações morfológicas com perdas ponderais maciças. A mamoplastia de aumento é um dos procedimentos mais realizados na cirurgia plástica, ao contrário da abdominoplastia reversa, pouco descrita. Porém, em pacientes com flacidez abdominal superior que desejam o aumento mamário, a mamoplastia de aumento por meio da abdominoplastia reversa (AMBRA) torna possível o aprimoramento das mamas e do contorno abdominal simultaneamente. O objetivo deste trabalho é descrever um caso de mamoplastia de aumento e mastopexia utilizando retalho em cambalhota a partir de abdominoplastia reversa.
Relato de Caso: Paciente do sexo feminino, parda, com história de perda ponderal maciça e com mamoplastia redutora e abdominoplastia prévias, evoluiu com ptose mamária e lipodistrofia em abdômen superior. Foi submetida à abdominoplastia reversa com utilização do retalho dermogorduroso epigástrico para projeção da mama. A paciente apresentou boa evolução pós-operatória, com resultado cirúrgico satisfatório.
Discussão: As perdas ponderais maciças podem resultar em deformidades nas mamas e no abdômen que exigem cirurgias reparadoras. A remodelação mamária é difícil e pode exigir a utilização de tecidos adjacentes. A abdominoplastia, por sua vez, é a técnica mais consagrada para o rejuvenescimento do tronco; entretanto, quando a flacidez atinge principalmente o abdômen superior, a abdominoplastia reversa torna-se uma opção. Em casos em que o desejo de mamoplastia de aumento se associa ao excesso de volume supraumbilical, deve-se considerar a AMBRA. A mamoplastia de aumento por meio da abdominoplastia reversa revelou ser uma técnica viável neste caso, com resultado final satisfatório.
Palavras-chave: Mama; Abdome; Perda de peso; Mamoplastia; Abdominoplastia
INTRODUCTION
The breasts and abdomen undergo significant morphological changes with weight variations1. In massive weight loss, abdominal lipodystrophy is accompanied by a small breast volume, associated or not with ptosis2.
Breast augmentation with or without mastopexy occupies an important position as one of the most performed plastic surgery procedures. The breast implant is still the most straightforward and safest method to improve the shape and size of the breasts3,4 However, complications such as capsular contracture, undulations, palpability, rupture of the prosthesis, and loss of local sensation make augmentation with autologous tissue a viable alternative3-6.
In contrast, reverse abdominoplasty has been poorly described in the literature, mainly due to the small number of patients who benefit from it and the scar’s non-acceptance on the upper abdomen3. However, when excess skin and residual fat are located, especially in the epigastric region, it becomes a great alternative, given that in this situation, classic abdominoplasty techniques are not always effective7.
In patients with upper abdominal flaccidity who desire breast augmentation, augmentation mammaplasty employing reverse abdominoplasty (AMBRA) stands out. It is a technique that uses the dermofat flaps of the abdomen as a breast implant, addressing both regions simultaneously3.
This work aims to report a case of breast augmentation and mastopexy from a dermofat flap in somersault from reverse abdominoplasty.
CASE REPORT
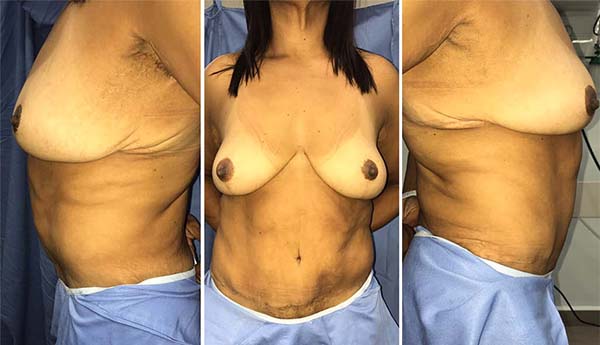
Female patient, 47 years old, brown, with a history of morbid obesity (BMI 53.15 kg/m2) and weight loss of 59 kg in 6 years, evolved in the late postoperative period of abdominoplasty and reduction mammoplasty with previous breast ptosis and lipodystrophy in the epigastric region. As for comorbidities, he reported only systemic arterial hypertension in treatment and denied smoking. On physical examination, a patient weighing 59kg, 1.49m, and a BMI of 26.58kg/m2. The breasts contained an inverted T scar and were not very bulky, mainly in the upper pole, ptosed, and with fatty substitution, classified as Regnault grade II (Figure 1). The abdomen had a lower horizontal scar, with an increased volume of the supraumbilical region (Figure 1). For the simultaneous correction of breast ptosis and epigastric lipodystrophy, we opted for breast augmentation and mastopexy with a somersault flap from reverse abdominoplasty.
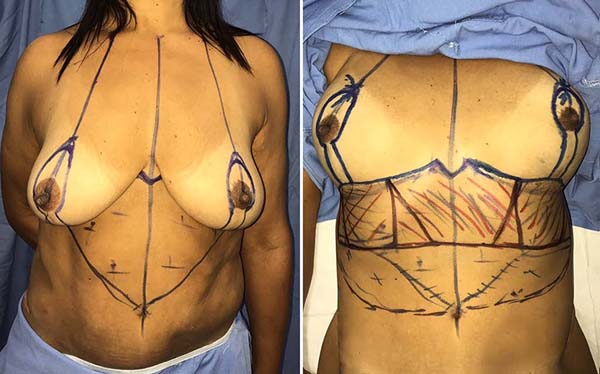
With the patient in an orthostatic position, the surgical demarcation was performed (Figure 2). Certain midline starting at the wishbone, passing through the xiphoid process, and ending at the umbilical scar. Point A was identified through a bidigital maneuver as a projection of the inframammary fold on the breast’s upper pole, also coinciding with the humeral midline. From point A, marking was drawn with a distance equal to the areolar diameter, to the lower border of the nipple-areola complex (NAC), and, from there, a spindle encompassing the previous scar. Inframammary grooves were marked, with a scar-breaking line in the median region, with a distance of 8 cm on each side predetermined from the midline to meet the mastopexy scar. A line was drawn parallel to the grooves in the upper abdomen identified by clamping, the lateral limits being the anterior axillary lines.
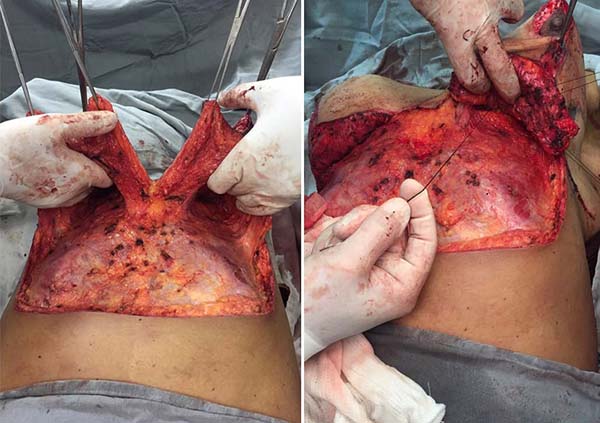
The patient was in a supine position under general and epidural anesthesia. An incision was made on the previous markings, followed by periareolar and abdominal de-epithelialization (Figure 3). After detachment and the median section of the dermofat flaps from the upper abdomen (Figure 3), subglandular pockets were made in the breasts (Figure 4). The flaps were repaired and, after somersault rotation, fixed on the fascia of the pectoralis major muscle, at the height of the 3rd costal arch (Figure 4). Craniocaudal detachment was performed from the abdomen to the umbilical scar. To reduce dead space and closure tension, it was decided to perform Baroudi stitches in the entire dissected area, up to the 6th costal arch’s periosteum, to form the new inframammary fold (Figure 5). Completion of assembly and symmetrization of the breasts, with the positioning of the NAC (Figure 5). It was closed by planes (Figure 6). The dressing was made with sterile gauze and micropore.
The patient did not have any complications and was discharged on the 1st postoperative day. The surgical wound was in good shape, with no signs of inflammation or other complications. The patient returned for outpatient follow-up with no seroma, hematoma, dehiscence, epitheliosis, or flap necrosis (Figures 6, 7, and 8)
DISCUSSION
During weight gain, anatomical changes in soft tissues and fat deposition pattern are determined by the patient’s sex, age, caloric intake, physical activity, and genetic predisposition. Likewise, changes in body shape and contour that occur after massive weight loss are also influenced by these factors and the weight lost2. With these consequent functional and aesthetic deformities, the number of surgeries that aim to repair them has been increasing, requiring the expertise of plastic surgeons6.
After large weight losses, the breasts lose shape, projection, and elasticity8. Due to significant ptosis and redundant skin secondary to fat atrophy after an obesity-expanding effect, isolated mastopexy has not always been satisfactory, requiring a simultaneous increase6. This breast remodeling is arduous and may require the use of adjacent tissues8. In the 1950s, Longacre described a breast augmentation and reconstruction technique using dermofat flaps with an upper pedicle folded under themselves in a somersault and fixed on the pectoral fascia9-11.
In turn, the abdomen is one of the regions that most show variations with weight loss, and resolving acquired deformities is not always easy12. Conventional abdominoplasty is the most established technique for rejuvenating the trunk; however, when flaccidity mainly affects the upper abdomen, reverse abdominoplasty becomes an option3. It was first described in 1972 by Rebello and Franco13. In 1979, Baroudi et al.1 associated the technique to reduce mammoplasty and emphasized the importance of fixing the breasts and abdomen’s flaps to the new mammary fold. Subsequently, in 2009, Deos et al.12 proposed tensioned reverse abdominoplasty, with the traction of the flap and its fixation to the abdominal aponeurosis, thus allowing an improvement in the quality of the scar as it is tension-free and has a decrease in the seroma and necrosis index due to the reduction of dead space. Yacoub et al., In 201214, published the extended reverse abdominoplasty, with wide dissection up to the pubis and allowing the combination with other surgeries. After, in 2014, Saldanha et al.15 detailed the use of the remaining flap from reverse abdominoplasty for breast reconstructions.
In cases where the desire for breast augmentation is associated with excess supraumbilical volume, breast augmentation through reverse abdominoplasty (AMBRA) should be considered. She uses excess flaps from the abdomen as breast implants. They are de-epithelialized, folded, and positioned in the breasts’ subglandular plane, remaining attached to their upper vascular pedicles. Because of the procedures’ combination, the scar, although extensive, is not an impediment factor. Besides, since the tissue is autologous, the result is more natural, and there is no risk of capsular contracture or loss of sensation3.
CONCLUSION
Reverse abdominoplasty has received little attention in the medical literature, which is the opposite of breast augmentation, which is one of the most performed plastic surgeons’ interventions today. However, these two techniques can be combined to approach patients with upper abdominal lipodystrophy associated with small isolated breast volume or varying ptosis degrees. Augmentation mammaplasty employing reverse abdominoplasty (augmentation mammaplasty by reverse abdominoplasty - AMBRA) has proved to be a viable and effective procedure, as long as it is well indicated. Despite the resulting extensive scar, the advantages of using autologous tissue as an implant, and the optimal final result stood out.
REFERENCES
1. Baroudi R, Keppke EM, Carvalho CG. Mammary reduction combined with reverse abdominoplasty. Ann Plast Surg. 1979 Mai;2(5):368-73.
2. Agha-Mohammadi S, Hurwitz DJ. Management of upper abdominal laxity after massive weight loss: reverse abdominoplasty and inframammary fold reconstruction. Aesthetic Plast Surg. 2010 Abr;34(2):226-31.
3. Zienowicz RJ, Karacaoglu E. Augmentation mammaplasty by reverse abdominoplasty (AMBRA). Plast Reconstr Surg. 2009 Nov;124(5):1662-72.
4. Lai YL, Yu YL, Centeno RF, Weng CJ. Breast augmentation with bilateral deepithelialized TRAM flaps: an alternative approach to breast augmentation with autologous tissue. Plast Reconstr Surg. 2003 Jul;112(1):302-8;discussion:309-11.
5. Van Landuyt K, Hamdi M, Blondeel P, Monstrey S. Autologous breast augmentation by pedicled perforator flaps. Ann Plast Surg. 2004 Out;53(4):322-7.
6. Kwei S, Borud LJ, Lee BT. Mastopexy with autologous augmentation after massive weight loss: the intercostal artery perforator (ICAP) flap. Ann Plast Surg. 2006 Out;57(4):361-5.
7. Flores LRP, Oliveira Junior FC, Zampar AG, Mélega JM. Cirurgia pós-bariátrica do tronco superior: abdominoplastia em "Y". Rev Bras Cir Plást. 2010 Set;25(3):540-6.
8. Hurwitz DJ, Agha-Mohammadi S. Postbariatric surgery breast reshaping: the spiral flap. Ann Plast Surg. 2006 May;56(5):481-6.
9. Longacre JJ. Correction of the hypoplastic breast with special reference to reconstruction of the "nipple type breast" with local dermo-fat pedicle flaps. Plast Reconstr Surg (1946). 1954 Dez;14(6):431-41.
10. Longacre JJ, Destefano GA, Holmstrand K. Breast reconstruction with local derma and fat pedicle flaps. Plast Reconstr Surg Transplant Bull. 1959 Dez;24:563-76.
11. Vieira LFDF, Almeida CLA. Mastopexia a Longacre modificada. Rev Bras Cir Plást. 2012 Jan/Mar;27(1):67-72.
12. Deos MF, Arnt RA, Gus EI. Tensioned reverse abdominoplasty. Plast Reconstr Surg. 2009 Dez;124(6):2134-41.
13. Rebello C, Franco T. Abdominoplastia por incisão submamária. Rev Bras Cir. 1972;62:249-52.
14. Yacoub CD, Baroudi R, Yacoub MB. Abdominoplastia reversa estendida. Rev Bras Cir Plást. 2012 Abr/Jun;27(2):328-32.
15. Saldanha OR, Urdaneta FV, Llaverias F, Saldanha Filho OR, Saldanha CB. Reconstrução de mama com retalho excedente de abdominoplastia reversa. Rev Bras Cir Plást. 2014;29(2):297-302.
1. Irmandade da Santa Casa da Misericórdia de Santos, Service of Plastic Surgery and
Burns, Santos, SP, Brazil.
GCVFS Conception and design study, Writing - Original Draft Preparation, Writing - Review & Editing
CMM Conception and design study, Writing - Original Draft Preparation, Writing - Review & Editing
DNDA Conception and design study, Writing - Review & Editing
Corresponding author: Giovanna Calil Vicente Franco de Souza, Rua Alferes Ângelo Sampaio, 967, Apto 801, Água Verde, Curitiba, PR, Brazil. Zip Code: 80250120. E-mail: giovannacvfsouza@hotmail.com
Article received: May 01, 2019.
Article accepted: October 21, 2019.
Conflicts of interest: none
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter