

Case Reports - Year 2020 - Volume 35 -
Nasal reconstruction with paramedian frontal flap after cancer resection
Reconstrução nasal com retalho frontal paramediano após ressecção oncológica
ABSTRACT
Introduction: Basal cell carcinoma is the most frequent type of tumoral lesion of the skin, often affecting the nasal region. The resulting defects require the use of nasal reconstruction techniques. The first plastic surgery described is the nasal reconstruction, according to the Indian method. Over the centuries, it has been the object of several modifications by the biggest names in the specialty, culminating in the paramedian frontal flap.
Case Report: A 62-year-old male patient went to the Plastic Surgery Service of the Federal Hospital of Ipanema, presenting an ulcerated, scaly lesion, occupying the entire lateral region of the nose with three years of evolution, suggesting at physical examination malignant skin tumor. It was performed cutaneous lesion excision and immediate reconstruction with a paramedian frontal flap and further refinement surgery.
Conclusion: Due to its vascularization by the supratrochlear artery and texture similar to the nasal tissue, the paramedian frontal flap is the gold standard for the correction of significant nasal defects.
Keywords: Nasal neoplasms; Reconstruction; Acquired nasal deformities; Reconstructive surgical procedures; Surgical flaps; Case reports.
RESUMO
Introdução: O carcinoma basocelular é o tipo mais frequente de lesão tumoral de pele acometendo frequentemente a região nasal. Os defeitos resultantes exigem o emprego de técnicas de reconstrução nasal. A primeira cirurgia plástica descrita é a reconstrução nasal segundo o método indiano. Ao longo dos séculos sofreu diversas modificações pelos maiores nomes da especialidade, culminando no retalho frontal paramediano.
Relato do Caso: Paciente do sexo masculino, 62 anos, apresentou-se no serviço de Cirurgia Plástica do Hospital Federal de Ipanema com lesão ulcerada, descamativa, ocupando toda a região lateral do nariz com três anos de evolução, sugestiva ao exame físico de tumor maligno de pele. Foi realizada exérese da lesão cutânea e imediata reconstrução com retalho frontal paramediano e posterior cirurgia de refinamento.
Conclusão: Devido à sua vascularização pela artéria supratroclear e textura semelhante ao tecido nasal, o retalho frontal paramediano constitui-se como o gold standard para a correção de grandes defeitos nasais.
Palavras-chave: Neoplasias nasais; Reconstrução; Deformidades adquiridas nasais; Procedimentos cirúrgicos reconstrutivos; Retalhos cirúrgicos; Relatos de casos
INTRODUCTION
The first description of nasal reconstruction was made around 700 B.C in the treatise of Ayurveda medicine called Sushruta Samhita. Although performed since ancient times, the Indian method was only published in the 18th century in the Madras Gazette of Bombay1.
In 1597, Tagliacozzi published a series of works in which he described the reconstruction of the nose using forearm flaps; this became known as the Italian method2.
During the 19th century, Blasius, Dieffenbach, and Petrali expanded the internal coating method in addition to the external one2. Gillies, Converse, Kazanjian, and Millard perfected the method throughout the 20th century, with new flap designs and restoring methods of nasal support. Kazanjian consecrated the median frontal flap in the United States in the 20th century first half3.
In the 80’ and 90’, Burget and Menick3,4, with their principles of nasal aesthetic subunits and the analysis of facial vascularization, established the paramedian frontal flap as the preferred method for nasal reconstruction.
The work’s objective is to illustrate a case of nasal cutaneous tumor exeresis and its immediate reconstruction with a paramedian frontal flap, demonstrating its importance in nasal reconstruction surgery.
CASE REPORT
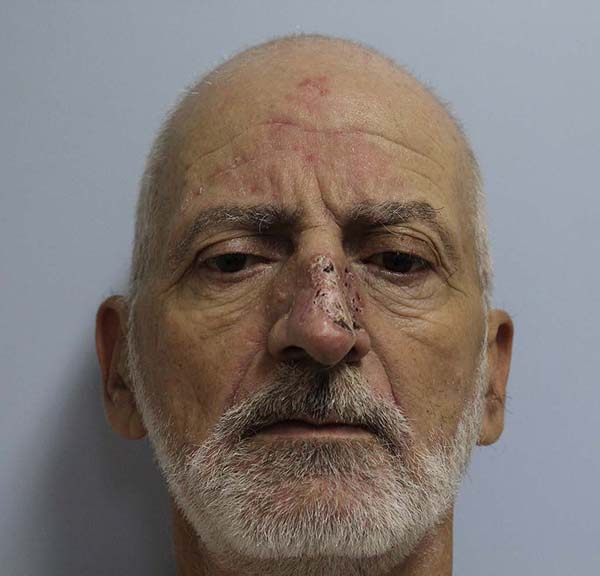
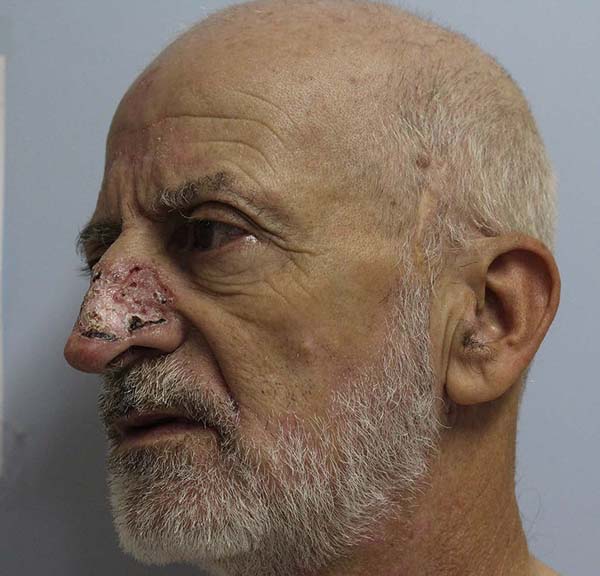
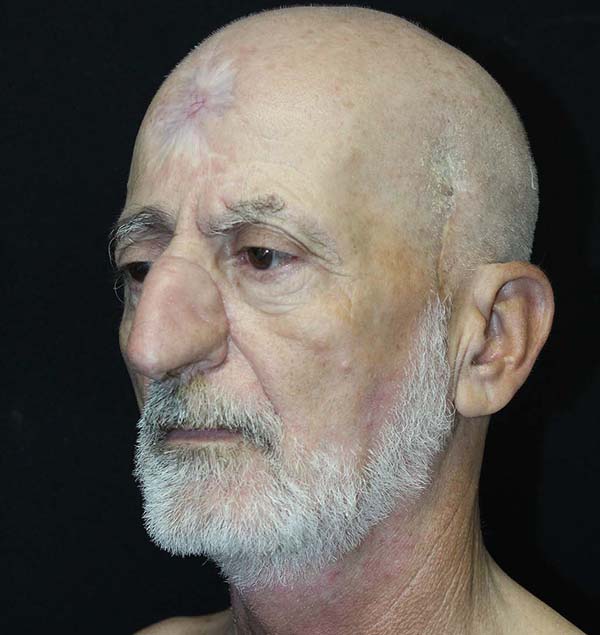
62-year-old male patient with a history of ischemic stroke 40 years ago with sequelae of monoparesis of the right upper limb, with no smoking or drinking habits. He presented an ulcerated, scaly lesion, occupying the entire left lateral region of the nose with three years of evolution, suggesting a malignant skin tumor (Figures 1 and 2).
Under general anesthesia and after due asepsis, the tumor lesion to be excised was marked with a 4 mm safety margin and infiltrated with an anesthetic solution of 1% lidocaine + adrenaline 1: 200,000.
The tumoral lesion was extensively resected, and the piece sent for the intraoperative freezing examination which revealed to be a superficial basal cell carcinoma with free limits.
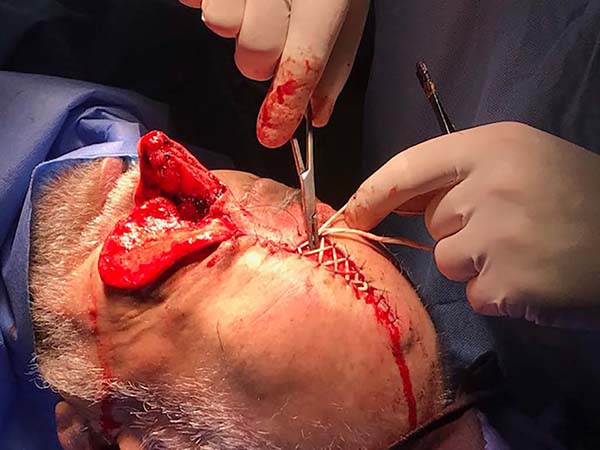
Then, the paramedian frontal flap was marked according to the Gillies3 drawing “up and down” (Figure 3). Resulting defect dimensions were considered and were respected the flap limits described by Menick in 20023: approximately 2 cm lateral to the midline near the eyebrow head and with a pedicle width of approximately 1, 5 cm in the vertical direction. The flap was detached distal-proximally, dissecting initially in the subcutaneous plane and more proximally in the juxtaperiosteal plane.
The flap was rotated, positioned over the defect, refined and sutured to the edges with 5-0 nylon thread. The donor region was sutured in regions eligible for coaptation. An elastic suture was applied in the remainder, leaving the resulting central defect to heal by second intention (Figures 4 and 5).
Four weeks later, the flap pedicle’s transection was performed with the repositioning of the eyebrow head. Finally, the flap was refined with degreasing and rotation of the left nasal wing.
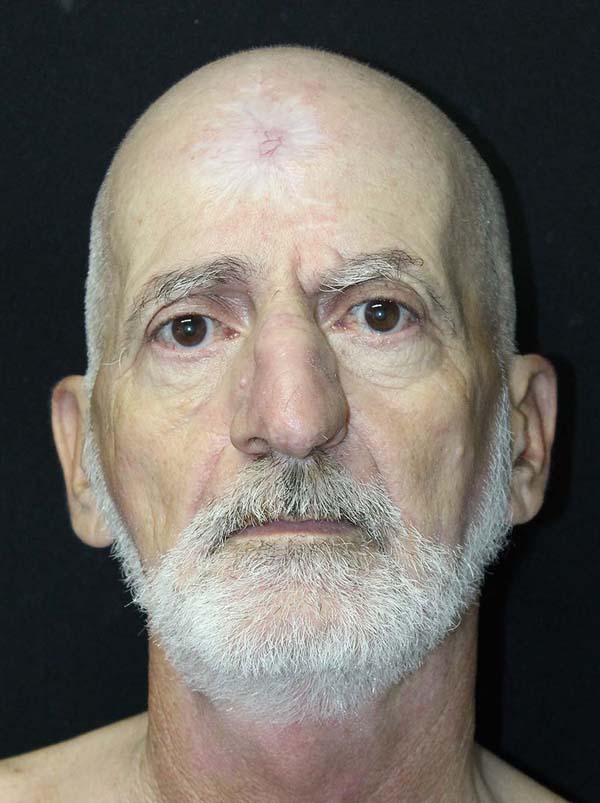
After three months of post-surgery, the patient was clinically well, without functional complaints, although he had highlighted a disturbance regarding the aesthetic result, the donor area was practically healed.
We then opted for nasal refinement surgery, which was performed in the sixth postoperative month. In the subsequent follow-up, at 9 months postoperatively, the patient was satisfied with the functional and aesthetic result (Figures 6 and 7).
DISCUSSION
Basal cell carcinoma is the most common malignant skin tumor in our daily practice.
In the present case, it was a superficial defect, although large (greater than 1.5 cm)5, reaching four of the aesthetic subunits of the nose: lateral wall, wing, back, and nasal tip.
The principle of aesthetic subunits described by Menick, in 20104, advocates that if the subunit is affected in more than 50% of its area, it must be removed entirely, which is particularly useful in the subunits of the lower third of the nose because its curved and prominent lines could result in more apparent scarring. In the present case, this principle was not strictly followed, taking into account the already considerable dimensions of the initial defect and the respect for the surgical safety margin.
Although several techniques can be used, the paramedian frontal flap is particularly safe, reliable, and reproducible. Its vascularization through the supratrochlear artery makes the frontal region skin the most similar in color and texture to that of the nose6,7.
The flap’s design can be presented in different forms, from oblique to a “gull” format by Millard5, passing through the “up and down” by Gillies3. The paramedian frontal flap vascularization is mainly done by the supratrochlear vessels. These pass over the orbital margin externally to the periosteum, follow vertically upwards within the frontalis muscle, and assume a subdermal position next to the capillary line5.
The pedicle is usually sectioned four weeks after the first surgery, configuring the surgery in two stages, being this one the most traditional7. In 2010, Menick4 advocated surgery in three stages, with an intermediate phase of “debulking,” especially indicated in smoking patients, with previous scars or full-thickness defects.
The donor area, with a significant defect, was approached with an elastic suture according to Nigri, in 20118, the remainder being left to heal by second intention, which was not a problem8.
As expected in two-stage surgery, refinement surgery was necessary. In this case, flap degreasing and nasal wing rotation were performed. The patient was satisfied with the aesthetic and functional result, and the refinement process was not continued.
CONCLUSION
The paramedian frontal flap allows the transfer of tissue to the nasal region efficiently and safely with little morbidity in the donor area, allowing a malleable and similar coverage to the nasal tissue with excellent viability.
REFERENCES
1. Cintra HPL, Bouchama A, Holanda T, Jaimovich CA, Pitanguy I. Uso do retalho médio-frontal na reconstrução do nariz. Rev Bras Cir Plást. 2013;28(2):212-7.
2. Baker SR. Principles of nasal reconstruction. Maryland, US: Mosby; 2002.
3. Menick FJ. A 10-year experience in nasal reconstruction with the three-stage forehead flap. Plast Reconstr Surg. 2002 Mai;109(6):1839-55;discussion:1856-61.
4. Menick FJ. Nasal reconstruction. Plast Reconstr Surg. 2010 Abr;125(4):138e-50e.
5. Menick FJ. Nasal reconstruction: forehead flap. Plast Reconstr Surg. 2004;113(6):100e-11e.
6. Quintas RCS, Araújo GP, Medeiros Junior JHGM, Quintas LFFM, Kitamura MAP, Cavalcanti ELF, et al. Reconstrução nasal complexa: opções cirúrgicas numa série de casos. Rev Bras Cir Plást. 2013;28(2):218-22.
7. Costa MJM. Versatilidade do retalho médio-frontal nas reconstruções faciais. Rev Bras Cir Plást. 2016;31(4):474-80.
8. Santos ELN, Oliveira RA. Tratamento de ferida com uso de sutura elástica. Rev Bras Cir Plást. 2014;29(4):587-8.
1. Hospital Federal de Ipanema, Plastic Surgery, Rio de Janeiro, RJ, Brazil.
Corresponding author: Carlos Miguel Pereira Rua Gomes Carneiro, 155, Apart. 1201, 22071-110, Ipanema, RJ, Brazil. Zip Code: 22071-110 E-mail: carlosmppereira@hotmail.com
Article received: May 31, 2019.
Article accepted: July 08, 2019.
Conflicts of interest: none.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter