

Case Reports - Year 2020 - Volume 35 -
Columellar reconstruction with chondrocutaneous graft after injury caused by CPAP
Reconstrução de columela com enxerto condrocutâneo após lesão causada por CPAP
ABSTRACT
Introduction: Continuous positive pressure in the nasal airways (CPAP) is a non-invasive form of ventilation used in premature newborns in intensive care units. However, it can affect the nose of these patients, even evolving with ischemia and columellar necrosis. Several techniques are described to reconstruct the columella, such as skin grafts, composite grafts, local flaps, and free flaps, but the atrial chondrocutaneous graft has stood out. This study aims to describe a case of columella necrosis using CPAP with reconstruction using posterior atrial chondrocutaneous grafting.
Case Report: A brown, female patient, with a history of prematurity and prolonged use of CPAP when she was born due to hyaline membrane syndrome, developed columella necrosis. The patient underwent posterior auricular chondrocutaneous grafting to reconstruct the columella. She presented a satisfactory surgical result, evolving with 100% graft vitality.
Discussion: Columellar necrosis associated with the use of CPAP can be aesthetically and functionally debilitating, and represents a reconstructive challenge. The options for obtaining acceptable results are limited. However, the use of ear grafts is technically straightforward, uses structurally similar donor tissues, does not cause additional scarring on the nose, is performed in a surgical period, and generally has an excellent result. Posterior auricular composite grafting for columellar reconstruction proved safe, with satisfactory aesthetic and functional results and minimal morbidity in the donor area.
Keywords: Acquired nasal deformities; Necrosis; Continuous positive airway pressure; Reconstructive surgical procedures; Autografts
RESUMO
Introdução: A pressão positiva contínua nas vias aéreas nasais (CPAP) é uma forma não invasiva de ventilação utilizada em recém-nascidos prematuros em unidades de terapia intensiva. Porém, ela pode acometer o nariz destes pacientes, evoluindo até mesmo com isquemia e necrose columelar. Diversas técnicas são descritas para reconstruir a columela, como enxertos de pele, enxertos compostos, retalhos locais e retalhos livres; mas o enxerto composto condrocutâneo auricular tem se destacado. O objetivo deste trabalho é descrever um caso de necrose de columela por uso de CPAP com reconstrução utilizando enxertia condrocutânea auricular posterior.
Relato do Caso: Paciente do sexo feminino, parda, com história de prematuridade e uso prolongado de CPAP quando recém-nascida devido à síndrome da membrana hialina, evoluiu com necrose de columela. Foi submetida à enxertia composta condrocutânea auricular posterior para reconstrução da columela. A paciente apresentou resultado cirúrgico satisfatório, evoluindo com 100% de vitalidade do enxerto.
Discussão: A necrose columelar associada ao uso do CPAP pode ser estética e funcionalmente debilitante, e representa um desafio reconstrutivo. As opções para obter resultados aceitáveis são limitadas, porém o uso de enxertos de orelha é tecnicamente simples, utiliza tecidos doadores estruturalmente semelhantes, não provoca cicatrizes adicionais no nariz, é realizado em um tempo cirúrgico e geralmente tem um resultado muito bom. A enxertia composta auricular posterior para reconstrução columelar se mostrou segura, com resultado estético e funcional satisfatório e mínima morbidade da área doadora.
Palavras-chave: Deformidades adquiridas nasais; Necrose; Pressão positiva contínua nas vias aéreas; Procedimentos cirúrgicos reconstrutivos; Autoenxertos
INTRODUCTION
Continuous positive airway pressure (CPAP) is a non-invasive form of ventilation used as a method of respiratory support in premature newborns in intensive care units as an alternative to endotracheal intubation and tracheostomy1-6. However, due to immaturity, the nose of these patients can be easily affected6. Nasal injury is a relatively common consequence secondary to CPAP, with an incidence of around 13.2% to 50% 1,5, and can vary from edema and erythema to columellar laceration and necrosis3,5. Less than 1% of these patients develop irreversible ischemia and necrosis, resulting in a spectrum of nasal disfigurement2.
Patients with functional and/or aesthetic impairment of columella after using CPAP may need intervention2. For columellar reconstruction, size, symmetry, color matching, skin texture, condition of the surrounding tissue, and donor area must be considered7. Several techniques have been described, and they include skin grafts, composite grafts, local flaps, and free flaps7. Among these various procedures, the auricular chondrocutaneous graft is one of the most advantageous methods, as it allows the reconstruction of the structural cartilage together with the skin, in a single surgical time, in addition to the ear being considerably similar in shape, curve, color and texture to the columela1,7.
The objective of this study is to report a case of an atrial chondrocutaneous graft for columellar reconstruction after necrosis using CPAP.
CASE REPORT
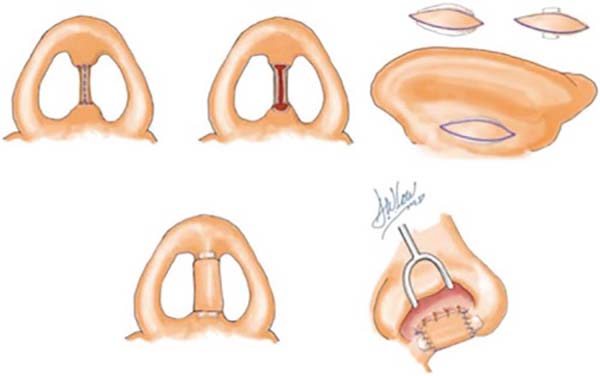
Female patient, 4 years old, brown, with a history of prematurity (gestational age 31 weeks and 4 days) and fetal distress due to placental abruption, developed hyaline membrane syndrome, requiring mechanical ventilation for 16 days and continuous positive pressure in the nasal airways for another 8 days. As a result of using CPAP, he presented a columella lesion with local necrosis. On physical examination, a patient with no columella, with a consequent drop in the tip of the nose (Figure 1). For reconstruction, the posterior atrial chondrocutaneous graft was chosen.
Patient in the supine position under general anesthesia. Surgical demarcation1 (Figure 2) was performed on the columellar defect, with transversal lines at the upper and lower edges, joined by a median vertical line, and the donor area in the posterior region of the left ear with an ellipse (Figure 3). Incision over the ear tag, followed by removal of a composite graft containing skin, subcutaneous tissue, and cartilage. An incision was made over the nasal marking, making two lateral flaps. Graft positioning, with cartilage fitting at the base of the columella, followed by suturing it to the flaps (Figures 4 and 5). Compressive dressing made with gauze.
The patient did not have any complications and was discharged from the hospital on the 1st postoperative day. The surgical wound showed no signs of complication, with a good appearance. The patient returned for outpatient follow-up and the graft was 100% vital (Figure 6). She will remain in follow-up until adolescence, to assess the need for re-approach for aesthetic refinement.
DISCUSSION
Although nursing initiatives have sought to reduce the incidence, nasal injury remains a common problem in preterm newborns who receive non-invasive respiratory support, especially in preterm infants born less than 30 weeks of gestation2,3,5,6. Columellar necrosis associated with CPAP use can be aesthetically and functionally debilitating and represents a reconstructive challenge2. The options for obtaining acceptable functional and cosmetic results are limited in the reconstruction of this delicate subunit, but the use of composite grafts is consistent with many fundamentals of plastic surgery8.
Nasal reconstruction requires the management of several layers simultaneously in a three-dimensional shape7,8. The practice has shown advances since in 19859, surgeons Burget and Menick, proposed the principle of subunits of the nose10. Nasal columella has traditionally been a subunit that is difficult to repair due to its unique contours, limited availability of adjacent skin, and tenuous vascularization10. The simplicity and elegance of using compound ear grafts to repair such defects were already recognized in 18968. The procedure is technically straightforward, uses structurally similar donor tissues, does not cause additional scarring on the nose, performs in a surgical procedure, and usually has a very satisfactory result8.
Posterior auricular composite grafting for columella reconstruction proved safe and had little technical difficulty in repairing the described lesion. The aesthetic and functional result was satisfactory, with minimal morbidity in the donor area.
REFERENCES
1. Chang CS, Swanson JW, Wilson A, Low DW, Bartlett SP. Columellar reconstruction following nasal continuous positive airway pressure injury. Plast Reconstr Surg. 2018 Jan;141(1):99e-102e.
2. Chao JW, Raveendran JA, Sauerhammer TM, Rogers GF, Oh AK, Boyajian M. Columellar reconstruction after nasal continuous positive airway pressure associated necrosis. J Craniofac Surg. 2017 Jun;28(4):928-30.
3. Günlemez A, Isken T, Gökalp AS, Türker G, Arisoy EA. Effect of silicon gel sheeting in nasal injury associated with nasal CPAP in preterm infants. Indian Pediatr. 2010 Mar;47(3):265-7.
4. Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child Fetal Neonatal Ed. 2005 Nov;90(6):F480-3.
5. Li Y, Sepulveda A, Buchanan EP. Late presenting nasal deformities after nasal continuous positive airway pressure injury: 33-year experience. J Plast Reconstr Aesthet Surg. 2015 Mar;68(3):339-43.
6. Imbulana DI, Manley BJ, Dawson JA, Davis PG, Owen LS. Nasal injury in preterm infants receiving noninvasive respiratory support: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2018 Jan;103(1):F29-35.
7. Son D, Kwak M, Yun S, Yeo H, Kim J, Han K. Large auricular chondrocutaneous composite graft for nasal alar and columellar reconstruction. Arch Plast Surg. 2012 Jul;39(4):323-8.
8. Teltzrow T, Arens A, Schwipper V. One-stage reconstruction of nasal defects: evaluation of the use of modified auricular composite grafts. Facial Plast Surg. 2011 Jun;27(3):243-8.
9. Burget GC, Menick FJ. The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985 Ago;76(2):239-47.
10. Sherris DA, Fuerstenberg J, Danahey D, Hilger PA. Reconstruction of the nasal columella. Arch Facial Plast Surg. 2002 Jan/Mar;4(1):42-6.
1. Irmandade da Santa Casa da Misericórdia de Santos, Plastic Surgery and Burning
Service, Santos, SP, Brazil.
GCVFS Conception and design study, Writing - Original Draft Preparation, Writing - Review & Editing
CMM Conception and design study, Writing - Original Draft Preparation, Writing - Review & Editing
MATAF Conception and design study, Writing - Review & Editing
Corresponding author: Giovanna Calil Vicente Franco de Souza, Rua Alferes Ângelo Sampaio, 967, Apart. 801, Bairro Água Verde, Curitiba, PR, Brazil. Zip Code: 80250-120. E-mail: giovannacvfsouza@hotmail.com
Article received: April 29, 2019.
Article accepted: July 08, 2019.
Conflicts of interest: none.













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter