

Review Article - Year 2020 - Volume 35 -
Festoons, edema, and malar bags: is there a consensus on aesthetic treatment?
Festoons, edema e bolsas malares: existe consenso no tratamento estético?
ABSTRACT
Introduction: Periorbital changes are some of the first detectable signs of aging. The most outstanding currently, refers to the rejuvenation of this region, involving the treatment from the eyebrows to the transition orbital-malar, where are festoons, edemas, and malar bags. However, this management is complex, involving several approaches: invasive or noninvasive techniques. Thus, this review aims to describe the scientific evidence of the most current techniques used in the treatment of festoons, edema, and malar bags and to evaluate the complications related to each modality.
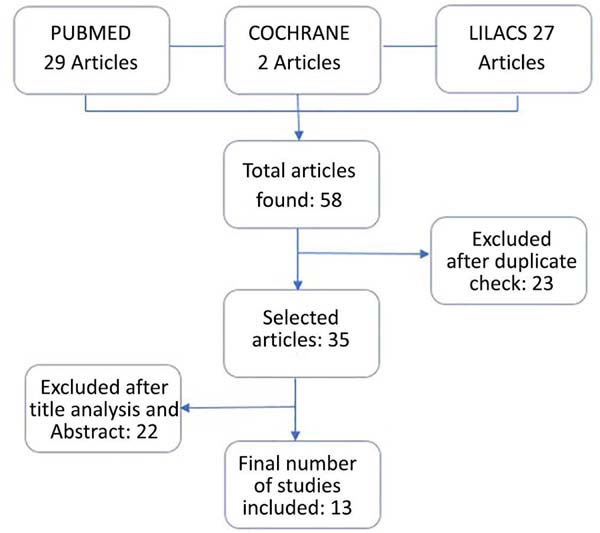
Methods: The research was carried out in three databases, PubMed, Cochrane, and LILACS - using the descriptors "bolsa malar," "malar mounds," "festoons" and "malar bags" in the period from 2014 to 2019, in English and Portuguese.
Results: We selected 13 articles; most of the studies were retrospective reviews (76.9%), seven dealt with noninvasive techniques, three about invasive, and three on the association of techniques. Regarding the procedures described, the noninvasive ones were represented by the use of Kinesio tape, tetracycline injection, doxycycline and hyaluronic acid, and the use of microneedling with radiofrequency. The invasive ones were represented by microaspiration, myocutaneous flap, subperiosteal lift of the middle face, and direct excision.
Conclusion: There are numerous techniques for treating festoon and malar bags, but it is up to the plastic surgeon to know its advantages and disadvantages to decide the most appropriate in each situation. Thus, there is no consensus, but it is vital to diagnose correctly to indicate the best treatment.
Keywords: Conservative treatment; Plastic surgery; Minimally invasive surgical procedures; Edema; Blepharoplasty; Eyelid diseases.
RESUMO
Introdução: As alterações periorbitais são alguns dos primeiros sinais detectáveis do envelhecimento. O destaque, atualmente, refere-se ao rejuvenescimento dessa região, envolvendo o tratamento desde as sobrancelhas até a transição órbito-malar, onde se encontram festoons, edemas e bolsas malares. Entretanto, este manejo é complexo, envolvendo várias abordagens: técnicas invasivas ou não invasivas. Assim, esta revisão objetiva descrever as evidências científicas relacionadas às técnicas mais atuais utilizadas no tratamento de festoons, edemas e bolsas malares e avaliar as complicações relacionadas à cada modalidade.
Métodos: A pesquisa foi realizada em três bases de dados - PubMed, Cochrane e LILACS - utilizando os descritores "bolsa malar", "malar mounds", "festoons" e "malar bags" no período de 2014 a 2019, na língua inglesa e portuguesa.
Resultados: Foram selecionados 13 artigos, a maioria dos estudos eram revisões retrospectivas (76,9%), sete versavam sobre técnicas não invasivas, 3 sobre invasivas e 3 sobre associação das técnicas. Em relação aos procedimentos descritos, os não invasivos foram representados pelo uso de Kinesio tape, injeção de tetraciclina, doxiciclina e de ácido hialurônico, e o uso de microagulhamento com radiofrequência. Já os invasivos foram representados por microaspiração, retalho miocutâneo, lift subperiosteal da face média e excisão direta.
Conclusão: Existem inúmeras técnicas para tratamento de festoon e bolsas malares, mas cabe ao cirurgião plástico conhecer suas vantagens e desvantagens para decidir a mais adequada em cada situação. Assim, não há consenso, mas é vital diagnosticar corretamente para indicar o melhor tratamento.
Palavras-chave: Tratamento conservador; Cirurgia plástica; Procedimentos cirúrgicos minimamente invasivos; Edema; Blefaroplastia; Doenças palpebrais
INTRODUCTION
Aesthetic interventions in the face have been increasingly sought after by patients in the context of plastic surgery, improving the facial contour, and returning the harmony and beauty of the face without losing naturalness1. Data from the American Society for Aesthetic Plastic Surgery (ASAPS) 2017 and the Sociedade Brasileira de Cirurgia Plástica (SBCP) 2016 show that in recent years approximately two hundred thousand surgical procedures have been performed such as blepharoplasty and facelift and more than one million noninvasive procedures on the face as the application of botulinum toxin and hyaluronic acid1,2.
The periorbital region’s rejuvenation has gained prominence in recent years and ranges from the treatment of the eyebrow area to the transition orbital-malar, where the festoons, edema, and malar bags are found. Periorbital changes are one of the earliest detectable signs of aging, but this region is still very neglected because it manifests pathologies that exhibit complex resolutions.
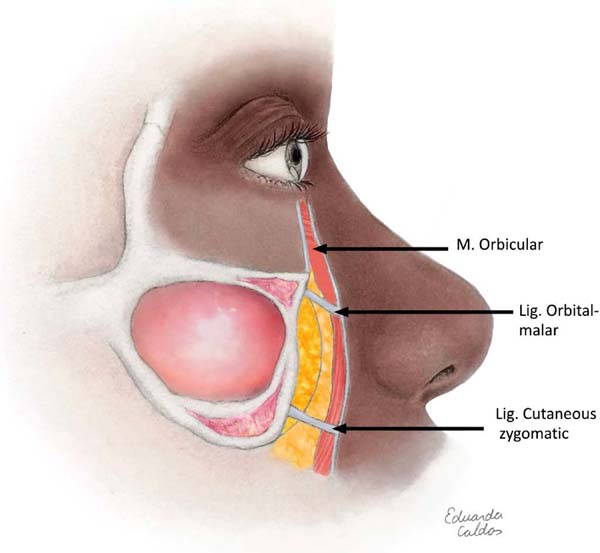
Besides, the region has a variable terminology that hinders diagnosis and treatment. However, more relevant than knowing nomenclature is to know the region’s anatomy, remembering the three main structures involved in the degeneration that occurs with aging: the orbicularis muscle, the orbital-malar ligament and the cutaneous zygomatic ligament (Figure 1). The malar edema is a fluid accumulation on the malar eminence, the malar bag is represented by chronic edema of permanent soft parts and the festoons are an accumulation of cascading skin3.
In this way, anatomical knowledge and current changes in behavior in the face of festoons, edema and malar bags can help in better management. Thus, surgical treatments associated with new invasive and noninvasive treatments lead to the best proposed aesthetic result, respecting the clinical condition and the will of each patient, with the plastic surgeon’s joint decision.
Thus, this study aims to conduct a systematic literature review on the current types of treatments for festoon, edema, and malar bags correction, dealing with invasive and noninvasive techniques. The objective is also to state the main advantages and disadvantages of each technique, besides proposing a modernized treatment algorithm, since there are few studies on the subject.
METHODS
This is a literature review limited to Pubmed database, Cochrane, and LILACS in English and Portuguese between 2014 and 2019, using the following descriptors: “bolsa malar,” “malar mounds,” festoons” and “malar bags. “ Exclusion criteria were: publications without full access, repeated by overlapping the keywords-key, not directly related to the theme, before 2014 and languages other than Portuguese or English. Two independent reviewers conducted the initial research of articles and subsequent selection.
All research information was tabulated in a spreadsheet for statistical data analysis.
This review is supplemented with photos of patients to illustrate some types of treatment, but they are not identified, and their personal information is also not present. Thus, this work does not require approval in the Research Ethics Committee, although the principles of the Helsinki Declaration of 2013 were followed.
RESULTS
The original research yielded 58 records, of which 23 duplicates were removed, leaving 35 articles for the first phase of screening (Figure 2). After title review and summary to determine relevance on the treatment of festoons, edema, and malar bag, 13 were eligible for full-text revision and listed in Chart 1.
| Authors | Year | Technique | Indication |
|---|---|---|---|
| Kpodzo et al.3 | 2014 | Invasive/noninvasive | Malar bag and festoons |
| Hilton et al.8 | 2014 | Noninvasive | Malar edema |
| Stevens et al.14 | 2014 | Invasive | Malar bag and festoons |
| Endara et al.12 | 2015 | Invasive | Festoons |
| Farrapeira16 | 2015 | Invasive | Festoons |
| Perry et al.6 | 2015 | Noninvasive | Festoons |
| Iverson and Patel10 | 2017 | Noninvasive | Malar edema |
| Costin5 | 2018 | Noninvasive | Festoons |
| Asaadi13 | 2018 | Invasive and noninvasive | Festoons |
| Braz et al.9 | 2018 | Noninvasive | Malar bag |
| Jeon and Geronemus11 | 2018 | Noninvasive | Festoons |
| Godfrey et al.7 | 2019 | Noninvasive | Edema and festoons |
| Newberry et al.15 | 2019 | Invasive/noninvasive | Edema, bag and festoons |
Most studies were retrospective reviews (76%), three prospective interventionists (23%), and only one systematic review. The types of techniques employed varied among invasive options (46.15%) and noninvasive (53.85%), being represented by the use of Kinesio tape, local injection of antimicrobial, injection of hyaluronic acid, microneedling with radiofrequency, microaspiration, myocutaneous flap, subperiosteal lift of the middle face and direct excision. The findings were as follows:
Noninvasive treatment
Noninvasive procedures are more conservative and non-surgical interventions, with variable results, used as primary therapy for mild or moderate malar edema with more restriction of outcome in the treatment of bags and festoons. Although not isolated, the first choice for the most advanced conditions, noninvasive procedures, represent adjunct benefits to surgical therapies.
Kinesio Tape
Only one study described the use of Kinesio tape. The tape was indicated to minimize festoon, through on-site application in an ascending vector, with noticeable improvement after three months, but with limited result in the more advanced festoons4.
Tetracycline and doxycycline injection
Two studies focused on the use of antimicrobials in periorbital rejuvenation. In one of them, the application of tetracycline 2% between the orbicularis muscle and deep fascia showed improvement in the contour to correct the festoons5. Doxycycline was used in the concentration of 10mg/ml in order to correct festoons and malar edema6. Complications such as ischemia, necrosis, nerve paralysis, persistent pain, or edema were not identified5. However, the application of these antimicrobials presents limited results, requiring more extensive and more detailed studies to determine the safety and efficiency of this treatment.
Hyaluronic acid injection
In four of the thirteen articles included, there was a description of fillers’ use to treat of edema and malar bag. Most studies agree that moderate to severe cases of malar bags or festoons are not adequately treated with filling, the best therapy being the surgical approach7-9.
Microneedling with radiofrequency
The use of radiofrequency microneedling devices for the treatment of malar and festoon bag was found in two articles, because they provide energy, similar to microwaves, to induce thermal lesions in adipose and dermal tissue, sparing the epidermis and improving the contour of the periorbital region. Studies generally report mild and temporary side effects such as erythema and edema. The procedure can be repeated in 1-2 months if necessary10.
Invasive treatment
The invasive treatment of malar and festoon bags can range from the myocutaneous flap to the direct excision of excess skin. The choice of a given type of surgical procedure depends on the correct diagnosis, the patient’s age, and the pathologies’ associations, among other variables.
Microsuction
Two articles focused on using this technique to treat patients with edema and malar bag. Superficial liposuction is performed to the orbicularis muscle in the subcutaneous plane. The care required is to avoid skin perforations and irregularities in the facial contour11.
Myocutaneous flap - orbicular muscle skin
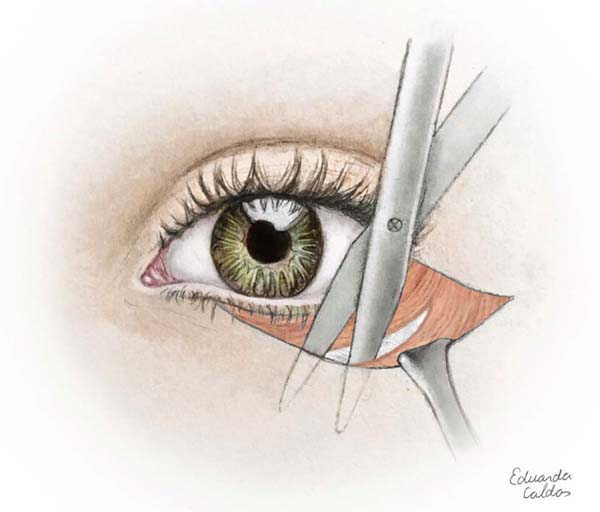
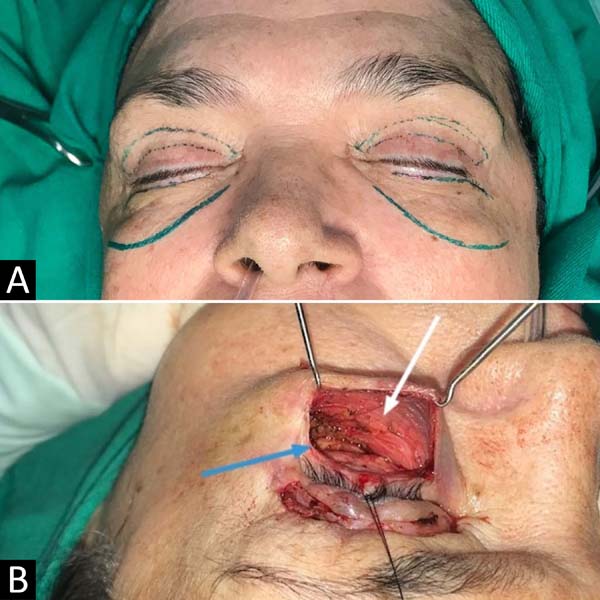
The most performed surgical modality in the studies (38.46%) is indicated for patients with malar bag and mild to moderate festoons11-13. A subciliary incision is performed, myocutaneous flap dissection to the orbital edge and removal of excess skin (Figures 3 and 4)11. Among the complications observed in the studies, we can have ectropion in up to 4% of cases and hematoma in 3%.
Middle face subperiosteal lift
In two studies, the indication of this technique was described for patients with festoons. Three routes can perform this: temporal, transpalpebral, or endoscopic assisted video. All techniques aim to make the resuspension of the orbital-malar ligament and suspension of the soft tissue. The difference is that in the first technique, the access is made by the temporal region, in the second by the lower eyelid, and in the third, an incision is made in the temporal region and the oral mucosa. The disadvantage of the video-assisted technique is the fact that it presents a longer learning curve, longer surgical time, besides attending with approximately 25% of oral wound dehiscence. On the other hand, the transpalpebral route may present hematoma more frequently and the temporal access route3,14.
Direct excision - in canoe
As discussed in three articles, such a procedure is also indicated for patients presenting severe festoons. The incision is made in the festoon’s demarcated area in the form of a canoe or ellipse, and excess skin is removed. As the scar is evident, it is better indicated in older adults. Lagophthalmos and ectropion are the main complication3,15.
DISCUSSION
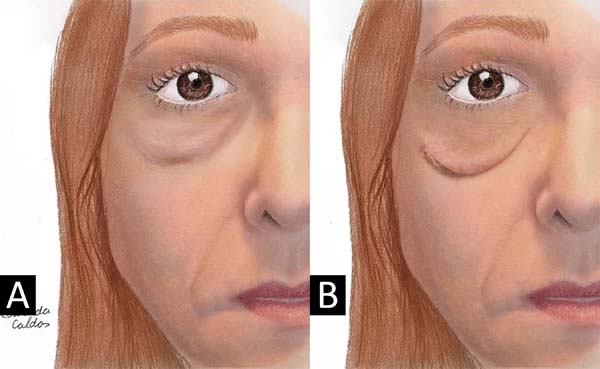
Since 1978, when Furnas first described “festoons”, the terms used to describe edema or excess tissue immediately below the infraorbital border within the pre-zygomatic space are variable. As all three anomalies (edema, malar bag, and festoon) cause lumps, we propose the following definitions to describe this broad anatomical problem: malar edema is an accumulation of fluid on the malar eminence that often varies in severity and can worsen after salty meals or in the morning. The malar bag is chronic edema of soft tissues in the pre-zygomatic space, which contains fat or orbicularis muscle due to descent or hypertrophy, and may be congenital. On the other hand, festoons are loose-skin cascade nets and orbicularis muscle below the infra-orbital edge (Figure 5), may also contain herniated or ptotic fat and accumulate edema. They are often found in older adults and represent a progression of the entities described above16.
The treatment of festoons, edema, and the malar bag is complex, involves diverse pathophysiology and inconsistency of terminology. The choice of an erratic approach will leave patients dissatisfied and with poor aesthetic results. Thus, treatment should be individualized, based on size, content (edema, fat, skin, and muscle), patient preference, and knowledge of the plastic surgeon. The choice of only non-surgical procedures should be made cautiously, as it presents limited results if poorly indicated. Kinesio tape was used in the treatment of festoons, but its mechanism of action is based on the improvement of lymphatic drainage, being better applied in malar edema or after surgeries as an adjuvant to minimize postoperative edema and ecchymosis4. Similarly, radiofrequency microneedling without association with other techniques would not be the best choice for the treatment of festoons, because despite causing a potential reduction of fat and decreased sagging skin in the lower eyelid, it is not enough to bring the best outcome to the patient10.
On the other hand, the use of antimicrobials, according to Perry et al., in 20155, seems to produce activity similar to growth factor, stimulating the proliferation of fibroblasts, as well as collagen production and fibrin deposition. Thus, tetracycline 2% or doxycycline 10mg/ml between the orbicularis muscle and deep fascia can improve the repair of the periorbital surface, however, with a poor result in the correction of festoons and severe malar bag because it already contains excess skin5,6. The use of hyaluronic acid is controversial because, at the same time, it can mask an irregular contour in the periorbital region can also aggravate malar edema in some cases, especially if hydrophilic, with possible involvement of lymphatic drainage8.
Besides, periorbital fat atrophy and malar bone resorption contribute to the loss of the lower periorbital area’s structural support. It is believed that medial and lateral resorption of SOOF(suborbicularis oculi fat) and the regeneration of ligaments and orbicularis leads to loosening the ceiling of the pre-zygomatic space, contributing to the pathogenesis of periorbital aging3,14. Thus, surgical techniques aim to restore the region by acting more anatomically with more predictable and lasting results. The choice of a specific technique over another depends on existing skin excess, patient age, and especially the surgeon’s proximity to the surgical procedure. Microaspiration in the periorbital region acts in such a way as to prevent the malar bag progression to the festoons, besides leading to a local fibrosis and face contour improvement3. The myocutaneous flap, subperiosteal lift, and direct excision rejuvenate the periorbital region by acting on the ligament, muscle regeneration, and excess skin. However, the complications inherent to surgical techniques are more feared and more challenging to treat when compared to less invasive techniques.
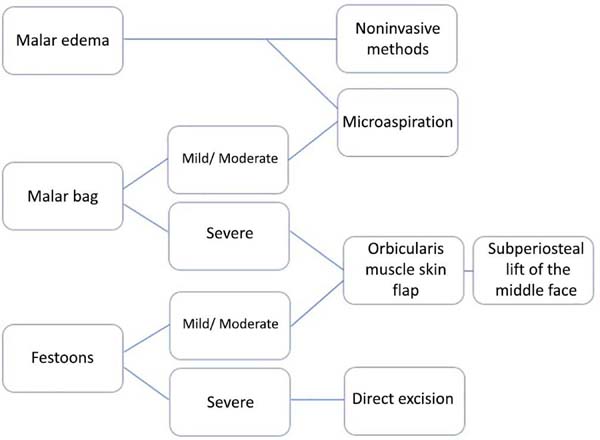
Thus, an algorithm is brought in an attempt to minimize doubts, facilitate the interpretation and choice of treatment in the face of a case of periorbital rejuvenation (Figure 6). It is noteworthy that despite the numerous invasive and noninvasive techniques, a single approach is not revolutionary. Thus, most often, repetitive treatments and a combination of techniques are necessary, leading to an increase in the cost and postoperative recovery time14. Furthermore, studies on the subject are deficient, mainly in Portuguese (found only one in this review), because these are studies at grade IV and V levels, limiting critical analysis and highlighting the need for higher quality studies.
CONCLUSION
There are numerous techniques for treating festoon and malar bags, but it is up to the plastic surgeon to know its advantages and disadvantages to decide the most appropriate for each type of patient. Therefore, there is no consensus, but it is essential to diagnose correctly and remember that the association of techniques may be the best treatment.
REFERENCES
1. International Society of Aesthetic Plastic Surgery (ISAPS). ISAPS International survey on aesthetic/cosmetic procedures performed in 2017 [Internet]. New York: ISAPS; 2017; [acesso em 2019 Jun 20]. Disponível em: https://www.isaps.org/wp- content/uploads/2019/03/ISAPS_2017_International_Study_Cosmetic_Procedure s_NEW.pdf
2. Sociedade Brasileira de Cirurgia Plástica (SBCP). Censo 2016. Situação da Cirurgia Plástica no Brasil [Internet]. São Paulo (SP): SBCP; 2017; [acesso em 2019 Jun 18]. Disponível em: http://www2.cirurgiaplastica.org.br/wp- content/uploads/2017/12/CENSO-2017.pdf
3. Kpodzo DS, Nahai F, McCord CD. Malar mounds and festoons: review of current management. Aesthet Surg J. 2014 Fev;34(2):235-48.
4. Furnas DW. Festoons of orbicularis muscle as a cause of baggy eyelids. Plast Reconstr Surg. 1978;61(4):540-6.
5. Costin BR. Kinesio tape for treatment of lower eyelid festoons. Ophthalmic Plast Reconstr Surg. 2018 Nov/Dez;34(6):602.
6. Perry JD, Mehta VJ, Costin BR. Intralesional tetracycline injection for treatment of lower eyelid festoons: a preliminary report. Ophthalmic Plast Reconstr Surg. 2015 Jan/Fev;31(1):50-2.
7. Godfrey KJ, Kally P, Dunbar KE, Campbell A, Callahan AB, Lo C, et al. Doxycycline injection for sclerotherapy of lower eyelid festoons and malar edema: preliminary results. Ophthalmic Plast Reconstr Surg. 2019 Set/Out;35(4):474-7.
8. Hilton S, Schrumpf H, Buhren BA, Bölke E, Gerber PA. Hyaluronidase injection for the treatment of eyelid edema: a retrospective analysis of 20 patients. Eur J Med Res. 2014 Mai;19:30.
9. Braz AV, Black JM, Pirmez R, Minokadeh A, Jones DH. Treatment of malar mounds with hyaluronic acid fillers: an anatomical approach. Dermatol Surg. 2018 Nov;(44 Suppl 1):S56-S60.
10. Iverson SM, Patel RM. Dermal filler-associated malar edema: treatment of a persistent adverse effect. Orbit. 2017 Dez;36(6):473-5.
11. Jeon H, Geronemus RG. Successful noninvasive treatment of festoons. Plast Reconstr Surg. 2018;141(6):977e-8e.
12. Endara M, Oh C, Davison SP, Baker SB. The management of festoons. Clin Plast Surg. 2015;42(1):87-94.
13. Asaadi M. Etiology and treatment of congenital festoons. Aesthetic Plast Surg. 2018 Ago;42(4):1024-32.
14. Stevens HPJD, Willemsen JCN, Durani P, Rasteiro D, Omoruyi OJ. Triple-layer midface lifting: long-term follow-up of an effective approach to aesthetic surgery of the lower eyelid and the midface. Aesthetic Plast Surg. 2014 Ago;38(4):632-40.
15. Newberry CI, McCrary H, Thomas JR, Cerrati EW. Updated management of malar edema, mounds, and festoons: a systematic review. Aesthet Surg J. 2019;40(3):246-58.
16. Farrapeira AB. Tratamento da bolsa malar e festoons. Rev Bras Cir Plást. 2014;29(4):486-9.
1. Hospital das Clínicas, Department of Plastic Surgery, Federal University of Pernambuco,
Recife, PE, Brazil.
2. University of Pernambuco, Recife, PE, Brazil.
3. Federal University of Pernambuco, Recife, PE, Brazil.
Institution: Hospital das Clínicas, Department of Plastic Surgery, Federal University of Pernambuco, Recife, PE, Brazil.
CSCA Analysis and/or data interpretation, Conceptualization, Data Curation, Formal Analysis, Methodology, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
KWMC Data Curation, Writing - Original Draft Preparation
RXBM Analysis and/or data interpretation, Conception and design study, Data Curation, Formal Analysis, Writing - Original Draft Preparation, Writing - Review & Editing
ALBNS Analysis and/or data interpretation, Data Curation, Formal Analysis, Investigation, Methodology, Writing - Original Draft Preparation, Writing - Review & Editing
EALC Writing - Original Draft Preparation, Writing - Review & Editing
MFMBL Data Curation, Methodology, Writing - Original Draft Preparation
ICGL Project Administration, Supervision, Visualization, Writing - Review & Editing
Corresponding author: Caroline Silva Costa de Almeida, Rua Barão de Itamaracá 78, Espinheiro, Recife, PE, Brazil. Zip Code: 52020-070. E-mail: carol_costaalmeida@hotmail.com
Article received: September 18, 2019.
Article accepted: February 22, 2020.
Conflicts of interest: none.









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter