

Ideas and Innovation - Year 2020 - Volume 35 - Issue 3
Chassaignac bursa flap: protection and support in reduction mammoplasties with implant
Retalho bolsa de Chassaignac: proteção e sustentação nas mamoplastias redutoras com implante
ABSTRACT
Introduction: Macromastias with fatty substitution, great flaccidity, and severe ptosis, constitute a specific group of difficult treatment, many without long-term results. The authors present the technique called Chassaignac bursa flap, indicated for selected cases.
Methods: When applied to 41 patients (2013-2019), the tactic allowed the creation of two independent spaces, one for the removal of the mammary parenchyma and the other isolated, pre-muscular, a flap composed by pedicles semicircular, superior, medial and lateral, dome-shaped, which protect the implant in the Chassaignac retromammary area.
Results: The patients evolved without complications, with the maintenance of the upper pole, a symmetrical harmonic redistribution of the breasts, without recurrent ptosis.
Conclusion: The bag flap proved feasible, allowing for safety during the operation and a lasting implant support.
Keywords: Mammoplasty; Open reduction; Breast implant; Hypertrophy; Surgical flaps.
RESUMO
Introdução: As macromastias com substituição gordurosa, grande flacidez e ptose severa,
constituem um grupo específico de difícil tratamento, muitos deles sem
resultados perduráveis a longo prazo. Os autores apresentam a técnica
denominada retalho bolsa de Chassaignac, indicada para casos
selecionados.
Métodos: Aplicada em 41 pacientes (2013-2019), a tática permite a criação de 2
espaços independentes, um para a retirada do parênquima mamário e outro
isolado, pré-muscular, que consiste em um retalho composto, de pedículo
semicircular, superior, medial e lateral, em forma de cúpula, que protege o
implante na área retromamária de Chassaignac.
Resultados: As pacientes evoluíram sem complicações, com manutenção do polo superior,
uma redistribuição harmônica simétrica das mamas, sem ptoses
recidivantes.
Conclusão: O retalho em bolsa se mostrou factível, permitindo segurança no
transoperatório e sustentação perdurável do implante.
Palavras-chave: Mamoplastia; Redução aberta; Implante mamário; Hipertrofia; Retalhos cirúrgicos
INTRODUCTION
After the publication of Sánchez et al., in 20081, about reduction mammoplasty with a silicone implant, a large contingent of patients began to request it. Some specialists incorporated it into their surgical arsenal, for cases specially selected within the universe of hypertrophies breast cancer. On the other hand, most publications that combine mammoplasties and implants have focused on treating hypomastias and breast ptosis. This one is a topic in which many authors have described techniques, with different tactics, for locating and protecting the implant, as Soares et al. , in 20112, in a double plane; Sánchez et al., 20081, Mansur and Bozola, in 20093, with an inferior pedicle; Gomes, in 20084, with an upper pedicle; Graf et al., in 20035, with a subfascial implant, among others; however, there are few publications regarding combined treatment in macromastias.
The challenges and difficulties of this surgery are similar to the ptosis treatment and begin in the intraoperative period. In most suprapeptorial techniques, a single surgical space is shared by implantation, parenchyma removal and ascending flaps of the areolomamilar complex (AMC) , which increases the frequency of immediate complications, such as hematoma, infection, dehiscence or extrusion and late complications, such as asymmetries and ptosis due to sliding of the implant (bottoming out) or due to tissue fall (waterfall). The retromuscular techniques provide support for the prosthesis; however, in the late evolution, they can also present the animation deformity and the double bubble7, expected consequences for structures of different embryological origins.
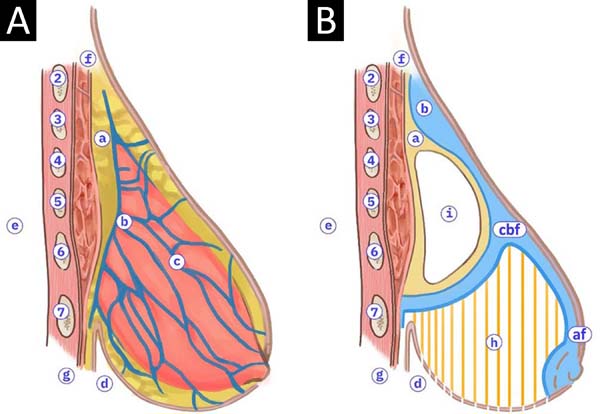
Following the anatomical description of the retromammary space, the posterior breast capsule, and the Giraldes suspensory ligament7,8, we idealized the possibility of surgical construction of a flap composed as a lipo-connective-glandular dome, with a semicircular pedicle (upper, medial and lateral), to protect the loose retromammary areolar space, isolating the implant site from the rest of the surgical procedures. The tactic aims to protect the prosthesis during surgery, to reduce risks in the postoperative period and to provide long-lasting support to the implant and the neo-breast itself, due to the scar adherence in the supradome cleavage plane, avoiding recurrent ptosis, erasure of the upper pole and asymmetries; anatomical aspects illustrated are shown in Figure 1, and we called it the Chassaignac or Kangaroo (CBF) bag flap.
OBJECTIVE
The authors describe the surgical preparation of a bag flap, with the breast base tissues, in a pre-muscular and pre-fascial way, in the dome form, which protects the implant in the Chassaignac space, isolating and supporting it in reduction mammoplasties. It is applied in specifically selected cases.
METHODS
In the period from 2013 to 2019, 41 patients underwent reduction mammoplasty and CBF. They were between 18 and 65 years old, 100% primary, 90% under epidural anesthesia, 10% general, and all were hospitalized for 24 hours. They were followed-up between 6 months to 1 year. The analysis of patient satisfaction was performed every 6 months, in a simple questionnaire form, with three objective questions: very satisfied, satisfied, and not very satisfied. Clinical analyzes and conclusions were carried out, recorded in periodic reviews, with physical examination and photographs, evaluated by a doctor and nurse. The proposed study is authorized by the Institutional Committee of Hospital da Mulher (0072020) and followed the principles of the Declaration of Helsinki. The authors have no conflicts of interest.
Selection
Breast hypertrophies with great liposubstitution, extreme flaccidity, severe ptosis, or total absence of the upper pole.
Round implants, cohesive silicone, high profile, textured, microtextured, or polyurethane, with low volume (175 to 225cc), are used.
Marking
Patient in an orthostatic position, in the following areas (Figure 2):
At the implantation site, cutaneous demarcation of the detachment area, with the help of a circular plate 12 cm in diameter, placed 2 cm from the sternal midline and 1 cm above the breast crease;
In the area of breast resection, using the Pitanguy technique;
In the areas of liposuction, lateral, and pre-axillary, if necessary (S/N).
Surgical technique
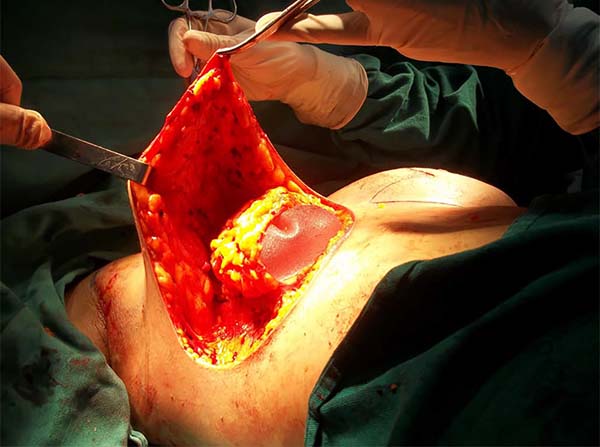
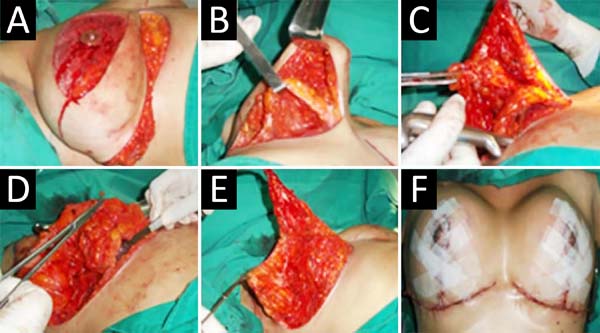
It is infiltrated subcutaneously under demarcation with Villafuerte-Vélez et al. (2017)9: 250cc saline, one adrenaline ampoule, one dexamethasone acetate ampoule (8mgs). Incision of the epidermal design and lateral and axillary liposuction (S/N). Decortication of the periareolar triangle and the lower medial triangle; in this and slightly above the inframammary fold, a 5cm incision was made for retromammary access, detaching the Chassaignac space, in the previously demarcated extension. A wet compress is introduced into the pocket, continuing with breast resection, initiated by the suprafascial side. In the medial area, a protective dome of the implant pocket is advanced, constituted by the posterior mammary capsule, free in its upper and internal area. The retroareolar and upper tissue are dried out in block and keel. It is also possible to remove all breast tissue, from upper to lower, preserving and sculpting the protective bag extended by the compress. Then, the superomedial pedicle flap, for areolar transposition, the retromammary compress is removed, and the silicone implant is inserted (Figure 3), closing the entrance via with 3-0 nylon.
Finally, the breast is assembled with pillar sutures (S/N), subcutaneous tissue and AMC repositioning; 2-0, 3-0, 4-0, 5-0 mononylon yarns, and 4-0 polyglycolic acid are used. The surgical sequence is shown in Figure 4. The drain is placed through the side incision (nasogastric tube 16), the dressing with neomycin ointment, compresses, and surgical bra. The drain is removed and discharged after 24 hours, weekly review for one month, followed by monthly.
RESULTS
Of the 41 patients (2013-2019), we obtained: 1 case of small medial skin dehiscence (2.43%); 1 case of hypertrophic scarring (2.43%); 2 cases of mild asymmetry of the AMC (4.87%); no case of hematoma, necrosis, infection, extrusion or contracture; 1 case of mild unilateral ptosis (2.43%); and there was no complaint of paresthesia. The aesthetic result obtained an excellent degree of satisfaction in 97.56% of the cases, and the average breast removal was 1.640g (Figures 5, 6, and 7).
DISCUSSION
The paradox of removing large breast volumes and, simultaneously, placing implants, has its specific application in challenging pathologies, since, for them, the medium- and long-term results, with other techniques, could be susceptible to complications and dissatisfaction1. After continuous clinical observation of the breast position in the profile view, we conclude that the mammary base and its inframammary fold are always in constant position; the groove is fixed, at the level of the 7th rib and acts as a pivot, it does not descend, even in large hypertrophies or ptosis, allowing the breast base to tilt, but without overpassing the breast adhesion (Figure 8), an anatomical fact that is also noticeable in breasts with lower thoracic implantation, which we believe to be of great value in the proposed surgical resource.
The publication by Sampaio et al., in 201310, rescues us the importance of retromammary anatomy, proposing basilar removal (Giraldes breast capsule) and Chassaignac bursa, for greater adherence in breast reconstructions with a submuscular prosthesis. However, the authors of this article propose a new approach, taking advantage of these anatomical structures to make a pre-muscular pouch that protects the implant and functions as a barrier and support capsule, preventing inferior or lateral slips. This principle is similar to that published by Faria et al., in 201711, in the Lockpocket technique for mammoplasty/mastopexy with subfascial implants, an excellent proposal in ptosis with smaller hypertrophies, but limited in large hypertrophies, where the pectoral fascia is atrophic, a clinical observation made after more than a decade of the gigantomastia treatment program12.
Besides, the velcro healing effect of the remaining breast tissues is added, in the dissection plane above the kangaroo bag, allowing its firm and adherent redistribution, also avoiding recurrent breast ptosis.
The use of silicone presented here is not for increasing but recommended to maintain the upper pole when smaller volumes of prostheses are indicated, fulfilling the main objective of the breast reduction.
CONCLUSION
The basis of the Chassaignac bursa flap (CBF) has its anatomical key in the construction of a pedicled dome structure, as a protective barrier, which offers security during the operation and support of the implant and the neo-breast in the long term, being practiced in cases selected, which combine the reduction mammoplasty and the implant.
REFERENCES
1. Sanchéz J, Carvalho AC, Erazo P. Mastopexia com prótese: técnica em “D” espelhado. Rev Bras Cir Plást. 2008;23(3):200-6.
2. Soares AB, Franco FF, Rosim ET, Renó BA, Hachmann JOPA, Guidi MC, et al. Mastopexia com uso de implantes associados a retalho de músculo peitoral maior: técnica utilizada na Disciplina de Cirurgia Plástica da Unicamp. Rev Bras Cir Plást. 2011 Dez;26(4):659-63. DOI: http://dx.doi.org/10.1590/S1983-51752011000400021
3. Mansur JRB, Bozola AR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24(3):304-9.
4. Gomes RS. Mastopexia com retalho de pedículo superior e implante de silicone. Rev Bras Cir Plást. 2008;23(4):241-7.
5. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003 Fev;111(2):904-8. DOI: http://dx.doi.org/10.1097/01.PRS.0000041601.59651.15
6. Khavanin N, Jordan SW, Rambachan A, Kim JY. A systematic review of single-stage augmentation-mastopexy. Plast Reconstr Surg. 2014 Nov;134(5):922-31. DOI: http://dx.doi.org/10.1097/PRS.0000000000000582
7. Bono JEP. Mamoplastia ligamentar. Rev Bras Cir Plást. 2008;23(3):192-9.
8. Procópio LD, Silva DDP, Rosique R. Implante submuscular em duplo bolso para mastopexias de aumento. Rev Bras Cir Plást. 2019;34(2):187-95.
9. Villafuerte-Vélez CK, Castro-Cabrera AC, Restrepo-Villafuerte C. Corticoterapia profiláctica transquirúrgica de la hiperplasia cicatricial. Estudio clínico-estadístico prospectivo. Cir Plást Iberolatinoam [Internet]. 2017 Mar; [citado 2020 Abr 25]; 43(1):33-9. Disponível em: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922017000100005&Ing=es
10. Sampaio MM, Fraga M, Ferreira AP, Barros AC. Structured mammaplasty: a new approach for obtaining breast symmetry. Plast Reconstr Surg. 2013 Fev;131(2):300e-2e. DOI: http://dx.doi.org/10.1097/PRS.0b013e318278d7d9
11. Faria CADC, Moura LG, Almeida CM, Galdino MCA, Santos GC, Pedroso DB, et al. Mammoplasty/mastopexy using implants: the Lockpocket technique. Rev Bras Cir Plást. 2017 Jan;32(2):218-24.
12. Villafuerte-Vélez CK. PROTG-Programa social de tratamiento de la gigantomastia, Bahía-Brasil. Cir Plást Iberolatinoam [Internet]. 2018 Set; [citado 2020 Abr 25]; 44(3):341-6. Disponível em: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922018000300020&lng=es
1. Hospital Municipal da Mulher, Department of
Plastic Surgery, Feira de Santana, BA, Brazil.
2. University of Salvador, Faculty of Medicine,
Salvador, BA, Brazil.
3. Universidad Abierta Interamericana, Faculty of
Medicine, Rosario, Santa Fe, Argentina.
Corresponding author: Cesar Kelly Villafuerte Velez Avenida João Durval, 3665, Multiplace 305, Feira de Santana, BA, Brazil. Zip Code: 44051-900 E-mail: kelly@gd.com.br
Article received: June 05, 2020.
Article accepted: August 08, 2020.
Conflicts of interest: none.
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter