

Original Article - Year 2020 - Volume 35 -
A new concept in neck aging: "cervicofacial waist"
Um novo conceito em envelhecimento de pescoço: "cintura cervicofacial"
ABSTRACT
Introduction: The aging of the lower third of the face stimulates the definition deletion of the mandibular border and the cervicofacial angle, besides the appearance of platysmal bands in the anterior neck region. Patients have high expectations that the facelift will significantly resolve such effects. To achieve these results, we have developed an approach to defining what we call the cervicofacial waist.
Methods: The author proposes a new surgical facelift approach that has been performed on 444 consecutive patients since 2015, which involves an aggressive plication of the SMAS-platysma plus lateral traction, also by plication, of the platysma medial bands. Results: Despite the difficulty in comparing results with different techniques, we perceive a significant improvement in our results with the new surgical technique, without increasing the complication rates.
Discussion: We are looking for new techniques because the cervical region's traditional treatments seem flawed and based on ill-founded concepts. These involve the medial plication of the platysma bands by a submental approach, bringing them closer together and impairing the cranial elevation of the SMAS-platysma. Thus, we started to directly perform lateral plications on the bands through the lateral access of the face detachment, making a cervicofacial waist.
Conclusion: The sum of the effects of the plication of the SMAS with the lateral plication of the platysma medial band makes the cervicofacial definition clearer with important optimization of the desired aesthetic effects.
Keywords: Rhytidoplasty; Neck; Aging; Superficial musculoaponeurotic system; Lipectomy.
RESUMO
Introdução: O envelhecimento do terço inferior da face promove o apagamento da definição
da borda mandibular e do ângulo cervicofacial, além do surgimento das bandas
platismais na região anterior do pescoço. Os pacientes têm grande
expectativa de que o facelift resolva de maneira
significativa tais efeitos. Para alcançar estes resultados, desenvolvemos
uma abordagem cuja finalidade é a definição marcante do que chamamos de
cintura cervicofacial.
Métodos: O autor propõe uma nova abordagem cirúrgica de facelift já
realizada em 444 pacientes consecutivos, desde 2015, que envolve uma
plicatura agressiva do SMAS-platisma somada a uma tração lateral, também por
plicatura, das bandas mediais do platisma.
Resultados: Apesar da dificuldade em comparar resultados com diferentes técnicas,
percebemos claramente uma melhora significativa nos nossos resultados com a
nova técnica cirúrgica, sem aumento dos índices de complicações.
Discussão: Buscamos novas técnicas pelo fato de que os tratamentos clássicos da região
cervical nos parecem falhos e baseados em conceitos mal fundamentados. Estes
envolvem a plicatura medial das bandas platismais por abordagem
submentoniana, aproximando-as e prejudicando a elevação cranial do
SMAS-platisma. Assim, passamos a realizar plicaturas laterais diretamente
sobre as bandas através do acesso lateral do descolamento da face, com
confecção de uma cintura cervicofacial.
Conclusão: A soma dos efeitos da plicatura do SMAS com a plicatura lateral da banda
medial do platisma torna a definição cervicofacial mais nítida com
otimização importante dos efeitos estéticos desejados.
Palavras-chave: Ritidoplastia; Pescoço; Envelhecimento; Sistema musculoaponeurótico superficial; Lipectomia
INTRODUCTION
In the early days of plastic surgery, the various attempts to treat wrinkles were based on the idea that wide tissue detachments associated with skin strips resections with the skin’s traction would generate faces with a rejuvenated aspect. However, what these techniques were able to achieve were ephemeral results and poor quality scars1-7. From the SMAS treatment concepts, there was a vast evolution in facelift techniques, with the achievement of more lasting and more natural results1-4,6-9.
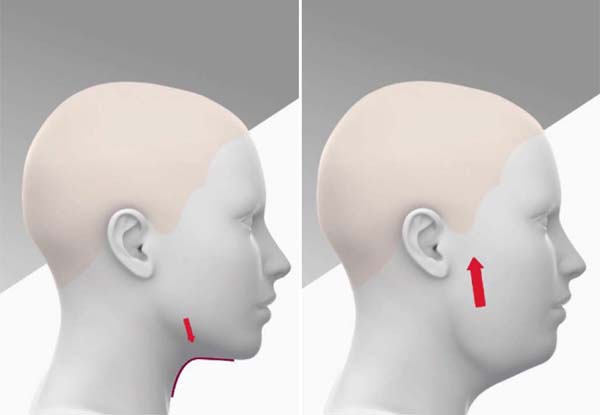
The superficial and deep facial tissues are continuously subject to environmental factors such as sun and pollution, the muscle relaxation process, and gravity action, which, together, aggravate the face aging process10. As gravity result, aging of the face lower third causes the definition of the mandibular edge and cervicofacial angle to be erased, besides the appearance of platysmal bands in the anterior region of the neck, because of the fall of the SMAS-platysma1,7,10) (Figure 1).
Ellenbogen and Karlin created, in 19808, criteria to define success in a cervical rejuvenation process: a very evident mandibular line, presence of subhioid depression, thyroid protuberance, defined border of the sternocleidomastoid muscle and a cervicomentual angle of 105 to 120 degrees8. Although still current and very accurate, the most important thing is to try to bring the contours of the lower third of the face closer to those that the patient had when she was younger.
Those who undergo facelift have high expectations of reaching a well-marked and youthful cervical and mandibular line, often considering them essential aspects in the aesthetic success of the surgery1,4,7,8. To achieve these results more predictably and efficiently, we have developed an approach that clearly defines what we call “cervicofacial waist.”
OBJECTIVE
The objective of the present work is to describe and demonstrate the efficiency increase in the cervicofacial angle definition during the facelift through a cervical strapping technique based on the platysmal band’s lateral plication.
METHODS
The technique of platysmal bands lateral plication with the cervicofacial waist definition was performed by the author in all subsequent cases from its conception in January 2015 until February 2019. This technique was performed in 444 consecutive facelifts (there were no criteria for not inclusion or exclusion). The patients’ age ranged from 37 to 79 years, with a mean age of 58.6. Four hundred thirty-three women and 11 men underwent the procedure.
All surgeries were performed in a hospital with general anesthesia, and the patients were discharged the morning after surgery. All followed the same protocols for preoperative assessment, prevention of thromboembolism, and bruising.
All the cases analyzed were conducted at the plastic surgery clinic Cló & Ribeiro, in Belo Horizonte, Brazil, from January 2015 to February 2019. The analysis of the medical records occurred between August and November 2019. The elaboration of the article followed the Helsinki principles.
Description of the surgical technique - cervicofacial waist
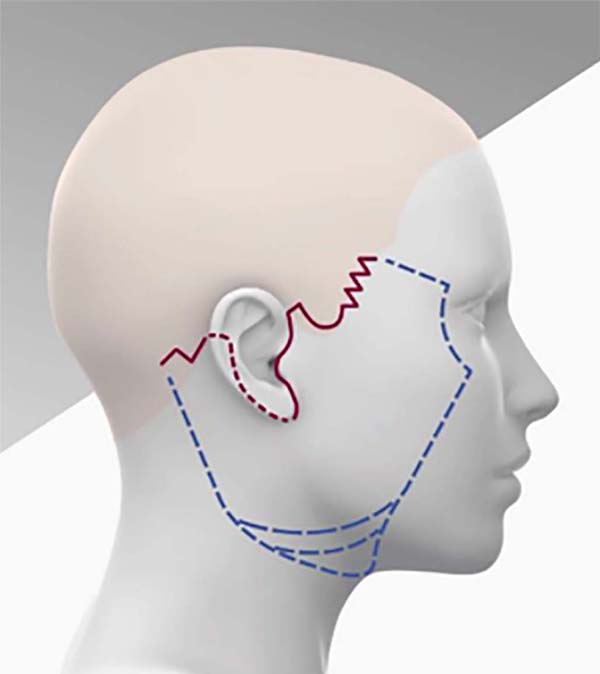
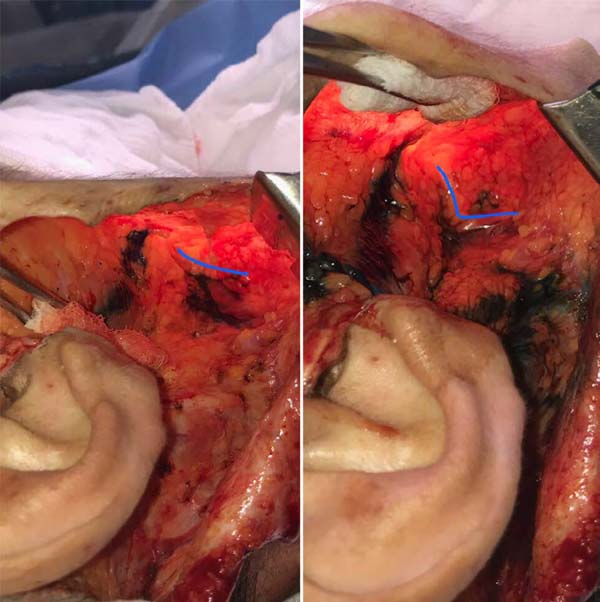
During the facelift, we prolonged the detachment of the skin flap in the inframandibular region in the form of a narrow tunnel to the ipsilateral medial platysmal band, previously marked with the patient seated (Figures 2 and 3).
A lipectomy is performed on the platysma surface to make it appear in the platysmal band area to be treated, using scissors or aspirating with a Pontes cannula1.
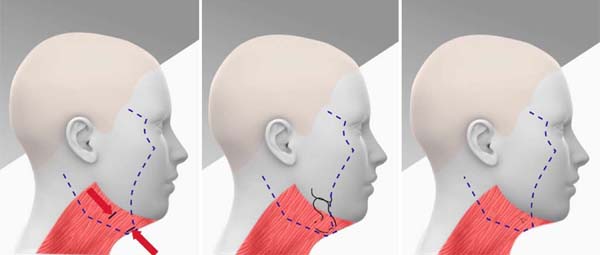
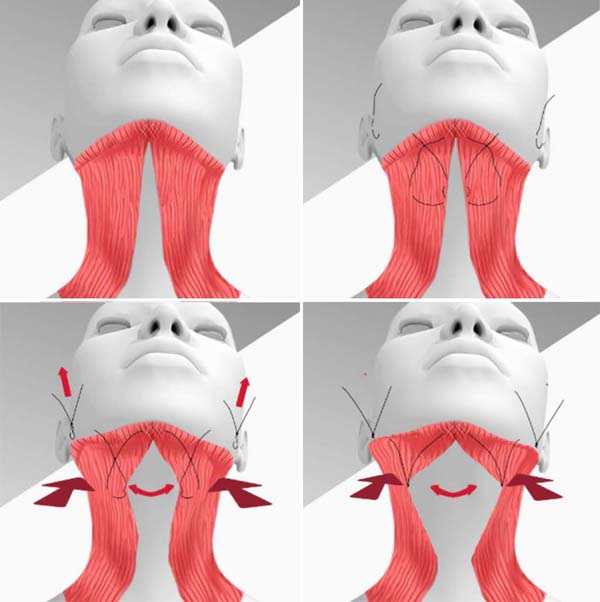
Next, we perform the lateral plication of each band through a single “U” or “X” suture with a double pass and 2-0 nylon thread. The first pass of the suture contours the edge of the platysmal band in the cervicofacial angle region, and the second passes laterally about 3 centimeters from the first. When the knot is tied, the platysma band is significantly lateralized, and the cervicofacial angle begins to be well defined. Likewise, central flaccidity in the anterior region of the neck is attenuated (Figure 4).
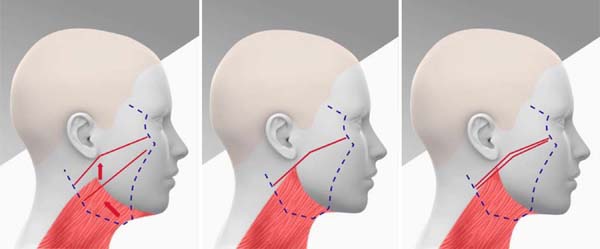
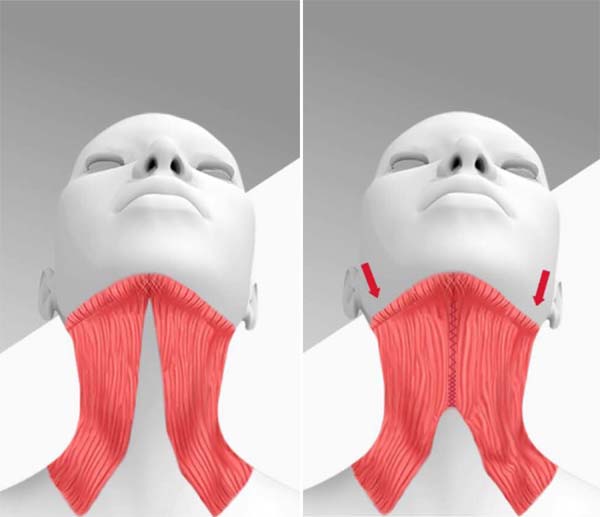
Then we started plicating the SMAS-platysma with two 2-0 nylon sutures. One pre-auricular, just above the angle of the mandible, and another infra-auricular just below, both close to the earlobe. The traction is done in a cephalic direction with a clear suspension effect. In this region, we do the most significant traction of the SMAS plication, reaching 3 to 4 centimeters in width. This great superior traction over the mandible’s angle enhances the effect of the previous lateral plication of the platysma medial band. Thus, it defines the mandible edge, as it deepens the inframandibular region, giving the desired effect of defining the waist from the entire cervicofacial angle (Figure 5).
After these two main sutures in the region of the mandible angle, we finish the plication of the SMAS on the face and neck (Figures 6 and 7 - perioperative photos of the waist definition - internal and external aspect).
RESULTS
It is tough to compare results obtained with the various facelift techniques4,11) objectively. The characteristics of each face and the number of aging changes in each face are very varied. Those with higher degrees of sagging and falling may have an excellent result when considering the case’s difficulty but may have a worse degree of the final definition of the mandibular edge or cervicofacial angle than others that had less severe sagging and falling. Besides, even though the surgeon can assess the final result of a case as excellent, taking into account objective criteria, the degree of demand and expectation of the patient may lead her to consider the same final result to be only reasonable. It is good to remember that the patient often compares her final result with that of other patients instead of comparing it with her preoperative appearance. Therefore, we opted for the methodology that we explain below to compare several results obtained by the author before and after using this technique.
One of the team’s plastic surgeons, who does not participate or perform facelifts, evaluated pre- and postoperative photographs of 100 patients who underwent face surgery by the author, 50 cases were operated before using the technique (before 2015) and 50 already with its use (from 2015). All postoperative photos of the author are taken 5 to 7 months after surgery, and it is important to remember that some patients do not take them. Therefore, in each of the groups, all included cases were consecutive, as long as they had postoperative photos.
The examiner was blinded as to the technique used in each patient and evaluated the degree of improvement in each case concerning three parameters: mandibular definition, cervicofacial angle, and platysmal bands. The final result was classified as weak, good, very good, or excellent (Figures 8 to 15). Through this analysis, we obtained the results shown in Tables 1 and 2.
Thus, we see a significant increase in results considered excellent and a significant decrease in results considered only good or even weak (Figure 16).
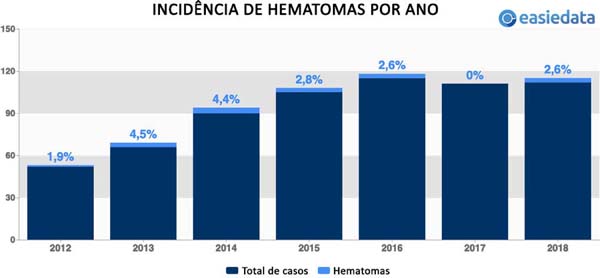
There was no increase in the main complications of the facelift in the evaluated period. The beginning of this technique coincides with the period in which the author started to dedicate himself exclusively to facial plastic surgeries, having concomitantly adopted a strict hematoma prevention protocol, the main complication of facelifts12-16. It can be observed a significant drop in the incidence of hematomas despite the progressive increase in the number of cases operated in the same period, which went from 52 in 2012 to 112 cases in 2018 (Figure 17).
| Old technique (with plication of the S MAS-platysma without lateral plication of the platysmal bands) |
|
|---|---|
| Excellent | 11 |
| Very good | 21 |
| Good | 12 |
| Weak | 6 |
| Current
technique (with plication of the SMAS-platysma and with lateral plication of the platysma bands) |
|
|---|---|
| Excellent | 21 |
| Very good | 22 |
| Good | 5 |
| Weak | 2 |
DISCUSSION
Our discontent with the treatment and definition of these areas has always been significant. The traditional treatments that involve the medial approximation of the platysmal bands by a submentonian approach seemed flawed and based on ill-founded concepts.
As they age, suffering from gravity, the platysmas, and their medial bands move away from the cervicofacial angle in a caudal direction. Thus, face aging favors the definition deletion of the mandibular edge and the cervicofacial angle, as well as the appearance of platysma bands in the neck’s anterior region because of the fall of SMAS-Platysma1-7,10,17.
Despite these bands not moving away from each other in a lateral direction, many authors continue to propose their aggressive medial approach through plication through submental access7,9,10,18,19,20.
McKinney et al., In 199617, proposed a classification to define the aging degree of the face lower third (Table 3)17,1 and Feldman, in 199020, developed a medial plication technique that influenced several plastic surgeons around the world entitled by him as “Corset.” In such a technique, he proposes a double suture of rigorous approximation of the medial edges with progressive tightening and overlapping of the medial muscle edge, similar to a corset, without drying out or cutting the platysma muscle18-20
| Grade | Characteristics |
|---|---|
| I | Barely visible platysmal bands. |
| II | Moderately visible platysmal bands. |
| III | Very visible platysmal bands. |
| IV | Very visible platysmal bands with excessive skin flaccidity. |
Rohrich et al., in 20115 and 20164, and other authors, use concepts similar to those of Feldman, however they associate with this treatment several types of sections of the medial edges of the platysma7,9,10,18-22.
Despite the good results achieved by surgeons who use such concepts and techniques, we understand that such an approximation of the medial bands will act in a counterproductive manner in the elevation of the SMAS-platysma in the cranial direction. In our opinion, although this maneuver causes the definition of the cervicofacial angle, it prevents the proper elevation of the pre-auricular SMAS-platysmas (Figure 18).
For many years, we have performed plicatures on facelifts that promote aggressive suspensions of the pre- and infra-auricular SMAS-platysmas, especially in the region of the mandibular angles, where, often, the width of the plications reaches 4 cm on each side. When we performed submentonian medial plications of the platysmal bands, we never achieved such significant lateral elevations of the SMAS.
Even though we have frequently been able to perform these large elevations in recent years, in a significant number of cases, we have encountered still unsatisfactory results concerning the definition of the cervicofacial angle in the anterior neck.
In many cases, we note that in addition to the elevations of the pre- and infra-auricular SMAS, some type of lateral traction would be needed that would act more directly on the anterior neck10,23. It was clear that tractions performed at a distance from the anterior cervical midline often did not have the efficiency that a maneuver performed directly over the bands would have. Like Pelle-Ceravolo et al. (2016)10, we also believe that the conventional traction of the lateral edge of the platysmas, far from their medial bands, has a limited effect on them.
To optimize the results, we must perform lateral traction as close as possible to the area where we want the highest definition, that is, directly over the medial bands. Also, the sum of these tractions promotes a significant decrease in the neck diameter in the region of the cervicofacial angle (cervicofacial waist).
Thus, as of January 2015, we began to use a new technique for treating platysmal bands and accentuated the definition of the anterior neck. We started to perform lateral plications directly on the bands through the lateral access of the face detachment.
The submental is approached whenever necessary, either for liposuction or for the treatment of subplatysmal fat. When necessary, the medial bands can receive only an approach suture in the region of the largest bulging in the subment. When used, this single suture is made close to the submental incision and far from the cervicofacial angle.
What we propose, in addition to promoting an effective treatment of platysmal bands, surprised us by significantly enhancing the effect of our suspension with aggressive plication of the SMAS-platysma. A high definition of the mandibular edges and the cervicofacial angle is created in the anterior neck, and to this effect, we call the cervicofacial waist (Figure 19).
Differently than Pelle-Ceravolo et al., in 201610, our support of the cervicofacial angle in the anterior neck is made by adding the effects of the “X” suture directly over the platysmal band and the plication in the cephalic sense of the SMAS of the region of the mandibular angle.
Pelle-Ceravolo et al. (2016)10, fix the traction of the edge of the platysma bands at a distance in the mastoid region, leaving long strands that cross the region below the mandible angle. As the surgery is performed with the face turned to the opposite side, these long threads that join the traction bands to the mastoid region certainly lose tension when the patient rectifies the face, reducing its traction effect.
As we do, the effect of the plication performed on the medial platysmal band enhances the effect of SMAS cephalic plication on the entire flaccidity of the anterior neck.
CONCLUSION
The sum of the effects of the SMAS plication and the lateral plication of the platysma’s medial band makes the cervicofacial definition clearer and creates the effect of defining the waist of the neck just below the angles and branches of the mandible. Besides, it made the platysmal bands and submandibular glands imperceptible in the vast majority of cases through traction and increased platysma tension. The technique benefit becomes evident when we observe, in addition to the comparative study results, its use by the author in more than 400 consecutive cases since the first time in 2015.
REFERENCES
1. Pontes R. O universo da ritidoplastia. Rio de Janeiro: Revinter; 2011.
2. Pitanguy I, Radwanski HN, Amorim NFG. Treatment of the aging face using the “round-lifting” technique. Aesthet Surg J. 1999;26:216.
3. Castro CC. Ritidoplastia: arte e ciência. Rio de Janeiro: DiLivros; 2007.
4. Rohrich RJ, Narasimhan K. Long-term results in face lifting: observational results and evolution of technique. Plast Reconstr Surg. 2016 Jul;138(1):97-108.
5. Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty: Blending the eyelid-cheek junction. Plast Reconstr Surg. 2011 Set;128(3):775-83.
6. Cló TCT, Flávio WF, Leão CEG, Cló FX, Lacerda LM, Leão LR. Sistematização perioperatória para prevenção de hematomas em face-lifts: abordagem pessoal após 1138 casos operados. Rev Bras Cir Plást. 2019;34(1):2-9.
7. Warren RJ, Neligan P. Cirurgia plástica estética. 3ª ed. Rio de Janeiro: Elsevier; 2015. v. 2.
8. Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976 Jul;58(1):80-8.
9. Narasimhan K, Stuzin JM, Rohrich RJ. Five-step neck lift: integrating anatomy with clinical practice to optimize results. Plast Reconstr Surg. 2013 Ago;132(2):339-50.
10. Pelle-Ceravolo M, Angelini M, Silvi E. Complete platysma transection in neck rejuvenation: a critical appraisal. Plast Reconstr Surg. 2016 Out;138(4):781-91.
11. Castro CC, Aboudib JHC, Giaquinto MGC, Moreira MBL. Avaliação sobre resultados tardios em ritidoplastia. Rev Bras Cir Plást. 2005;20(2):124-6.
12. Cló TCT, Flávio WF, Cló FX. Necrose extensa em face pós-ritidoplastia: relato de caso. Rev Bras Cir Plást. 2019;34:90-3.
13. Baker DC, Stefani WA, Chiu ES. Reducing the incidence of hematoma requiring surgical evacution following male rhytidectomy: a 30-year review of 985 cases. Plast Reconstr Surg. 2005 Dez;116(7):1973-85.
14. Pitanguy I, Ramos H, Garcia LC. Filosofia, técnica e complicações das ritidectomias através da observação e análise de 2600 casos pessoais consecutivos. Rev Bras Cir. 1972;62:277-86.
15. Weissman O, Farber N, Remer E, Tessone A, Trivizki O, Bank J, et al. Post-facelift flap necrosis treatment using charged polystyrene microspheres. Can J Plast Surg. 2013 Spring;21(1):45-7.
16. Mustoe TA, Park E. Evidence-based medicine: face lift. Plast Reconstr Surg. 2014 Mai;133(5):1206-13.
17. McKinney P. The management of platysma bands. Plast Reconstr Surg. 1996;98(6):999-1006.
18. Righesso R, Chem EM, Netto R, Martins ALM, Sartori N. Ritidoplastia videoassistida do terço inferior da face: corset videoendoscópico. Rev Bras Cir Plást. 2014;29(3):328-36.
19. Feldman JJ. Neck lift my way: an update. Plast Reconstr Surg. 2014 Dez;134(6):1173-83.
20. Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990 Mar;85(3):333-43.
21. Narasimhan K, Ramanadham S, O’Reilly E, Rohrich RJ. Secondary neck lift and the importance of midline platysmaplasty: review of 101 cases. Plast Reconstr Surg. 2016 Abr;137(4):667-75.
22. Pita PCC, Azevedo SFD, Cabral PO, Melo SRPP. Lifting cervical gravitacional. Rev Bras Cir Plást. 2010;25(2):291-6.
23. Gonzalez R. The LOOP - lateral overlapping plication of the platysma: an effective neck lift without submental incision. Clin Plast Surg. 2014;41:65-72.
1. Cló & Ribeiro Plastic Surgery, Belo
Horizonte, MG, Brazil.
2. Hospital das Clínicas, Federal University of
Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author: Ticiano Cesar Teixeira Cló Rua República Argentina, 507, Bairro Sion, Belo Horizonte, MG, Brazil. Zip Code: 30315-490, E-mail: ticianoclo@gmail.com




































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter