

Original Article - Year 2020 - Volume 35 -
Reconstruction of eyelid zones II and III: case series
Reconstrução das zonas II e III palpebrais: série de casos
ABSTRACT
Introduction: The eyelids represent anatomical structures of high complexity, requiring the plastic surgeon's technical skills and experience to their reconstruction. Defects in these areas happen mainly after tumor resection, with the lower eyelids being a frequent site of lesions of this nature. The options for reconstruction vary according to some criteria, including the size of the resulting defect, location, and depth. The result of the reconstruction is mainly aimed at restoring the proper functioning of this delicate structure.
Methods: This work presents a series of seven cases of patients of different complexity, attended, and treated by the Plastic Surgery Service of the Federal Hospital of Ipanema. We show the versatility of local flaps to restore the proper anatomy and function of the lower eyelid. We also try to highlight different types of tumor pathologies that occur in this region.
Results: No patient evolved with ectropion or anatomical distortion, ultimately obtaining a good cosmetic and functional result.
Discussion: The medial region of the eyelids represents a significant challenge for its reconstruction since, in this topography, there are delicate structures such as the lacrimal canaliculus and the medial canthal ligament. Several local flaps can be used depending on the extent and depth of the defect generated after trauma or tumor excision. Having mastery over the periorbital anatomy and surgical options is essential for successful treatment.
Keywords: Carcinoma, Basal cell; Eyelid neoplasms; Surgical flaps; Face; Anatomy.
RESUMO
Introdução: As pálpebras representam estruturas anatômicas de grande complexidade,
exigindo habilidades técnicas e experiência por parte do cirurgião plástico
para a sua reconstrução. Defeitos nessas áreas são produzidos,
principalmente, após ressecção tumoral, sendo as pálpebras inferiores sede
frequente de lesões dessa natureza. As opções para reconstrução variam de
acordo com alguns critérios, entre eles: tamanho do defeito resultante,
localização e profundidade. O resultado da reconstrução visa sobretudo
reestabelecer o funcionamento adequando dessa nobre estrutura.
Métodos: Este trabalho apresenta uma série de sete casos, de diferentes
complexidades, de pacientes atendidos e tratados pelo Serviço de Cirurgia
Plástica do Hospital Federal de Ipanema. Mostramos a versatilidade dos
retalhos locais para restaurar a anatomia e função adequadas da pálpebra
inferior, bem como ressaltar diferentes tipos de patologias tumorais
incidentes nessa região.
Resultados: Nenhum paciente evoluiu com ectrópio ou distorção da anatomia, obtendo ao
final bom resultado cosmético e funcional.
Discussão: A região medial das pálpebras representa uma área de grande desafio para
reconstrução, uma vez que nessa topografa se localizam estruturas nobres,
como o canalículo lacrimal e o ligamento cantal medial. A depender da
extensão e profundidade do defeito gerado, após trauma ou exérese tumoral,
vários são os retalhos locais que podem ser utilizados. Ter domínio sobre a
anatomia periorbital e das opções cirúrgicas é fundamental para o sucesso no
tratamento.
Palavras-chave: Carcinoma basocelular; Neoplasias palpebrais; Retalhos cirúrgicos; Face; Anatomia
INTRODUCTION
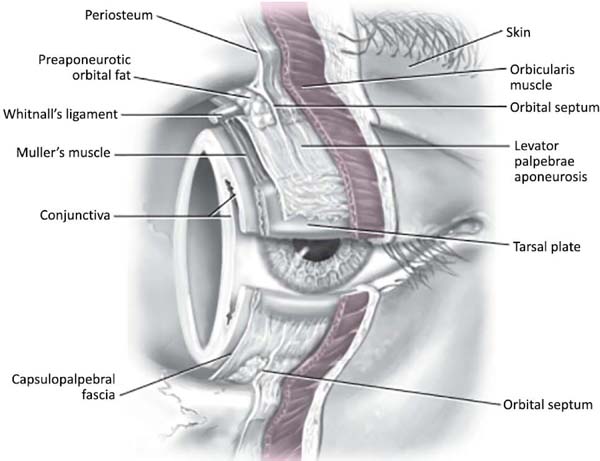
Detailed knowledge of the eyelids and ocular region anatomy (Figure 1) helps the surgeon select the best surgical technique capable of restoring eye function and perfecting the aesthetic result. The eyelid is divided into an anterior and posterior lamella. The anterior lamella is composed of skin and orbicularis muscle. The posterior lamella is composed of the conjunctiva, tarsus, and eyelid retractor muscles. The orbital septum can be considered a median lamella and is not usually reconstructed. The ocular conjunctiva on the surface of the globe is continuous with the conjunctiva that lines the eyelids’ inner surface; this relationship needs to be maintained or restored during reconstruction to preserve eyelid function1,2.
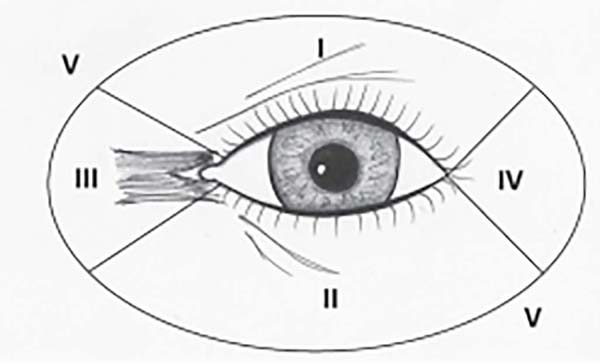
The periorbital zones can be didactically divided, as shown in Figure 2, and are numbered from I to V.
Surgical excision of skin tumors is one of the most frequent causes of eyelid defects. Basal cell carcinoma (BCC) is the most frequent tumor in this location, corresponding to about 90% of cases, with a predominance of lesions in the lower eyelid1. Squamous cell carcinoma, sebaceous carcinoma, and melanoma are less prevalent histological types2. The defects resulting from the excision of cutaneous eyelid tumors require detailed knowledge of the periorbital region’s anatomy and the most appropriate surgical approaches for the success of reconstruction.
OBJECTIVE
The objective of the work is to apply different forms of reconstruction of eyelid defects located specifically in zone II and III or that corresponding to the lower eyelid and the medial angle, respectively.
METHODS
Serie of seven patients between 69 and 90 years old with a surgical wound on the lower eyelid, after removal of malignant tumors, with defects ranging from approximately 30% to 80% of horizontal extension (Table 1). Patients underwent local anesthesia with or without sedation or general anesthesia. After complete excision of the tumor located in the lower eyelid, surgical reconstruction was performed, according to the extent and depth, using neighborhood flaps or skin grafting. In none of the cases, tarsal reconstruction with cartilage graft was not performed, which is usual in lower eyelid surgeries with extensive involvement of this anatomical structure (Figure 2).
| Patient | Sex | Age | Tumor | Location | Surgical Technique |
|---|---|---|---|---|---|
| Patient 1 | M | 90 | Sebaceous carcinoma | Zone III | Imre flap |
| Patient 2 | F | 69 | Basal cell carcinoma | Zone III | Paramedian frontal flap |
| Patient 3 | F | 76 | Basal cell carcinoma | Zone III | Glabellar flap |
| Patient 4 | F | 73 | Basal cell carcinoma | Zone III | Esser flap |
| Patient 5 | M | 81 | Basal cell carcinoma | Zone II and III | Esser flap |
| Patient 6 | M | 76 | Basal cell carcinoma | Zone III | Imre flap |
| Patient 7 | F | 86 | Basal cell carcinoma | Zone II and III | Skin graft |
Different flaps were drawn and made, and a more superficial defect was repaired with a skin graft from the preauricular area.
Case 1
Skin graft: 86-year-old patient, whose lesion affected the skin, reaching zone III, resection was performed with preservation of the middle and posterior lamella structures. Skin grafting was performed, obtaining ipsilateral anterior preauricular skin and repairing the defect (Figure 3).
More superficial defects can be repaired with skin grafts, constitute donor areas: retroauricular and preauricular skin in some cases of the upper eyelid, as they have similarities with the eyelid skin1,4.
Case 2
Paramedian frontal flap: patient presented a recurrent lesion in the right eye (RE) medial canthus with ten months of evolution. Resection and intraoperative freezing were performed. The generated defect had depth up to the orbit periosteal region. The patient had several scar areas in the nasal and glabellar dorsal region; the paramedian and contralateral frontal flap was selected for reconstruction (Figure 4).
Cases 3 and 4
Imre flap: two male patients were selected, the first of them with a large lesion, with partial blockage of the visual axis. He underwent resection with intraoperative freezing. The pathology revealed to be sebaceous carcinoma. The second case was a 76 years old male, with histopathological diagnosis of BCC (Figures 5 and 6).
Case 5
Glabellar flap: 76-year-old patient with an ulcerated lesion in the transition region from the medial palpebral canthus to the nasal dorsum. It was performed a glabellar flap (Figure 7).
RESULTS
Seven patients aged between 69 and 90 years were operated on, four females and three males, six with a BCC diagnosis, and one with a sebaceous tumor. All operated cases were located in periorbital zones II and/or III, in the medial canthus of the unilateral lower eyelid. All of them evolved with useful function without retraction or distortion of the anatomy and preservation of the lacrimal pathways’ drainage.
DISCUSSION
In superficial lesions, a free skin graft is used, which is preferably obtained from the retroauricular region. The skin to be grafted, after cleaning the subcutaneous cell tissue, is sutured in the recipient bed, and a Brow dressing is made. Five days after the dressing is done, the tie-over is removed4. In deep lesions where the bone part is exposed after resection, the glabella VY flap is used, which is practical and simple; two incisions forming an inverted V in the glabella region are made, then the flap is detached and slid to the place where the lesion was resected and sutured1,5.
In cases where the ends of the eyelids are included in the resection, the frontomedial flap is used. In these cases, the surgery will be performed in two stages - the frontomedial flap is initially transposed; after 3 to 4 weeks, the second time is done: the pedicle is resected, the rest being taken to its original bed. Then the area is degreased, and the ends of the eyelids are remade5,6.
The frontal flap is safe, with little morbidity in the donor area, and is an essential option for eyelid reconstructions. The need for a posterior surgical procedure for resectioning the pedicle and the excess volume of flap fat tissue is one of the main disadvantages of this procedure. The patient presented an adequate postoperative evolution without complications7,8.
When the defect is greater than 50% of the lower eyelid, and this same defect has a circular shape, the Imre sliding flap should be considered. The incision is parallel to the lower palpebral margin, extending to the inner canthus and descending to the nasolabial fold. This flap must be well taken off throughout the genian region to avoid ectropion9.
The use of the Imre flap provided good aesthetic and functional result, similar to other flaps commonly used for that kind of reconstructions, such as Mustardé, Esser, and the glabellar flap for the medial canthus. As an advantage, we believe that this method ensures a better positioning of the final scar in the natural grooves of the face9.
The simple or bilobed glabellar flap is characterized by its transposition of skin from the glabellar region to the medial eye canthus. It is essential to incorporate the vascular pedicle of this flap into the supratrochlear artery. The result may not reproduce the concavity typical of the medial eye canthus. It is important to note that hair in the glabellar region represents a disadvantage in using this flap since it can provide hair growth in an area of glabrous skin, such as the inner eye canthus1,6.
The Esser flap is used to repair significant defects in the lower eyelid. Its incision begins in the lateral canthus, extends upwards, and descends to the preauricular region (Figures 8 and 9). The entire flap is dissected in the genian and preauricular region through a plane immediately above the musculoaponeurotic system, and, finally, it is rotated and advanced to cover the defect1,5,7.
CONCLUSION
Eyelid reconstruction requires not only precise anatomical knowledge, but also the most varied surgical techniques to obtain a functional and aesthetically satisfactory result and, thus, minimize postoperative complications.
REFERENCES
1. Mélega JM. Cirurgia Plástica - os princípios e a atualidade I. Rio de Janeiro: Guanabara Koogan; 2004.
2. Baker SR. Retalhos locais em reconstrução facial. 2º ed. Rio de Janeiro: DiLivros; 2009.
3. Spinelli HM, Lewis AB, Elahi E. Atlas of aesthetic eyelid & periocular surgery. New York: W. B. Saunders; 2004.
4. Galimberti G, Ferrario D, Casabona GR, Molinari L. Utilidade dos retalhos de avanço e rotação para fechamento de defeitos cutâneos na região malar. Surg Cosmet Dermatol. 2013;5(1):769.
5. Sasson EM, Codner MA. Eyelid reconstruction. Operat Tech Plast Reconstr Surg. 1999;6(4):250-64.
6. Lima EA. Enxertia de tecido palpebral na reconstrução de tumores cutâneos. Surg Cosmet Dermatol. 2010;2(4):333-5.
7. Spinelli HM, Jelks GW. Periocular reconstruction: a systematic approach. Plast Reconstr Surg, 1993;91(6):1017-24;discussion: 1025-6.
8. Kakizaki H, Madge SN, Mannor G, Selva D, Malhotra R. Oculoplastic surgery for lower eyelid reconstruction after periocular cutaneous carcinoma. Int Ophthalmol Clin. 2009;49(4):143-55.
9. Metzger JT. Joseph Imre, Jr., and the Imre flap. Plast Reconstr Surg Transplant Bull. 1959 Mai;23(5):501-9.
1. Hospital Federal de Ipanema, Department of
Plastic Surgery, Rio de Janeiro, RJ, Brazil.
Corresponding author: Délcio Aparecido Durso Rua Antônio Parreiras 126, Apart. 803, Ipanema, Rio de Janeiro, RJ, Brazil. Zip Code: 22411-020, E-mail: delciodurso@gmail.com
Article received: July 08, 2019.
Article accepted: July 15, 2020.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter