

Original Article - Year 2020 - Volume 35 -
Facelift light, rhytidoplasty for the treatment of the face and neck lower third with reduced scarring and adhesion points
Facelift light, ritidoplastia para tratamento do terço inferior da face e pescoço com cicatriz reduzida e pontos de adesão
ABSTRACT
Introduction: Facelift light represents a technique standardization to treat face and neck lower third, with lesser scars, SMAS plication in all patients, and adhesion points to reduce bruises. Moderate detachment allows the patient to return to their activities faster.
Methods: Surgery is performed after prior periauricular marking of all patients of the area to be detached and the skin's design to be removed. Anesthesia is local with sedation, and without the need for haircuts. Flap detachment, SMAS plication, adhesion points in the anterior and posterior flaps are performed, in addition to the internal suture by layers and liposuction of the subment when necessary. The dressing is compressive without using drains.
Results: One hundred and eighty-five patients underwent rhytidoplasty using this technique since 2014. Their age varied between 31 and 84 years, with an average of 55 years. Lymphatic drainage is performed after seven days, and after two weeks, a considerable reduction in edema has been observed.
Conclusion: Facelift light is a useful technique, simple to perform with reduced scarring and few complications, favoring the early return of patients to their activities.
Keywords: Rhytidoplasty; Plastic surgery; Abnormalities of the skin; Suture techniques; Face.
RESUMO
Introdução: O facelift light apresenta uma padronização da técnica com
o objetivo de tratar o terço inferior da face e o pescoço, com menores
cicatrizes, plicatura do SMAS em todos os pacientes e utilização de pontos
de adesão para redução de hematomas. O descolamento moderado permite um
retorno mais rápido do paciente às suas atividades.
Métodos: A cirurgia é feita após uma marcação prévia periauricular de todos
pacientes, com a área a ser descolada e o desenho da pele a ser retirada. A
anestesia é local e sedação, sem a necessidade de cortes no cabelo. É feito
o descolamento dos retalhos, plicatura do SMAS, pontos de adesão nos
retalhos anterior e posterior, além da sutura interna por planos e
lipoaspiração do submento quando necessária. O curativo é compressivo sem a
utilização de drenos.
Resultados: Foram submetidos à ritidoplastia por essa técnica 185 pacientes a partir de
2014. Com a idade variando entre 31 e 84 anos, sendo a média de 55 anos. É
feita drenagem linfática a partir de sete dias e com duas semanas
observou-se uma redução considerável do edema.
Conclusão: O facelift light é uma técnica eficaz, de simples execução, cicatrizes
reduzidas e com poucas complicações, favorecendo o retorno precoce dos
pacientes às suas atividades.
Palavras-chave: Ritidoplastia; Cirurgia plástica; Anormalidades da pele; Técnicas de sutura; Face
INTRODUCTION
Non-surgical aesthetic procedures, such as botulinum toxin and fillers, are increasingly delaying the indication for facial lifting, especially in the frontotemporal region1. In this context, we observed a lack of publications that contemplate the mini facelift technique with a reduced scar standardization as part of the therapeutic arsenal for the face middle and lower thirds treatment.
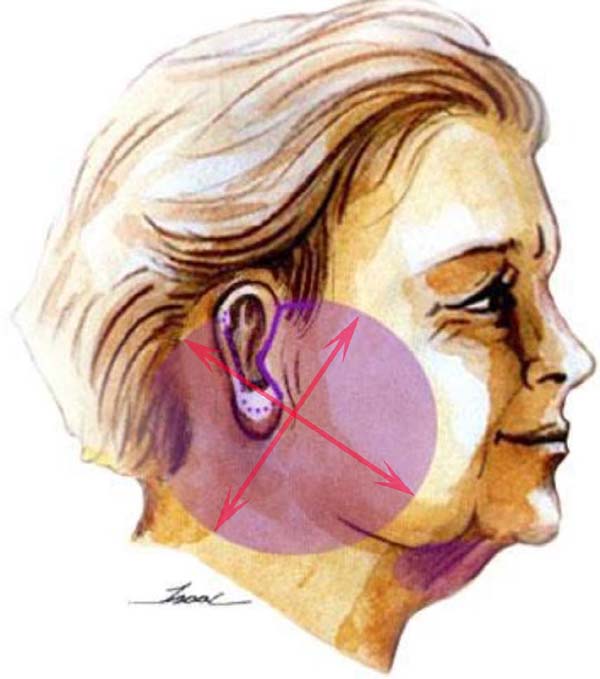
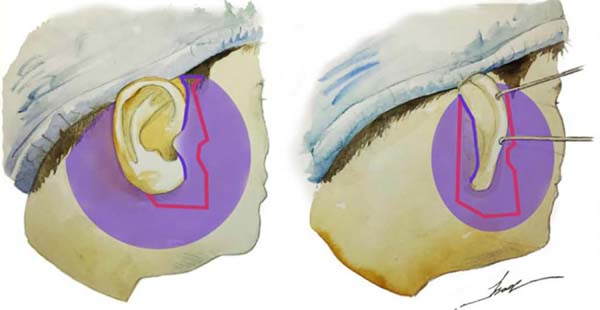
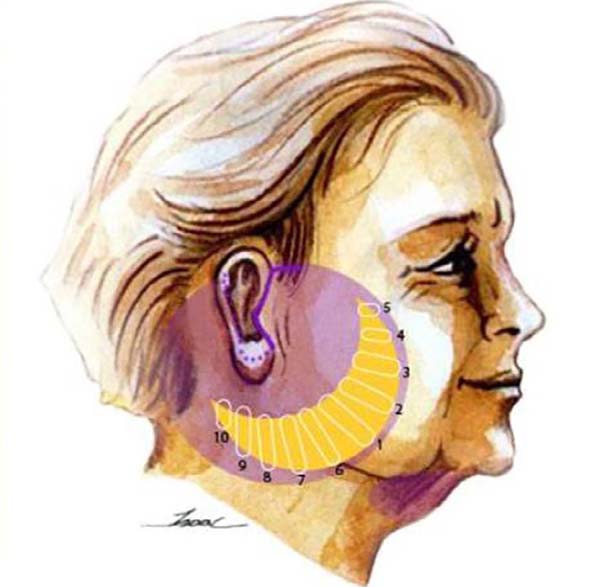
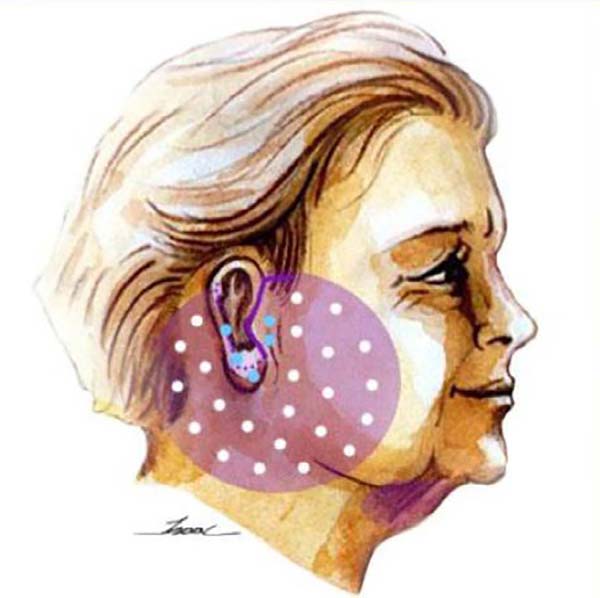
Thus, we used the facelift light technique standardization, which consists in moderate detachment, demarcated in the preoperative period, as well as its execution with specific points for the detachment, associated with the plication of the superficial aponeurotic system (SMAS) and the points of adhesion (Figures 1, 2, 3 and 4). Standardized preoperative marking makes this technique reproducible and with less learning curve, but without compromising the results. The SMAS plication proved to be essential for the best treatment and lasting traction, associated with a reduction in skin tension, with less risk of flap necrosis and a better quality of the scar.
OBJECTIVE
Evaluate the results of the facelift light as a standardized and reproducible technique, the moderate SMAS detachment and plication, with natural results, associated with lower rates of complications and early return to activities.
METHODS
Two hundred eighty-four patients who underwent rhytidoplasty using the facelift light technique were operated on from 2014 to 2020, 39 were men. Patients aged between 31 and 84 years (with a mean of 56 years). All patients were operated on and observed by the same surgeon and author of this study (2014 - 24, 2015 - 35, 2016 - 33, 2017 - 42, 2018 - 51, 2019 - 80, 2020 - 19).
Surgical technique
With the patient in an orthostatic position, the preoperative marking of the region of the incision is made, of the region to be released and of the possible skin to be removed (Figures 1 and 2). Taking the location of the ear lobe insertion as the center of the circumference, we make a circle that varies from 4 to 6 centimeters, according to the existing alterations in the mandible branch (“jowl” or “bulldog”) and the platysmal bands of the neck. In the submental region, liposuction is already scheduled, if necessary.
All patients were operated on a hospital operating room under local anesthesia associated with sedation. Local infiltration was performed with lidocaine solution (40 ml), saline solution (120 ml), and an adrenaline ampoule.
The incision is made only in the glabrous area, so there is no need to cut hair. The incision starts at the rib capillary region (around 1.5 cm), breaking at an angle of 90 degrees in the pre-auricular region, descending retrotragal, and outlining the ear from its posterior region to its upper portion (Figure 2). Subcutaneous detachment is done initially with the scalpel and then with scissors in the demarcated area.
The second step is the plication of the superficial muscle-aponeurotic system (SMAS), made with colorless nylon 4.0 (Figure 3). Starting the suture through the mandible branch, then in the anterior region, and finally in the posterior region, leaving the entire surface smooth and without sagging. The next step is the adhesion suture of the entire flap, made with monocryl 4.0, pulling gently without marking the skin too much (Figure 4). The adhesion points follow the same order as the SMAS, starting with the mandible branch.
After the excess skin is removed, adjusting with the drawing made previously, there may be the need to remove a little more or less. The skin is sutured with monocryl 4.0 and, finally, with a continuous intradermal suture performed with monocryl 5.0; there is no need for drains. The last step is liposuction of the subment, made by a small median incision in the subment. And the compressive dressing with gauze around the ear, padded gauze, and the elastic band. The dressing is renewed 24 hours after discharge (Figure 5).
RESULTS
Partial results are seen in the first few weeks, especially after lymphatic drainage. After a month, edema is no longer observed. In the long term, the surgery can be redone around 5 to 7 years, and since it does not change the hair implant, it can be done several times over the years without leaving stigmas, as seen in one year postoperative (Figures 6 and 7). The complications were much less, where the rare hematomas were restricted to small regions drained by 7-day transcutaneous puncture (12 cases). The main complaint is the persistence in elderly and post-bariatric patients of some skin in the central cervical region.
DISCUSSION
Facial rejuvenation must encompass several complementary forms of treatment and act effectively in all facial regions. The rising cosmiatric arsenal, with fillers added to the botulinum toxin, puts into question the broad coronal lifting, especially in younger patients. In older individuals, understanding the interaction between these complex anatomical changes is essential when choosing a surgical strategy, which can vary from periorbital treatment, through conservative frontal lifting, to radical liftings in this region2.
Facelift light is approached in this study as an alternative for the face middle and lower thirds treatment, with a standardized, reproducible mark; with a reduced scar, moderate detachment, plication of the SMAS and points of adhesion; as well as with natural results, few complications and early return of patients to daily activities.
Standardized preoperative marking facilitates the technique reproducibility with more accessible and safer learning compared to classic rhytidoplasty or aggressive detachments3. Since the most aggressive and profound approaches, or large detachments, bring an even higher risk of other complications, such as injuries to facial nerve branches and flaps suffering 4.
Several authors report that they have reduced the detachments’ amplitude and realized that results are equally good and very similar to those obtained with the broader and more generalized detachments used before. These are now reserved for cases of great skin flaccidity and for those who need large cervical degreasing associated with platysma plication5,6.
Another essential point of rhytidoplasty is the treatment of the superficial musculoaponeurotic system (SMAS) 5,7, as it has become essential during the performance of the facial lifting, since it determines the elevation and traction of the tissue planes, with long-term effects8. These techniques can be used, ranging from mobilization, plication, and repositioning, to subaponeurotic resections. In this context, the facelift light is performed with the standardized plication of the SMAS, without detachment and deep resections, to reduce the risk of injury to the subaponeurotic structures.
The use of adhesion points applied in the pre and behind-the-ear regions reduced to zero the incidence of large bruises requiring urgent surgical drainage9,10, making the use of drains unnecessary with the use of this technique.
Thus, the rejuvenation surgery of the face middle and lower thirds has been evolving to perform less invasive and less aggressive techniques, in order to reduce complications and provide an earlier return to the usual activities of patients8-12; without, however, compromising the occurrence of natural and satisfactory results to patients.
CONCLUSION
The facelift light technique was considered satisfactory due to the quality of the results obtained in this series, the low rate of complications, and the early return of patients to their activities.
REFERENCES
1. Menezes MVA, A bla LEF, Dutra LB, Junqueira AE, Ferreira LM. Modified minilifting results: prospective study. Rev Bras Cir Plást. 2010;25(2):285-90.
2. Tabatabai N, Spinelli HM. Limited incision nonendoscopic brow lift. Plast Reconstr Surg. 2007;119(5):1563-70.
3. Baker DC, Stefani WA, Chiu ES. Reducing the incidence of hematoma requiring surgical evacuation following male rhytidectomy: a 30-year review of 985 cases. Plastic Reconstr Surg. 2005 Dez;116(7):1973-85;discussion:1986-7.
4. Paul MD, Calvert JW, Evans GR. The evolution of the midface lift in aesthetic plastic surgery. Plast Reconstr Surg. 2006 Mai;117(6):1809-27.
5. Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976 Jul;58(1):80-8.
6. Saldanha OR, Azevedo SFD, Saldanha Filho OR, Saldanha CB, Chaves LO. Ritidoplastia com descolamento composto. Rev Bras Cir Plást. 2010;25(1):135-40.
7. Pitanguy I, Degand M, Ceravolo MP, Bos H. Considerações sobre nossa experiência com dissecção e plicatura do SMAS em meloplastia. Rev Bras Cir Plást. 1981;71(1):57-72.
8. Maloney BP, Schiebelhoffer J. Minimal-incision endoscopic face-lift. Arch Facial Plast Surg. 2000;2(4):274-8.
9. Destro MWB, Destro C, Baroudi R. Adhesion stitches in rhytidoplasty: a comparative study. Rev Bras Cir Plást. 2013;28(1):55-8.
10. Cló TXT, Ferraz Junior WFF, Leão CEG, Cló FX, Mourão LM, Leão LR. Perioperative systematization for the prevention of hematomas following face-lift procedures: a personal approach bases on 1,138 surgical cases. Rev Bras Cir Plást. 2019 Jan/Mar;34(1):2-9.
11. Aboudib JH, Pontes R, Amaral PB, Castro CC. Debate sobre ritidoplastias: "radicais ou econômicas?". Rev Bras Cir Plást. 2005;20(4):253-5.
12. Zani R, Fadul Junior R, Rocha MAD, Santos RA, Alves MCA, Ferreira LM. Facial nerve in rhytidoplasty: anatomic study of its trajectory in the overlying skin and the most common sites of injury. Ann Plast Surg. 2003 Set;51(3):236-42.
1. Isaac Furtado Clinic, Fortaleza, CE,
Brazil.
2. Hospital Geral de Fortaleza, Fortaleza, CE,
Brazil.
COLLABORATIONS IRF Analysis and/or data interpretation, Conception and design study, Writing - Original Draft Preparation
COLLABORATIONS NOS Writing - Review & Editing
Corresponding author: Isaac Rocha Furtado Avenida Dom Luís, 1233, Sala 606, Fortaleza, CE, Brazil. Zip Code: 60160.230 E-mail: dr.isaacfurtado@gmail.com
Article received: June 10, 2019.
Article accepted: July 15, 2020.
Conflicts of interest: none.













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter