

Original Article - Year 2020 - Volume 35 -
Breast region measurements: direct or indirect anthropometry?
Medidas da região mamária: antropometria direta ou indireta?
ABSTRACT
Introduction: Accurate female breast measurements are difficult due to the topography, volume, and projections present there. Therefore, this study aimed to compare breast region measurements obtained by direct (tape measurement) and indirect (computer-based photogrammetry) anthropometry.
Methods: This is a transversal study. Forty women were evaluated, aged 18-60 years, body mass index of <29.2kg/m² that had 12 anatomical marks on the breast region and arms. These points' union formed 7 linear segments and 1 angle for each hemibody, and 1 segment common to both hemibodies. The photographs obtained in a standardized way were measured using computer-based photogrammetry with Image ToolTM software. The same segments were also measured by direct anthropometry, using a tape measure. The Shapiro-Wilk test was used to assess whether each variable was normally distributed. The Pearson correlation test was applied to evaluate the correlation between different methods: the direct (tape measurement) and indirect (photogrammetry by Image ToolTM) anthropometry. The significance level adopted for statistical tests was 5% (p<0,05).
Results: Significant differences were found in the comparisons between the tape measurement and computer-based photogrammetry for all segments analyzed (p>0.05).
Conclusion: There is a correlation between the breast measurements obtained by direct (tape measurement) and indirect (photogrammetry by Image ToolTM software) anthropometry, especially the papilla measures.
Keywords: Breast; Anthropometry; Photogrammetry; Mammaplasty; Women; Surgery, Plastic.
RESUMO
Introdução: As medidas precisas dos seios femininos são difíceis de obter devido à
topografia, volume e projeções presentes. Portanto, este estudo teve como
objetivo comparar medidas da região mamária obtidas por antropometria direta
(fita métrica) e indireta (fotogrametria computadorizada).
Métodos: Este é um estudo transversal. Foram avaliadas 40 mulheres, com idades entre
18 e 60 anos, índice de massa corporal <29,2 kg / m², que tinham 12
marcas anatômicas na região das mamas e braços. A união desses pontos formou
7 segmentos lineares e 1 ângulo para cada hemicorpo, e 1 segmento comum a
ambos os hemicorpos. As fotografias obtidas de forma padronizada foram
mensuradas por fotogrametria computadorizada com o software Image
Tool®. Os mesmos segmentos também foram medidos por
antropometria direta, com fita métrica. O teste de Shapiro-Wilk foi usado
para avaliar se cada variável tinha uma distribuição normal. O teste de
correlação de Pearson foi aplicado para avaliar a correlação entre os
diferentes métodos: antropometria direta (medição com fita) e indireta
(fotogrametria por Image Tool®). O nível de significância
adotado para os testes estatísticos foi de 5% (p <0,05).
Resultados: Diferenças significativas foram encontradas nas comparações entre a fita
métrica e a fotogrametria computadorizada para todos os segmentos analisados
(p> 0,05).
Conclusão: Existe correlação entre as medidas dos seios da face obtidas pela
antropometria direta (medição com fita métrica) e indireta (fotogrametria
pelo software Image Tool®), principalmente nas medidas da
papila.
Palavras-chave: Mama; Antropometria; Fotogrametria; Mamoplastia; Mulheres; Cirurgia Plástica
INTRODUCTION
Accurate measurements of female breasts are challenging due to the topography, volume, and projections present there1. Therefore, linear breast reference parameters were created to directly analyze the size, shape and positioning1-5.
In clinical practice, breast measurements are done by direct anthropometry, usually using tape measure or compass. However, these measures may be altered due to respiratory oscillations or slight body positioning changes in body positioning6. Despite the limitations of direct breast anthropometric measurements, they have been the most widely used method for expressing and comparing mammaplasty results, both in scientific publications and in events (conferences, symposia, forums, etc.).
Given the need for a method that would overcome direct anthropometry limitations, some authors have proposed photogrammetry7-9. However, in the literature, the existing studies comparing photogrammetry and direct anthropometry are not specific for the breast region.
OBJECTIVE
This study compares breast region measurements obtained by direct (tape measurement) and indirect (computer-based photogrammetry, Image ToolTM software) anthropometry.
METHODS
The study was approved and conducted by the Research Ethics Committee of the Universidade Federal de São Paulo (UNIFESP) (1054/10). Written informed consent was obtained from all volunteers before their inclusion in the study.
Forty female volunteers, aged 18 to 60, body mass index (BMI) of <29.9kg/m², were included in the study, between June and December 2018. They were recruited from the Plastic Surgery Division Outpatient Service at UNIFESP. Each side of the thorax was separately analyzed, with a total of 80 hemibodies. Women who underwent a mastectomy, with a history of any type of conservative breast surgery, congenital or acquired chest deformities and severe breast ptosis in which the nipples cross a transverse line at the limit of the umbilicus were not included in the study.
Each volunteer was instructed to place their feet on predetermined marks on the floor with a 3 cm distance between their medial margins and remain in anatomical position, with the head in the Frankfurt position during measurements. The distance between the most posterior point of the volunteer’s feet and the photography background was 70cm.
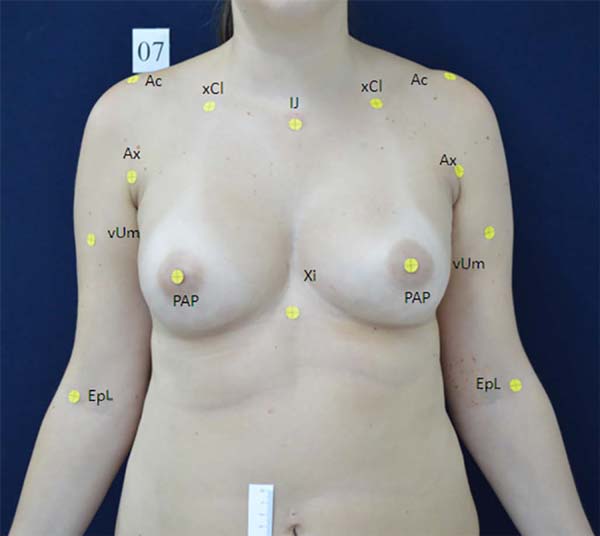
Self-adhesive labels with 0.6 cm diameter were used to mark the anatomical landmarks used in each hemibody. These landmarks in counterclockwise were: the center of the mammary papilla (PAP), the midpoint of the base of the xiphoid process (Xi), jugular notch center (IJ), half the distance between the jugular notch center and the acromion (xCl), lateral border of the acromion (Ac), the most cranial point of the fold in the anterior axillary line (Ax) and the anterior projection of the lateral epicondyle (EpL) (Figure 1).
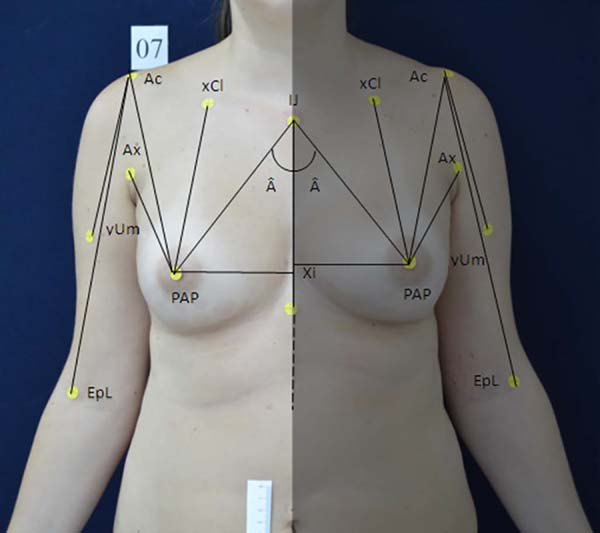
From these points, 8 line segments and 1 angle per hemibody were formed. Only the segment passing through the anterior median line, from the center of the jugular notch to the base of the xiphoid process (segment IJ-Xi), was common to both hemibodies. The other 7 segments were formed bilaterally: center of the mammary papilla to the anterior median line, passing through the base of the xiphoid process (segment PAP-Xi), center of the mammary papilla to jugular notch center (segment IJ-PAP), the center of the mammary papilla to half the distance between the jugular notch center and the acromion (segment xCl-PAP), the center of the mammary papilla to the lateral border of the acromion (segment Ac-PAP), the center of the mammary papilla to most cranial point of the fold in the anterior axillary line (segment Ax-PAP), lateral border of the acromion to the anterior projection of the lateral epicondyle (segment Ac-EpL), half the distance between the acromion and the lateral epicondyle to the lateral epicondyle (Ac-yUm). The confluence of the segments (IJ-Xi) and (IJ-PAP) formed the  angle (Figure 2).
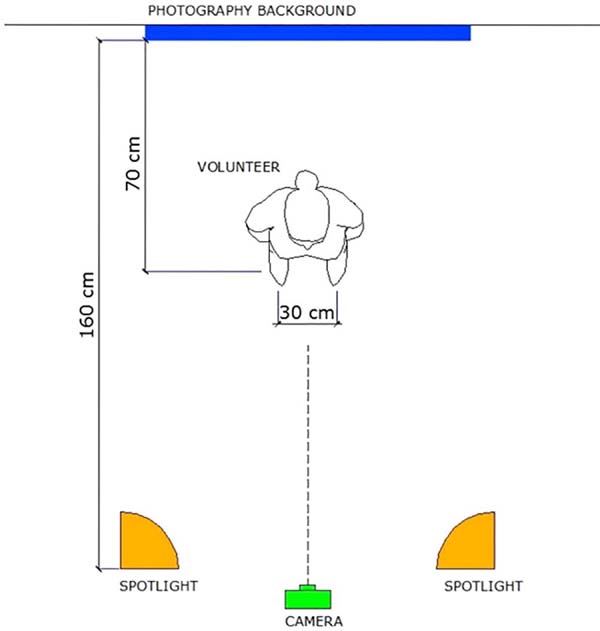
We used a SonyTM DSC-W120 digital camera, with the distance from the lens to the voluntary determined by the framework, without zooming, on a tripod with bubble level. All photographs were standardized with 7.0 megapixels and JPEG format. Two spotlights were positioned at the height of 1.50m from the floor and at a distance of 1.60m from the photography background, convergently directed, each one angled at 45º to the blue photography background (Figure 3).
The breast region’s photographic framing was delimited superiorly by a transverse line at the gnathion (Gn) and inferiorly by a transverse line at the bottom of the navel. A ruler with a millimeter scale 0-10cm long was attached to the volunteer’s right mesogastric region to proceed to the Image ToolTM 3.0 software calibration. A centimeter-scale was chosen for digital photogrammetry.
Direct anthropometry was performed with a tape measure with a scale in millimeters. The tape measure was placed in the label’s center and directed to the label’s center on the opposite side of the selected segment. For measuring the α angle, a dotted line was drawn using a dermographic pen and a metallic ruler, crossing over the segment IJ-Xi and another one over the segment IJ-Pa. Then, a 180° clear plastic protractor was placed in the center of the label of the jugular notch (IJ), and the measure corresponding to the angle was obtained. The same evaluator collected all indirect (photography and software) and direct anthropometry data.
Statistical analysis
Data will be analyzed using GraphPad Prism 6.0 for Windows. Variables were tested for normal distribution by the Shapiro-Wilk test. Data are presented as mean and SD. The Pearson correlation test was applied to evaluate the correlation between the direct (tape measurement) and indirect (photogrammetry by Image ToolTM software) anthropometry, considering weak correlation (0.20 to 0.39), moderate correlation (0.40 to 0.69), a strong correlation (0.70 to 0.89) and very strong correlation (0.9 to 1). A significance level of 5% (p<0.05) was adopted to interpret the data.
RESULTS
The study included 80 breasts of 40 female volunteers with a mean age of 29.1 (±10.3) years old, weight of 63.4 (±5.4), height of 1.57 (±0.1) and BMI of 25.7 (±2.2). The prevalence of white race was 65%, black 2.5%, and others 32.5%. Table 1 shows the clinical characteristics of all volunteers.
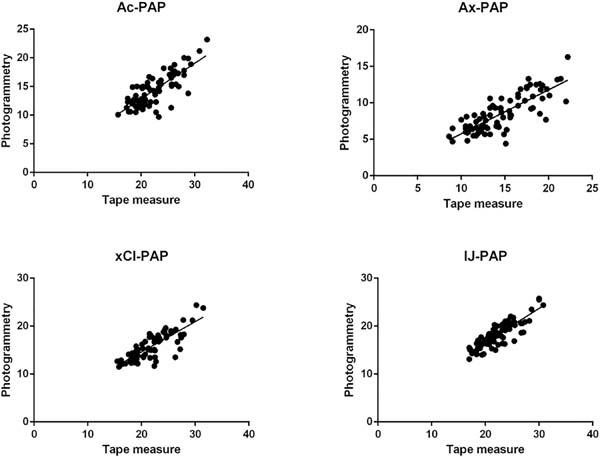
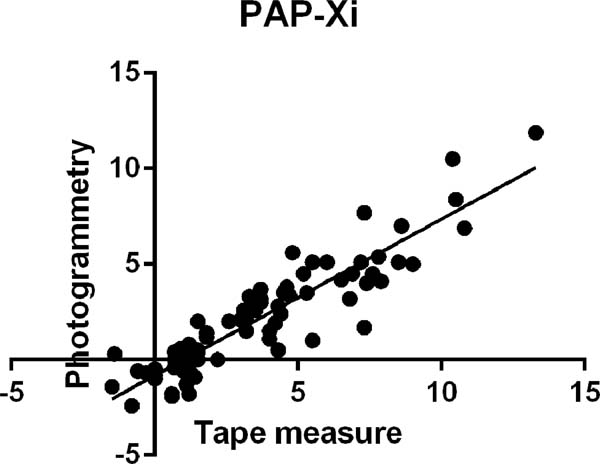
The means of segments obtained using the tape measure (direct anthropometry measurements) and photogrammetry by Image ToolTM software (indirect anthropometric measurements) were 16.35 (±1.14) and 12.90 (±1.69) of IJ-Xi, 11.16 (±1.07) and 10.98 (±1.30) of PAP-Xi, 22.08 (±3.08) and 18.24 (±2.65) of IJ-PAP, 21.46 (±3.54) and 15.66 (±2.82) of xCl-PAP, 22.00 (±3.45) and 14.29 (±2.82) of Ac-PAP, 14.44 (±3.28) and 8.57 (±2.52) of Ax-PAP, 29.12 (±1.58) and 24.53 (±1.91) of Ac-EpL, 14.49 (±0.95) and 12.30 (±1.00) of Ac-yUm, and 29.90 (±2.91) and 37.82 (±4.60) of  angle. The measurements of all segments obtained using the tape measure (direct anthropometry measurements) showed significant differences when compared with photogrammetry by Image ToolTM software (indirect anthropometric measurements) (Table 2).
| Segments | Tape measure | Photogrammetry | r | CI | p value |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | ||||
| IJ-Xi | 16.35 ± 1.14 | 12.90 ± 1.69 | 0.64 | 0.50 to 0.76 | < 0.0001 |
| PAP-Xi | 11.16 ± 1.07 | 10.98 ± 1.30 | 0.91 | 0.86 to 0.94 | < 0.0001 |
| IJ-PAP | 22.08 ± 3.08 | 18.24 ± 2.65 | 0.86 | 0.78 to 0.90 | < 0.0001 |
| xCl-PAP | 21.46 ± 3.54 | 15.66 ± 2.82 | 0.83 | 0.75 to 0.88 | < 0.0001 |
| Ac-PAP | 22.00 ± 3.45 | 14.29 ± 2.82 | 0.79 | 0.69 to 0.86 | < 0.0001 |
| Ax-PAP | 14.44 ± 3.28 | 8.57 ± 2.52 | 0.79 | 0.70 to 0.86 | < 0.0001 |
| Ac-EpL | 29.12 ± 1.58 | 24.53 ± 1.91 | 0.66 | 0.52 to 0.77 | < 0.0001 |
| Ac-yUm | 14.49 ± 0.95 | 12.30 ± 1.00 | 0.64 | 0.49 to 0.75 | < 0.0001 |
| Â angle | 29.90 ± 2.91 | 37.82 ± 4.60 | 0.46 | 0.27 to 0.62 | < 0.0001 |
SD: Standard deviation; r: Pearson correlation; CI: Confidence interval; IJ-Xi: Segment from the jugular notch center to the base of the xiphoid process; PAP-Xi: Center of the mammary papilla to anterior median line, passing through the base of the xiphoid process; IJ-PAP: Center of the mammary papilla to jugular notch center; xCl-PAP: Center of the mammary papilla to half the distance between the jugular notch center and the acromion; Ac-PAP: Center of the mammary papilla to lateral border of the acromion; Ax-PAP: Center of the mammary papilla to most cranial point of the fold in the anterior axillary line; Ac-EpL: Lateral border of the acromion to anterior projection of the lateral epicondyle; Ac-yUm: Half the distance between the acromion and the lateral epicondyle to the lateral epicondyle; Â angle: Confluence of the segments (IJ-Xi) and (IJ-PAP).
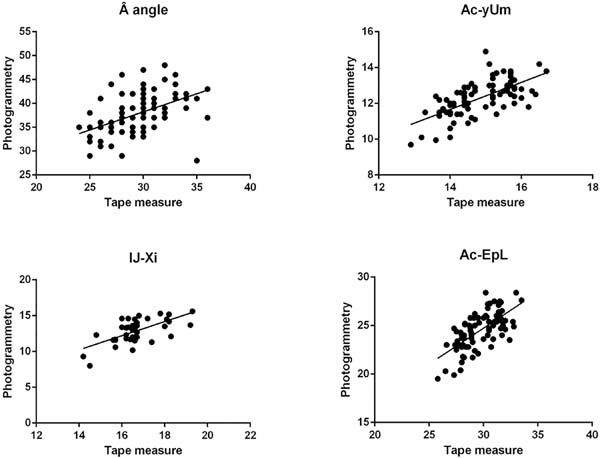
There was a moderate positive and statistically significant correlation between the measures: Â angle (r=0.46; p<0.0001), Ac-yUm (r=0.64; p<0.0001), IJ-Xi (r=0.64; p<0.0001) and Ac-EpL (r=0.66; p<0.0001) (Table 2 and Figure 4); strong positive and statistically significant correlation between the measures: Ac-PAP (r=0.79; p<0.0001), Ax-PAP (r=0.79; p<0.0001), xCl-PAP (r=0.83; p<0.0001) and IJ-PAP (r=0.86; p<0.0001) (Table 2 and Figure 5); and very strong positive and statistically significant correlation between the measure: PAP-Xi (r=0.91; p<0.0001) (Table 2 and Figure 6).
DISCUSSION
Breasts are considered a symbol of femininity, sensuality, and motherhood; therefore, they play a fundamental role in women’s physical and mental health10. In 1955, Penn2 collected measurements from 150 women; only 20 considered having symmetrical and aesthetically perfect breasts. This way, an attempt was made to set a normal standard for breast measures. Since then, several authors have developed protocols for direct breast anthropometric measurements1-5. When used the same anthropometric points for direct measurement of the breast region, using different measuring instruments (compass and metric tape), there may be differences in the measures found6. Nechala et al., in 19998, have compared direct anthropometry with photogrammetry for face measurements and concluded that there was no consensus on determining the best measurement method.
Given the lack of consensus of photogrammetry in different body areas, this study aimed to investigate the differences between measurements obtained by direct (tape measurement) and indirect (digital photogrammetry) anthropometry of the breast region, a subject of significant importance in plastic surgery. The standardization of positions, relative measurements, and photographic angles and markers on the anthropometric points and/or anatomical landmarks bring reliability and reproducibility to a scientific study11-15. The systematization and standardization of photographic framing, distance, and height of the camera and reflectors so as patient positioning are needed procedures for sequenced evaluations, for example, for pre- and postoperative comparisons, thereby allowing validating the comparison of techniques and results, preserving the scientific rigor13.
An alternative method is an indirect anthropometry using computer-based photogrammetry, which performs the measurement of photographs with graphic software aid and does not require the patient’s physical presence for data collection8,9. This method allows centesimal precision, reducing errors, besides enabling measurements over time. Thus, it is possible to compare pre- and postoperative differences quantitatively.
The average time spent with data collection for each volunteer, from the beginning to the end of the measurement interview was 34 minutes, 10 minutes spent only for measurements with a tape measure. Four volunteers reported discomfort while performing the measurements. This event did not allow a tacit recommendation of scientific rigor concerning the need of 2 intra-evaluator measurements to verify the accuracy or the degree of reproducibility of the method used.
The determining factor for the use of the labels was the fact that they minimize discomfort and pain as felt when marking with pen the center of the mammary papilla. Christie et al., in 200516, used this same tactic, reporting that the use of self-adhesive labels at the time of the photography sessions lessened the discomfort of demarcating anthropometric points besides reducing the chances of errors.
According to Westreich, in 19971, the most challenging measurements were the segment from the axilla to the center of the mammary papilla, and the segment of the mammary fold’s lateral point since markings made on soft tissue are too much variable to be included in studies of breast measurements. These markings can vary from woman to woman and change even with the patient’s slight movements, and may, therefore, be inaccurate, which was also highlighted in the study by Smith et al. (1986)4.
Until now, the breasts are measured by digital photography. However, the studies are not clear, and standardization should be made for the breast measurement. The literature used direct anthropometry,1,4,6,7) or the studies evaluated mastectomy and voluminous breast17,18. The Pearson correlation test demonstrated that measures that are directly related to the breast presented a strong or very strong correlation. However, measurements related to the arm and chest showed a moderate correlation. Therefore, for measurements related to the breast, especially the papilla, the use of tape measure and digital photography performed by Image ToolTM could be an option in the evaluation of breasts in women. Thus, the discomfort reported by volunteers could be minimized because digital photography is faster than a tape measure.
Although clinical photographs have been taken in 5 different positions - anteroposterior (AP), right and left profiles and right and left oblique, according to literature guidelines1,14,15) - in this study, given the fact that all points determined for evaluation could also be evaluated in frontal position, only the AP position was standardized. How was demonstrated by Quieregatto et al., in 201519, our results demonstrate that the association between direct and indirect anthropometry could not be indiscriminately used. The present study demonstrates two forms to evaluate the healthy breast. We are looking for the best way to suggest breast evaluation. Other studies are necessary to compare different breast measurement software.
CONCLUSION
There was a correlation between direct (tape measurement) and indirect (photogrammetry by Image ToolTM software) anthropometry in the segments that directly involve the breast, especially the papilla. However, although there is a correlation between the measurements, they are statistically different when obtained by direct and indirect anthropometry
REFERENCES
1. Westreich M. Anthropomorphic breast measurement: protocol and results in 50 women with aesthetically perfect breasts and clinical application. Plast Reconstr Surg. 1997 Aug;100(2):468-79.
2. Penn J. Breast reduction. Br J Plast Surg. 1955 Jan;7(4):357-71.
3. Brown TP, Ringrose C, Hyland RE, Cole AA, Brotherston TM. A method of assessing female breast morphometry and its clinical application. Br J Plast Surg. 1999 Jul;52(5):355 - 9.
4. Smith Junior DJ, Palin Junior WE, Katch VL, Bennett JE. Breast volume and anthropomorphic measurements: normal values. Plast Reconstr Surg. 1986 Sep;78(3):331-5.
5. Odo LM, Guimarães PA, Lemos ALA, Pozzobon AV, Sabino Neto M, Ferreira LM. Avaliação do tratamento cirúrgico da assimetria mamária por meio de medidas lineares. Arq Catarin Med. 2009;38(Suppl 1):43-5.
6. Quieregatto PR, Hochman B, Ferrara SF, Furtado F, Liebano RE, Sabino Neto M, et al. Anthropometry of the breast region: how to measure?. Aesthetic Plast Surg. 2014 Mar;38(2):344-9.
7. Ward CM. An analysis, from photographs, of the results of four approaches to elongating the columella after repair of bilateral cleft lip. Plast Reconstr Surg. 1979 Jul;64(1):68-75.
8. Nechala P, Mahoney J, Farkas LG. Digital two-dimensional photogrammetry: a comparison of three techniques of obtaining digital photographs. Plast Reconstr Surg. 1999 Jun;103(7):1819-25.
9. Hochman B, Castilho HT, Ferreira LM. Padronização fotográfica e morfométrica na fotogrametria computadorizada do nariz. Acta Cir Bras. 2002 Jul/Aug;17(4):258-66.
10. Pozzobon AV, Sabino Neto M, Veiga DF, Abla LE, Pereira JB, Biasi TL, et al. Magnetic resonance images and linear measurements in the surgical treatment of breast asymmetry. Aesthetic Plast Surg. 2009 Mar;33(2):196-203.
11. Farkas LG, Bryson W, Tech B, Klotz J. Is photogrammetry of the face reliable?. Plast Reconstr Surg. 1980 Sep;66(3):346-55.
12. McCausland TM. A method of standardization of photographic viewpoints for clinical photography. J Audiov Media Med. 1980 Jul;3(3):109-11.
13. Rodrigues OR, Geraldelli S, Minamoto H, Schmidt Junior AF. A fotografia em ciências biológicas: uso no ensino e na documentação científica. Acta Cir Bras. 1995;10(4):173-82.
14. Gherardini G, Matarasso A, Serure AS, Toledo LS, DiBernardo BE. Standardization in photography for body contour surgery and suction-assisted lipectomy. Plast Reconstr Surg. 1997 Jul;100(1):227-37.
15. Hochman B, Nahas FX, Ferreira LM. Fotografia aplicada na pesquisa clínico-cirúrgica. Acta Cir Bras. 2005;20(Suppl 2):19-25.
16. Christie D, Sharpley C, Curtis T. Improving the accuracy of a photographic assessment system for breast cosmesis. Clin Oncol (R Coll Radiol). 2005 Feb;17(1):27-31.
17. Reddy JP, Lei X, Huang SC, Nicklaus KM, Fingeret MC, Shaitelman SF, et al. Quantitative assessment of breast cosmetic outcome after whole-breast irradiation. Int J Radiat Oncol Biol Phys. 2017 Apr;97(5):894-902.
18. Nicoletti G, Scevola S, Faga A. Is breast reduction a functional or a cosmetic operation? Proposal of an objective discriminating criterion. J Plast Reconstr Aesthet Surg. 2009 Dec;62(12):1644-6.
19. Quieregatto PR, Hochman B, Furtado F, Ferrara SF, Machado AFP, Sabino Neto M, et al. Photographs for anthropometric measurements of the breast region. Are there limitations?. Acta Cir Bras. 2015 Jul;30(7):509-16.
1. Federal University of São Paulo, São
Paulo, SP, Brazil.
PRQES Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Software, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing
AFPM Analysis and/or data interpretation, Conception and design study, Data Curation, Investigation, Methodology, Software, Writing - Review & Editing
SF Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Formal Analysis, Methodology, Project Administration, Realization of operations and/or trials, Supervision, Writing - Original Draft Preparation, Writing - Review & Editing
AAQES Data Curation, Formal Analysis, Investigation, Software, Visualization
FF Analysis and/or data interpretation, Conception and design study, Conceptualization, Formal Analysis, Project Administration, Resources, Software, Supervision, Writing - Review & Editing
REL Analysis and/or data interpretation, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Methodology, Supervision, Validation, Writing - Review & Editing
MSN Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Investigation, Methodology, Supervision, Visualization, Writing - Original Draft Preparation
LMF Analysis and/or data interpretation, Conceptualization, Final manuscript approval, Investigation, Supervision, Writing - Review & Editing
Corresponding author: Paulo Rogério Quieregatto do Espirito Santo, Rua Napoleão de Barros, 715, 4º andar, Vila Clementino, São Paulo, SP, Brazil. Zip Code: 04023-002, E-mail: contato@pauloquieregatto.com.br
Article received: March 29, 2020.
Article accepted: June 04, 2020.
Conflicts of interest: none.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter