

Original Article - Year 2020 - Volume 35 -
Reconstruction of nasal defects using the Rieger flap
Reconstrução de defeitos nasais utilizando o retalho de Rieger
ABSTRACT
Introduction: the reconstruction of skin defects in the distal part of the nose is always a challenge. The dorsal nasal flap, initially described by Gillies, was unveiled when Rieger, in 1967, described the use of a modified rotation flap that used the redundant skin of the glabella to repair full-thickness defects of the lower half of the nose of equal or greater size of 2 cm, allowing reconstruction in a single surgical time.
Methods: A retrospective study was carried out, selecting patients who had basal cell carcinoma, in the middle and/or lower third of the nose, who were treated at the Plastic Surgery outpatient clinic of the Plastic Surgery Service Prof. Dr. Oswaldo de Castro, in the period from 2017 to 2019.
Results: The total number of patients was six, with ages ranging from 64 to 95 years, with an average of 80.67 years. Five of these patients were male, with only one female. There were no complications during or after the procedures. Also, there were no cases of infection, bleeding, hematoma, dehiscence, or necrosis of the flap.
Conclusion: the Rieger flap is a good option for cases of reconstruction of defects located in the lower half of the nose; it is performed in a single moment, is easy to perform, and has a high level of patient satisfaction. It provides an adequate result aesthetics of the reconstructed area, in texture and color, through the use of specific tissues for the nasal covering.
Keywords: Surgical flaps; Nose; Reconstructive surgical procedures; Nose neoplasms; Carcinoma, Basal cell.
RESUMO
Introdução: A reconstrução de defeitos cutâneos na porção distal do nariz sempre é um desafio. O retalho de dorso nasal, originalmente descrito por Gillies, ficou conhecido quando Rieger, em 1967, descreveu o uso de um retalho de rotação modificado que utilizava a pele redundante da glabela para reparar defeitos de espessura total da metade inferior do nariz com tamanho igual ou menor a 2cm, permitindo a reconstrução em somente um tempo cirúrgico.
Métodos: Um estudo retrospectivo foi realizado, selecionando pacientes que foram atendidos no ambulatório de Cirurgia Plástica do Serviço de Cirurgia Plástica Prof. Dr. Oswaldo de Castro, no período de 2017 a 2019, que apresentavam carcinoma basocelular, em região de terço médio e/ou inferior do nariz.
Resultados: O número total de pacientes foi de seis, com idade variando entre 64 a 95 anos, com média de 80,67 anos. Cinco destes pacientes eram do sexo masculino, sendo somente uma do sexo feminino. Não houve intercorrências durante ou após os procedimentos. Ainda, não ocorreram casos de infecção, sangramento, hematoma, deiscência ou necrose do retalho.
Conclusão: O retalho de Rieger é uma boa opção para casos de reconstrução de defeitos localizados em metade inferior do nariz, sendo realizado em tempo único, de fácil execução e com alto nível de satisfação dos pacientes, fornecendo um adequado resultado estético da área reconstruída, em textura e cor, por utilizar tecidos próprios da cobertura nasal.
Palavras-chave: Retalhos cirúrgicos; Nariz; Procedimentos cirúrgicos reconstrutivos; Neoplasias nasais; Carcinoma basocelular
Introduction
Reconstructing skin defects on the distal portion of the nose is always a challenge. Irregularities in color, texture, skin thickness and contour are easily noticeable1,2. The dorsal nasal flap, initially described by Gillies in 19203, became known when Rieger in 19674 described the use of a modified rotation flap that used the redundant skin of the glabella to repair full-thickness defects of the lower half of the nose 2 cm or less, allowing reconstruction in a single surgical time2,4. Initially, the flap was randomized; however, Marchac, 19705, modified it, creating an axial pattern based on angular artery perforators. Several other authors published modifications to the technique, allowing its refinement.
OBJECTIVE
The objective of this work is to demonstrate a series of six cases of reconstruction of nasal defects using the Rieger flap, performed by Prof. Dr. Oswaldo de Castro Plastic Surgery Service, during the period from 2017 to 2019.
METHODS
A retrospective study was carried out, selecting medical records of patients who had basal cell carcinoma in the region of the middle and/or lower nose and who were treated at the private office of Plastic Surgery of the Prof. Dr. Oswaldo de Castro, under the coordination of Dr. Antônio Egidio Rinaldi, in the period from 2017 to 2019.
The term of free and informed consent was applied to all patients, including authorization for the dissemination and use of images for academic purposes. The study followed the principles of the Declaration of Helsinki and Resolution 466/2012 of the National Health Council.
After resection of the nasal tumor, a rotation flap is made with its pedicle laterally based on the branches of the angular artery, with a relaxation line. From the created defect, a curvilinear line is drawn that passes at the transition between the nasal wall of the nose and the cheek, then extends superiorly to the region of the glabella. The glabellar extension should correspond approximately 1 ½ times the vertical height of the defect (Figure 1).
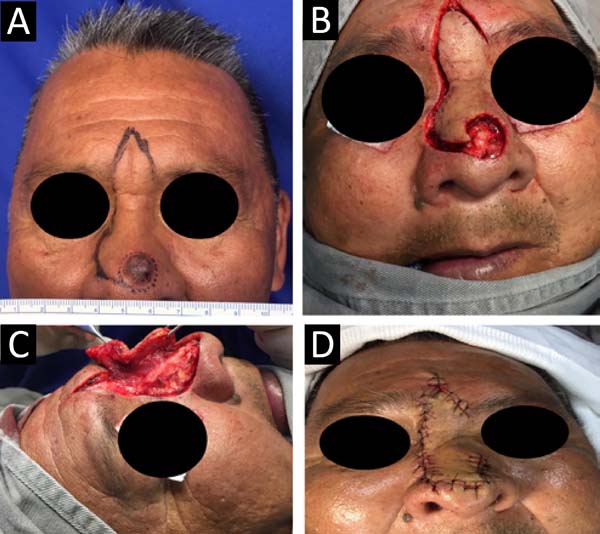
After infiltrating a local anesthetic solution containing 2% lidocaine plus epinephrine at a concentration of 1: 200,000 IU, the flap area in the glabellar region is elevated in the subcutaneous plane and the others in the submuscular plane. After release and rotation, it is essential to check for differences in skin thickness and significant distortions in the wings and nasal tip. Simple stitches with mono nylon 5- 0 are used to secure the flap, and the donor area in the glabella is closed by primary suturing, and a V-Y advance may be necessary. The sutures are removed after seven days.
RESULTS
The total number of patients was six, with ages ranging from 64 to 95 years, with an average of 80.67 years. Five of these patients were male, with only one female (Table 1).
| Patient | Age (years) | Gender | Tumor location (aesthetic subunits of the nose) | Defect (cm) |
|---|---|---|---|---|
| 1 | 93 | M | nasal tip | 1.0 |
| 2 | 95 | F | lower back. left side. left nasal wing | 3.0 |
| 3 | 78 | M | lower back. right nasal wing | 1.5 |
| 4 | 64 | M | nasal tip | 2.5 |
| 5 | 82 | M | nasal tip | 2.0 |
| 6 | 72 | M | nasal tip | 1.0 |
| Média | 80.67 | 1.8 |
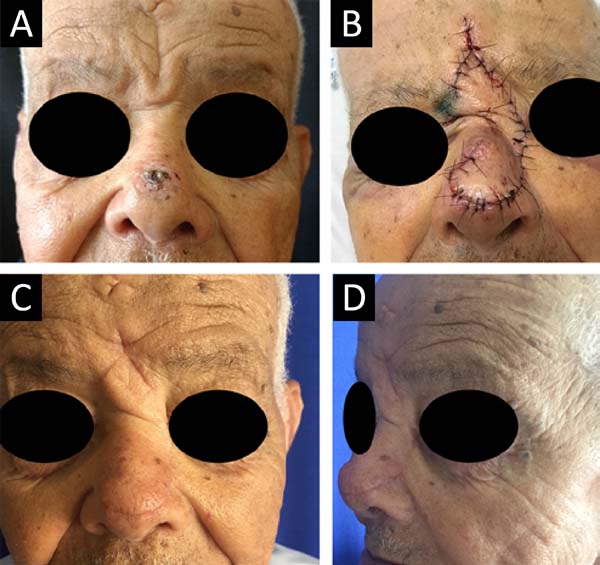
The size of the defects varied from 1.5 to 3 cm, with an average of approximately 2.0 cm. Patient 2 presented an injury that extended beyond the lower third of the nose, which involved the entire lower half, requiring a nasogenian flap to complement the closure of the defect superiorly (Figure 2). Furthermore, patient 3 presented a lesion in the right malar region, where the open area was closed with an advancement flap (Figure 3).
There were no complications during or after the procedures. Besides, there were no cases of infection, bleeding, hematoma, dehiscence, or necrosis of the flap. Even so, all the pathological examinations showed surgical margins free of neoplasia. No case required a second surgical procedure for refinement. The patients, without exception, were satisfied with the aesthetic result, a question asked during each postoperative consultation (Figures 4, 5 and 6).
DISCUSSION
The nose is the most exposed aesthetic unit of the face, with the lower part of the nose being the most vulnerable to ultraviolet radiation and trauma. Any irregularities in the color, texture, thickness, and contour of the skin in this region are easily noticed. Furthermore, the intense activity of the sebaceous glands in these areas produces an increase in scar tissue. Therefore, the defects located in this region, the nasal tip and the alar region, are the most difficult during reconstruction1,6,7.
The Rieger flap is a modified rotation flap that uses the redundant skin of the glabella, with its pedicle laterally based on the medial corner of the eye, allowing reconstruction by recruiting adjacent tissues that have similar characteristics, easily and fast. It is also performed in a single surgical time, lasting approximately 30 to 50 minutes, and only local anesthesia can be used, with a high level of patient satisfaction, being an alternative to the paramedian flap2,8.
The Rieger flap is better indicated in elderly patients who have greater skin laxity, both in the glabella and nasal skin, since it ensures better rotation of the flap, in addition to making the glabellar scar hidden in the rhytids. The technique is best used in the correction of skin defects located centrally in the nasal tip; however, it is possible to use this flap to correct injuries in regions of the back and also of the lateral nasal wall2,9.
It is important to emphasize that, although the Rieger flap was initially described for use in partial-thickness lesions, up to 2 cm, even defects higher than 2 cm can be corrected with this flap, at the expense of greater head displacement of the margin, the nostril and the nasal tip. Therefore, we should always try to respect the 1 cm distance from the wing margin to avoid problems in the function of the external nasal valve, as well as significant distortions1,2. In 2010, Wentzell8 demonstrated that the dorsal nasal flap could be used for full-thickness defects, without the need for cartilage grafts or mucosa flaps.
CONCLUSION
The Rieger flap is a good option for cases of reconstruction of defects located in the lower half of the nose, since it is performed in a single moment, is easy to execute and has a high level of patient satisfaction, providing a satisfactory aesthetic result of the reconstructed area, in texture and color, to use specific tissues for the nasal covering.
COLLABORATIONS
|
FLD |
Analysis and/or data interpretation, conception and design study, conceptualization, data curation, final manuscript approval, formal analysis, funding acquisition, investigation, methodology, project administration, realization of operations and/or trials, resources, supervision, validation, visualization, writing - original draft preparation, writing - review & editing. |
|
AER |
Analysis and/or data interpretation, conception and design study, conceptualization, data curation, final manuscript approval, formal analysis, investigation, methodology, project administration, realization of operations and/or trials, resources, supervision, validation, visualization, writing - original draft preparation, writing - review & editing. |
REFERENCES
1. Eren E, Beden V. Beyond Rieger’s original indication; the dorsal nasal flap revisited. J Craniomaxillofac Surg. 2014 Jul;42(5):412-6. DOI: https://doi.org/10.1016/j.jcms.2013.05.031
2. Baker SR. Retalhos de rotação. In: Baker SR. Retalhos locais em reconstrução facial. Rio de Janeiro: Di Livros; 2009. p. 109-33.
3. Gillies HD. Plastic surgery of the face. London: Oxford Medical Publishers; 1920.
4. Rieger RA. A local flap for the repair of the nasal tip. Plast Reconstr Surg. 1967;40:147-9.
5. Marchac D. Lambeau de rotation fronto-nasal. Ann Chir Plast Esthet. 1970;15:44-9.
6. Raschke GF, Rieger UM, Bader RD, Kirschbaum M, Eckardt N, Schultze-Mosgau S. Evaluation of nasal reconstruction procedures results. J Craniomaxillofac Surg. 2012;40(8):732-49. DOI: https://doi.org/10.1016/j.jcms.2012.01.023
7. Yong HK, Hyung WY, Seum C, Yoon KC. Reconstruction of cutaneous defects of the nasal tip and alar by two different methods. Arch Craniofac Surg. 2018 Dec;19(4):260-3. DOI: https://doi.org/10.7181/acfs.2018.02271
8. Wentzell MJ. Dorsal nasal flap for reconstruction of full-thickness defects of the nose. Dermatol Surg. 2010 Jul;36(7):1171-8. DOI: https://doi.org/10.1111/j.1524-4725.2010.01603.x
9. Redondo P, Bernad I, Moreno E, Ivars M. Elongated dorsal nasal flap to reconstruct large defects of the nose. Dermatol Surg. 2017 Aug;43(8):1036-41. DOI: https://doi.org/10.1097/DSS.0000000000001149
1. Serviço de Cirurgia Plástica Prof. Dr. Oswaldo de Castro, Cirurgia Plástica, São
Paulo, SP, Brazil.
Corresponding author: Filipe Lopes Decusati Praça Santa Terezinha, nº 20 - Tatuapé, São Paulo, SP, Brazil Zip Code 03308-070 E-mail: decusati@gmail.com
Article received: December 10, 2019.
Article accepted: February 22, 2020.
Conflicts of interest: none.
Institution: Instituição: Clínica Plastiquè, Tatuapé, São Paulo, SP, Brazil.














 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter