

Case Report - Year 2020 - Volume 35 -
Association of the Tripier myocutaneous flap to scapha cartilage graft: a surgical resource for reconstruction of full thickness defects of lower eyelids
Associação do retalho miocutâneo de Tripier a enxerto de cartilagem da escafa: um recurso cirúrgico para reconstrução de defeitos de espessura total da pálpebra inferior
ABSTRACT
The reconstruction of the secondary lower eyelid to a resection of skin cancer is a challenging surgical procedure that must be carefully planned with regards to issues related to lamella and extension of the resection. We present the case of a 69-year-old male patient who, after oncologic resection, presented a total thickness defect greater than 60% in the lower eyelid. For reconstruction, it was indicated that the use of Tripier's unipedic myocutaneous flap with scapha cartilage graft produced favorable results, which confirms that it is worthwhile using these techniques when planning lower eyelid reconstruction.
Keywords: Basal cell carcinoma; Skin neoplasia; Myocutaneous flap; Ear cartilage; Eyelids.
RESUMO
A reconstrução da pálpebra inferior secundária à ressecção de câncer de pele é um desafio cirúrgico e sua abordagem deve ser planejada por lamelas e extensão da ressecção. Apresentamos o caso de paciente do sexo masculino, 69 anos, que após a ressecção oncológica apresentou defeito de espessura total maior de 60% na pálpebra inferior. Para reconstrução foi indicada a associação do retalho miocutâneo unipediculado de Tripier com enxerto de cartilagem da escafa obtendo resultados favoráveis, mostrando que a associação destas técnicas é uma boa prática na hora de planejar a reconstrução da pálpebra inferior.
Palavras-chave: Carcinoma basocelular; Neoplasias cutâneas; Retalho miocutâneo; Cartilagem da orelha; Pálpebras
INTRODUCTION
Basal cell carcinoma (BCC) is the most common cancer among humans. In Brazil, it is estimated that there are 165,580 new cases of non-melanoma skin cancer per year 1. Its growth is slow and rarely produces metastasis. However, when located on the eyelids, reconstruction after surgical treatment can pose a challenge to the plastic surgeon. The lower eyelid reconstruction should be planned to follow its anatomical limit; particularly, reconstructing the anterior and posterior lamella as two independent structures. Hence, the different prevailing techniques for either procedure should be studied, and there must be a safety recommendation regarding using both to optimize aesthetic results while preserving the functionality of either procedure2.
Within the lower eyelid reconstruction techniques, the Tripier myocutaneous flap offer several advantages; it is well known to be a good option for anterior lamella cover, which can be associated with cartilage grafts for posterior lamella reconstruction with or without mucosa cover.
OBJECTIVE
To report a case of lower eyelid reconstruction with the association of the Tripier myocutaneous flap to scapha cartilage graft and demonstrating a therapeutic option in reconstructions of defects of total thickness and extensions over 60% of the lower eyelid.
CASE REPORT
We present the case of a 69-year-old male patient diagnosed with nodular basal cell carcinoma recurring in the lower right eyelid. He was referred for resection with freezing through horizontal cuts (en face or CCPDMA) intraoperatively at the Hospital AC - Camargo Cancer Center.
Under general anesthesia, in the dorsal decubitus position and with ophthalmic protection with ointment, the edges of the lesion were marked with 4 mm of safety to be sent for freezing. After resection by hemostatic infiltration, the freezing reportedly compromised lateral and deep margins that required enlargement.
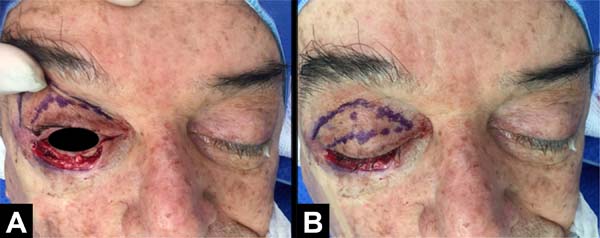
After obtaining free margins, the final defect showed a loss of lower eyelid continuity affecting 70% of its extension, covering skin, tarsal plate, and conjunctiva, from the lateral corner to the medial corner therearound. The final size of the defect was 3.0 x 0.5 cm (Figure 1).
For the reconstruction of the defect, a myocutaneous Tripier monopediculated lateral flap was chosen, using an advancing flap of the conjunctiva and an auricular scapha cartilage graft.
The flap was marked on the ipsilateral upper eyelid similarly to a blepharoplasty marking. The lower flap edge in the eyelid groove and the upper edge were marked leaving 1 cm of flap width corresponding to the excess skin amount, without compromising ocular occlusion; in the lateral corner, a 0.5-cm wide base was preserved. Using local infiltration, the myocutaneous flap was raised from the medial corner, leaving it pediculated at the base. The defect was sutured using a 6-0 Mononylon thread continuously.
After local infiltration, we obtained a fragment of cartilage and perichondrium, from the right scaphoid fossa using a previous approach, with the dimensions of the new tarsal plate being 3 cm long and 4 mm wide. The skin of the scaphoid was sutured with 4-0 Mononylon thread. The scapha cartilage graft was positioned so that its upper edge was at the level of the lower sclerocorneal limb, fixed with two points of 5-0 Mononylon at the lateral end using the lateral cantal ligament and two points in the medial portion, fixed to the tarsus. After fixation, the upper portion of the Tripier flap was sutured to the upper portion of the conjunctiva flap using Vicryl Rapid 6-0, supported on the cartilage graft (Figures 2 and 3).

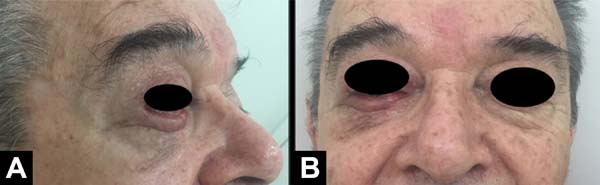
The patient recovered satisfactorily after reconstruction, without recurrence of the lesion and showing adequate aesthetic and functional results of the lower eyelid (Figure 4). There was adequate eyelid occlusion and no complaints of dry eye. No physiotherapy was indicated.
DISCUSSION
The reconstruction of the lower eyelid should be planned to follow its anatomical limits, particularly the anterior and posterior lamella must be reconstructed as two independent structures. Hence, the different techniques already pertaining to both lamellas should be studied, and there must be a safety recommendation regarding using both lamellas to optimize aesthetic results while preserving their functionalities2.
Among the options for the reconstruction of defects with an extension greater than 60% of the anterior lamella is the Mustardé3 rotation flap, which requires a wide area of detachment or local periorbital flaps; some well-known flaps are due to Blasius, Imre, Fricke, and Tripier4. The Tripier flap, originally described in 1889, describes two types of bipediculated myocutaneous flaps based on the orbicularis oculi muscle drawn in the shape of a bucket handle, considered in the literature as the first description of a myocutaneous flap preserving its innervation. One of the flaps described was applied to the lower eyelid reconstruction after resection of a tumor5.
The Tripier flap has been used in a very versatile way and different variations of the technique have been published for both upper eyelid reconstruction and lower eyelid ectropion correction6.
Siegel, in 19877, who called his description “Blepharoplasty flap”, describes the aesthetic and functional advantages of this flap for lower eyelid reconstruction, because he reports that it allows a transfer of muscle tissue that provides adequate support vectors to the eyelid edge, with an optimal compatibility in texture and color of the donor area that leaves the scar on the eyelid fold.
Other modifications have been reported, such as performing a monopediculated lateral flap transposition to correct lateral eyelid defects and also avoiding a second surgical time to section the pedicles8.
Thus, the Tripier myocutaneous flap has advantages such as contribution of muscle tissue to the defect, similarity in color and skin thickness to the recipient area, minimal morbidity of the donor area with minute apparent scar, adequate aesthetic and functional result in the recipient area, less surgical detachment, and a single surgical time.
Posterior lamella reconstruction requires a fibrous tissue support that maintains the eyelid edge at a sufficient height to avoid sclera exposure. Hence, different reconstruction techniques have been proposed using chondromucous grafts of hard palate9,10 and nasal septum11,12, as well as simple conchal or scaphoid auricular cartilage grafts,13 which are well tolerated when used in along with myocutaneous flaps such as the Tripier flap. This offers a benefit in terms of limited movement of the lower eyelid against the corneal surface14 with ease of surgical access.
In this case report, we demonstrate the use of two techniques by a simple execution in a single surgical time: the posterior lamella requires a structure that offers adequate support to the eyelid edge, obtaining a complete occlusion of the eyeball; the cartilage graft from the scapha is sufficiently rigid and still offers a convexity similar to the normal anatomy of the lower eyelid edge, adequately recreating the tarsal plate structure. The difference in the conchal cartilage is that it has a more pronounced curvature; moreover, the perichondrium preservation in the graft allows for conjunctiva mucous reintegration, thereby avoiding direct contact of the cartilage with the sclera. In our case, we use the remaining local conjunctiva to advance cartilage by covering the sclera to position the cartilage graft.
The association of this posterior lamella reconstruction technique with the Tripier flap, which offers well-known advantages, produced a favorable aesthetic result, similar color and texture with adequate functionality, correct positioning of the eyelid edge, and complete sclera occlusion.
CONCLUSION
The monopediculated Tripier myocutaneous flap and scaphoid cartilage graft are two technical resources that, used together, offer a practical approach in planning the reconstruction of defects of total thickness and length greater than 60% of the lower eyelid, thereby offering satisfactory aesthetic and functional results.
COLLABORATIONS
|
CGM |
Analysis and/or data interpretation, Data Curation, Final manuscript approval, Methodology, Writing - Original Draft Preparation, Writing - Review & Editing |
|
MC |
Conception and design study, Final manuscript approval, Methodology, Project Administration, Realization of operations and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing |
|
ACC |
Conception and design study, Data Curation, Writing - Review & Editing |
|
AOE |
Conception and design study, Final manuscript approval, Methodology, Writing - Original Draft Preparation |
|
LG |
Conception and design study, Writing - Original Draft Preparation, Writing - Review & Editing |
|
OS |
Project Administration, Supervision, Validation |
|
ERB |
Conception and design study, Final manuscript approval, Realization of operations and/or trials, Supervision, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
REFERENCES
1. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Estimativa 2018: incidência de câncer no Brasil. Rio de Janeiro (RJ): INCA; 2018. Disponível em: http://www1.inca.gov.br/estimativa/2018/
2. Chang EI, Esmaeli B, Butler CE. Eyelid reconstruction. Plast Reconstr Surg. 2017;140(5):724e-35e.
3. Mustardé JC. New horizons in eyelid reconstruction. Int Ophthalmol Clin. 1989;29(4):237-46.
4. Alghoul M, Pacella SJ, McClellan WT, Codner MA. Eyelid reconstruction. Plast Reconstr Surg. 2013;132(2):288e-302e.
5. Tripier L. Lambeau musculo-cutané en forme de pont. Appliqué à la restauration des paupières. Gazette Hôspitaux Paris. 1889;62:1124-5.
6. Elliot D, Britto JA. Tripier’s innervated myocutaneous flap 1889. Br J Plast Surg. 2004;57:543-9.
7. Siegel RJ. Severe ectropion: repair with modified Tripier flap. Plast Reconstr Surg. 1987;80(1):21-8.
8. Machado WLG, Sampaio FMS, Gurfinkel PCM, Melo MLC, Gualberto GV, Treu CM. Modified Tripier flap in reconstruction of the lower eyelid. An Bras Dermatol. 2015;90(1):108-10.
9. Nakajima T, Yoshimura Y. One-stage reconstruction of full-thickness lower eyelid defects using a subcutaneous pedicle flap lined by a palatal mucosal graft. Br J Plast Surg. 1996;49(3):183-6.
10. Siegel RJ. Palatal grafts for eyelid reconstruction. Plast Reconstr Surg. 1985;76(3):411-4.
11. Santos G, Goulão J. One-stage reconstruction of full-thickness lower eyelid using a Tripier flap lining by a septal mucochondral graft. J Dermatol Treat. 2014;25(5):446-7.
12. Maghsodnia G, Ebrahimi A, Arshadi A. Using bipedicled myocutaneous Tripier flap to correct ectropion after excision of lower eyelid basal cell carcinoma. J Craniofac Surg. 2011;22(2):606-8.
13. Koshima I, Urushibara K, Okuyama H, Moriguchi T. Ear helix flap for reconstruction of total loss of the upper eyelid. Br J Plast Surg. 1999;52:314-6.
14. Codner MA, McCord CD, Mejia JD, Lalonde D. Upper and lower eyelid reconstruction. Plast Reconstr Surg. 2010;126(5):231e-45e.
1. Serviço de Cirurgia Plástica Osvaldo Saldanha, Universidade Metropolitana de Santos,
Santos, SP, Brazil.
2. Hospital A.C. Camargo Cancer Center, São Paulo, SP, Brazil.
Corresponding author: Carlos Goyeneche Montoya Avenida Ana Costa, 146, Cond. 1201, Gonzaga, Santos, SP, Brazil. Zip Code: 11060-002. E-mail: carlosgoye.m@gmail.com
Article received: November 5, 2018.
Article accepted: June 22, 2019.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter