

Original Article - Year 2020 - Volume 35 -
Other trends in abdominoplasty: new design and importance of lipo-mid-abdominoplasty in body contour surgery
Outras tendências na abdominoplastia: novo desenho e importância da lipomidiabdominoplastia na cirurgia do contorno corporal
ABSTRACT
Introduction: During the last few years, the surgical principles of abdominoplasty have remained unchanged. Therefore, many patients undergoing this technique have misalignment and high and straight transverse scars of the abdomen, with the final position of the umbilical scar being very close to the transverse scar, making the abdomen seem short. We propose modifying the basic concept of marking in abdominoplasty, because we believe it is important to position the transverse scar lower in the medial and pubic region and higher at the lateral ends, allowing anterior lumbar flap rotation in an inferomedial direction.
Methods: We retrospectively analyzed 146 patients with abdominal defects and subjected them to lipomid-abdominoplasty, marking with strong upper concavity and guiding the sides of the scar towards the lower transverse line of the abdomen, 4 cm equidistant from the root of the thigh. We also define liposuction as a complementary treatment to body contouring.
Results: We consider that mid-abdominoplasty parameters are applicable in most cases, obtaining satisfactory results both in patients with flatness and supraumbilical abdominal lipodystrophy and patients with an "apron" abdomen with considerable flaccidity and diastasis of the abdominal rectus.
Conclusion: It is important to determine the area of the abdominal defect and its classification to establish treatment strategies and association with complementary procedures. A lower marking with respect to the treatment areas will allow a more aesthetic scar and a harmonic body contour as well as an adequate placement of the umbilical scar, pubis, and lateral ends of the transverse abdominal scar.
Keywords: Abdominoplasty; Body contour; Lipectomy; Abdominal fat; Body surface; Abdominal rectus; Abdominal wall; Umbilicus; Fat tissue.
RESUMO
Introdução: Durante os últimos anos, os princípios cirúrgicos da abdominoplastia permaneceram inalterados. Portanto, muitos resultados observados apresentam desalinhamento, cicatrizes transversais altas e retas do abdome, levando ao posicionamento final da cicatriz umbilical a ser muito próximo da cicatriz transversal, o que dá a impressão de abdome curto. Propomos que a abdominoplastia modifique a concepção básica de sua marcação, pois acreditamos que é importante posicionar a cicatriz transversal mais baixa na região medial e púbica, e mais alta nas extremidades laterais, permitindo, no nível dos flancos, a rotação dos retalhos lombares no sentido anterior em direção inferomedial.
Métodos: Foram analisados de forma retrospectiva 146 pacientes portadores de deformidades abdominais e os submetemos a lipomidiabdominoplastia, marcando com forte concavidade superior e orientando os lados da cicatriz em direção à linha transversa inferior do abdômen, 4cm equidistantes da raiz da coxa. Também associamos a lipoaspiração como um tratamento complementar ao contorno corporal.
Resultados: Consideramos que os parâmetros da midiabdominoplastia são aplicáveis na maioria dos casos, obtendo resultados igualmente satisfatórios, tanto nos pacientes com flacidez e lipodistrofia abdominal supraumbilical, quanto nos pacientes com abdome em avental com importante flacidez e diástase dos retos abdominais.
Conclusão: É importante determinar a área da deformidade abdominal e sua classificação, para estabelecer as estratégias do tratamento e associação de procedimentos complementares. Uma marcação mais baixa, respeitando as áreas de tratamento, permitirá uma melhor cicatriz estética e um contorno corporal harmônico, além de uma adequada colocação dos elementos: cicatriz umbilical, púbis e extremidades laterais da cicatriz abdominal transversa.
Palavras-chave: Abdominoplastia; Contorno corporal; Lipectomia; Gordura abdominal; Superfície corporal; Reto do abdome; Parede abdominal; Umbigo; Tecido adiposo
INTRODUCTION
Because aesthetic abdominal surgery requires a global approach to body contouring, it is necessary to evaluate the surrounding regions and structures1,2. For instance, obesity, significant weight loss, and consecutive pregnancies cause abdominal defects that affect more than one region of the body3,4. It is also important to determine the presence of predisposing factors such as skin flaccidity, localized or generalized lipodystrophy, musculoaponeurotic flaccidity, and stretch marks, which together with the determination of the affected areas, help in choosing suitable surgical strategies1,2,5,6.
Abdominal plastic surgery is a procedure characterized by total resection of skin and fat within the infraumbilical region and is performed without considering the final tissue repositioning. This fact leads to a high horizontal scar near the neo-umbilicus, which makes the abdomen seem short or amputated7. Abdominoplasty includes the following elements: low transverse incision in the abdomen, medial dissection to the costal margin, treatment of diastasis of the rectus abdominis muscle with the plication procedure, abundant resection of the abdominal flap with maximum umbilical transposition of the medial resection, and closure of the skin with trunk flexion3-5.
For this reason, we observed unsatisfactory aesthetic results, generating stigmas such as high and straight scars. Because most surgeons perform an elliptical resection with greater width in the medial axis, the umbilical final position is very close to the transverse lower scar, which makes the abdomen seem short, amputated, and unaesthetic2,7,8. Other observed stigmas are residual flaccidity of the flanks, depression of the suprapubic scar with soft tissue protuberances above and below the incision scar, superior displacement of the suprapubic region with excessive exposure, enlargement of the pubic hair area, and persistence of pubic lipodystrophy9-11 (Figure 1).

We should first refer to the terminology and conceptualization of procedures involved in abdominal plastic surgery, such as complete abdominoplasty, miniabdominoplasty, and mid-abdominoplasty. The first refers to the resection of the infra and/or periumbilical segment and is often indicated for patients with severe supra and infraumbilical abdominal flaccidity3-5. Miniabdominoplasty refers to the discrete abdominal resection of the infraumbilical, suprapubic segment, in patients with mild to moderate infraumbilical skin flaccidity, without supraumbilical flaccidity; whose resection does not cause a decrease in the umbilicopubic distance6. In general, it is indicated for patients with high or upper umbilicus.
The so-called mid-abdominoplasty is the indicated procedure for correcting supra- and juxtaumbilical skin flaccidity, whose detachment and medial traction of the abdominal flap results in lower repositioning of the periumbilical skin with reopening of the umbilicus at a higher skin level. The resulting scar is usually lower and reduced compared with that of full abdominoplasty7,8.
We propose a new approach to the abdomen, regardless of the amount of skin to be resected. In this new approach, the final position of the scar must be low. For this, the resected segment must have a lower height in the medial area, requiring a partial resection of the infraumbilical segment12.
The mid-abdominoplasty known as limited abdominoplasty was proposed and published for the first time in the study by Wilkinson and Swartz13 in 1986. This technique corrected the flaccidity of the skin with a shorter incision, which must be placed on the root of the thigh. Subsequently, Ribeiro et al.8 used this term in 1998 to describe a technique with reduced skin resection compared with standard abdominoplasty. However, the final scars remained straight because of the cuneiform resection of the skin.
The extent of skin resection is defined by the degree of flaccidity or lipodystrophy present in the supra- and infraumbilical segment1,2, which indicates the appropriate treatment. Thus, we believe that many of the standardized techniques in abdominoplasty suggest a larger resection of the medial skin, regardless of the resulting lifting of the pubic area and the high position of the final transverse scar. The extension of the abdominal flap and the area of greater flaccidity occur laterally and not centrally, as in the usual standard abdominoplasty designs14,15.
We also believe that abdominoplasty and liposuction must always be performed together and in a balanced and harmonic way to promote better results and safety, even if the approach to the body contour is performed during various surgeries15,16.
In general, discrete or moderate infraumbilical lipodystrophy responds very well to liposuction, invariably accompanied by adequate and effective skin contraction, with a visible improvement in its elastic and structural properties. Conversely, supraumbilical skin and adipose components indicate the insufficiency of contraction after liposuction. This contractile inability or reduced elastic response to local liposuction imposes or requires the adoption of skin resection and traction methods for better adaptation10,11.
OBJECTIVE
Our objective was to describe a new approach to abdominoplasty regardless of the amount of skin to be resected. A low and concave final position of the scar must be prioritized in abdominoplasty, maintaining the aesthetic integrity of the abdominal wall as a whole and preserving umbilical height12.
METHODS
We retrospectively analyzed 146 patients, of which 143 were female and 3 were male, between January 1988 and March 2019. The senior author performed their surgeries at the Plastic Hospital, Rio de Janeiro, Brazil. All patients were instructed and received sufficient clarification of all the benefits and risks of the procedures performed and considered and accepted all information relevant to the study. Thus, they agreed with the informed consent form provided to them. This study was conducted in accord with the Declaration of Helsinki, always promoting and safeguarding the health of patients, and was approved by the Ethics Committee of the Plastic Hospital (approval 09/2018).
The patients’ age range was 30-50 years, with a predominance of patients aged between 41 and 50 years (40% of the surgeries).
In the diagnostic evaluation of the cases, we observed each of the three most important elements in the direct or indirect determination of the abdominal form separately, as well as the body contour. These elements are skin, subcutaneous panniculus, and the musculoaponeurotic complex1,2,6,17,18. For this purpose, pre- and postoperative evaluations were performed according to the classification of abdominal defects proposed by Caldeira et al.1,2 in 1990 (Chart 1).
| Category | Skin flaccidity | Lipodystrophy | Musculoaponeurotic flaccidity | Treatment |
|---|---|---|---|---|
| Group I | None | Mild to moderate | None | Liposuction |
| Group II | Mild to moderate in the infraumbilical region |
Moderate | With or without | Mini-abdominoplasty with liposuction |
| Group III | Mild to moderate in the infra- and supraumbilical region |
Moderate | Moderate | Mid-abdominoplasty with liposuction |
| Group IV | Marked | Moderate or marked |
Moderate or marked | Lipoabdominoplasty |
| Group V | Presence of medium vertical scar with moderate or marked skin flaccidity |
Moderate or marked |
Marked | Vertical abdominoplasty |
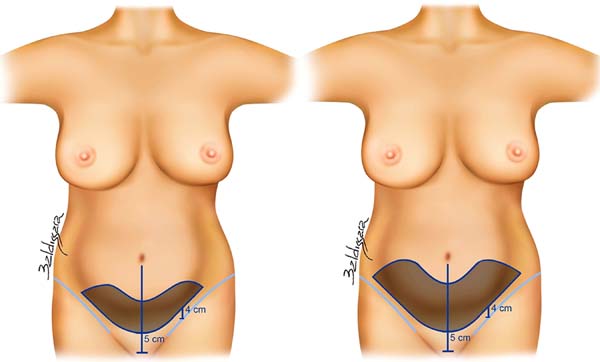
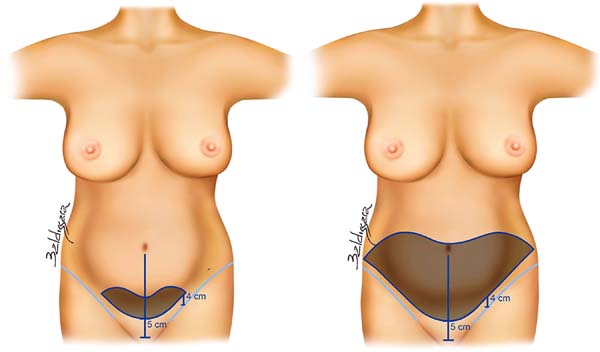
We began marking for the mid-abdominoplasty and liposuction with the patient in the supine position. We identified the pubic symphysis and drew a vertical line toward the umbilicus at a height of 5 cm from the medial commissure. We then marked a transverse curved line of upper concavity extending laterally toward the lower transverse fold of the abdomen. We set the position of the root of the thigh to ensure that the drawn line remained 4 cm above it in order to preserve the integrity of the inguinal region (Figure 2A and 2B) Thus, we preserved the strong adhesion zones described by Lockwood19 in 2006 (Figure 3A and 3B).

For marking the upper limit of the skin resection, we defined the medial height of the flap by bidigital palpation, extending laterally in an upper convexity design, resulting in a larger resection of the tissue in the lateral areas of the abdomen. This marking is also applicable for cases with less skin resection, such as in a mini-abdominoplasty. The marking denotes the areas of strong adhesion, and a smaller design is carried out proportional to the amount of tissue to be resected (Figure 4A). In cases with greater tissue resection, the lateral curved lines rise slightly higher, allowing more volume to be included. Thus, the shape of the drawing is maintained, and resection can reach the umbilicus (Figure 4B). In other words, full abdominoplasty is performed only when the resection of the lateral segments is higher than the umbilicus. We treat lipodystrophy with liposuction of the flanks and upper abdomen before dermolipectomy for providing a better outline of the silhouette. We continue with the plication of the abdominal rectus muscle with continuous suture using Prolene 0 in one or two planes. The umbilicus is then fixed to the aponeurosis as proposed by the technique of Avelar20 in 2016. This position is set at 14-16 cm from the transverse scar12. The flap is then fixed to the aponeurosis with the points proposed by Pollock21 in 2004 and by Baroudi22 in 1998. It is then closed in three anatomical planes.
Antibiotic prophylaxis is performed with 2 g of cefazolin at the beginning of the surgical procedure, following the standard scheme with continued outpatient use. We performed abdominal drainage of the flanks and lumbar region exteriorized by pubic contraincision, which was maintained for 5 to 7 days. The dressing consists of padded gauze wrapped by elastic bandages for 12 to 24 hours. A mild to moderate compression girdle is used on the first day of the postoperative period and maintained for 30 days together with an anterior abdominal rigid plate. Calf wraps are also used from the preoperative period (maintained for 7 days), and the patient starts receiving massages by a trained professional from the second week after surgery.
RESULTS
We treated 146 patients with a mean BMI of 28.1 kg/m2 and predominantly aged between 41 and 50 years (40%). Most patients (143, 97.94%) were female, and three (2.05%) were male (Table 1).
| n | % | |
|---|---|---|
| Mean Age | ||
| 41 - 50 years | 58 | 39.72 |
| Sex | ||
| Female | 143 | 97.95 |
| Male | 3 | 2.05 |
| Mean Bmi | 28.1 | - |
| Patient Post-bariatric surgery | 25 | 17.2 |
| Procedure | ||
| Abdominoplasty | 15 | 10.27 |
| Mid-abdominoplasty | 130 | 89.04 |
| Mini-abdominoplasty | 1 | 0.68 |
| Complications | 12 | 8.21 |
| Total | 146 | 100 |
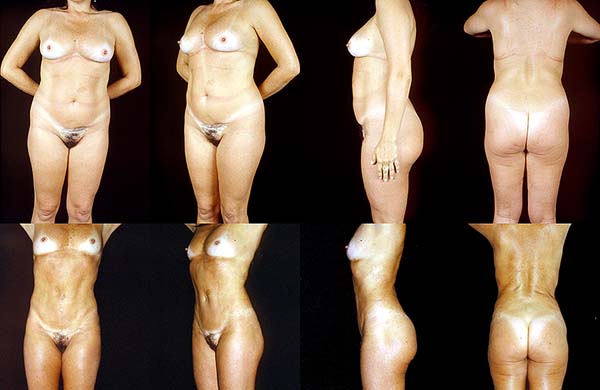
Mid-abdominoplasty was performed in 130 patients (89.04%). We initially performed mid-abdominoplasty for patients with flaccidity and significant lipodystrophy of the supraumbilical abdomen, obtaining good results (Figures 5 and 6). Subsequently, we extended the indication to cases of “pendulum” or “apron” abdomen with flaccidity and diastasis of the abdominal rectus muscle, as a result of the loss of body contour, also obtaining satisfactory results (Figures 7, 8, and 9). Therefore, we considered that the parameters of mid-abdominoplasty are applicable in most cases (Figure 10).





We also observed that the number of complications was low and within the expected value for an abdominoplasty procedure. Small seromas were observed in 5.47% of patients and were drained by a puncture in two to three sessions. Dehiscence was observed in two cases (1.36%), one of 1 cm and the other of 3 cm, and were addressed by resuturing. Two cases of necrosis (1.36%) were observed, one of 2 × 1.5 cm and the other of 2.5 × 2 cm, and were addressed with serial dressings (Table 2).
| Complications | No. of patients | Percent |
|---|---|---|
| Seroma | 8 | 5.47 |
| Necrosis | 2 | 1.36 |
| Dehiscence | 2 | 1.36 |
| Hypertrophic scar | 0 | 0.00 |
| No complications | 134 | 91.78 |
| Total number of complications | 12 | 8.21 |
DISCUSSION
Since the beginning of modern abdominoplasty in 1960, modifications have been proposed by several authors7,8,13,15,23,24. However, the surgical stigmas of these approaches, such as high and straight scars, remained constant. Therefore, changing the view on abdominoplasties is necessary. We consider that the final position of the scar must be prioritized rather than focusing on the amount of skin to be removed. Therefore, we try to set the final scar at a low level to protect the aesthetics of the abdomen12 (Figure 11).

In order to keep the scar in this position and have a medial concavity, the infraumbilical region cannot be completely resected. In standard resection, the medial limitation of the tissue reduces the distance between the umbilicus and the final scar, which generates an upper straight scar.
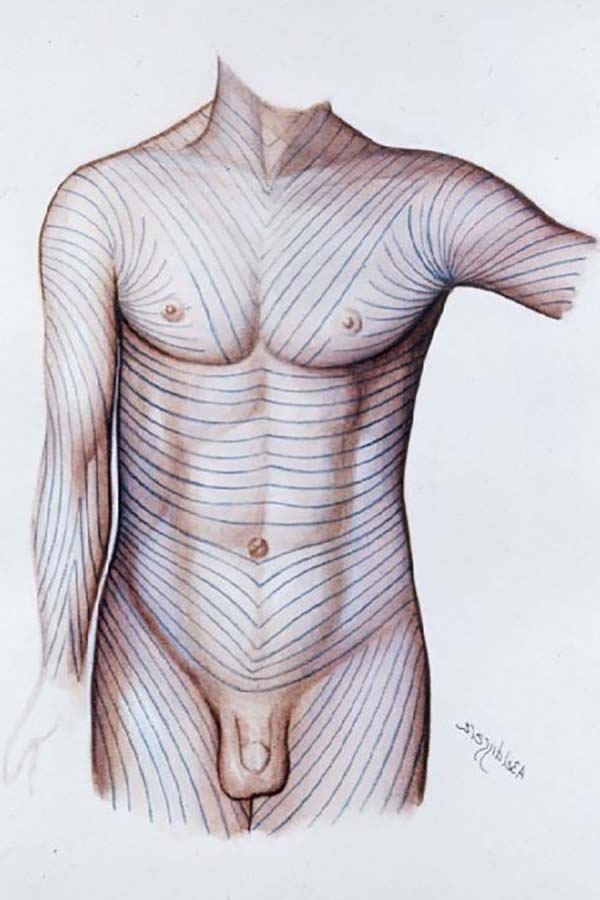
We also propose that the lateral ends of the marking be high, thus allowing anterior rotation of the lumbar flaps in the inferomedial direction. The aim is to achieve a transverse scar with a robust medial concavity with the ends maintaining the lateral limits accompanying the lower transverse fold of the abdomen. This location allows us to position the scar in an anatomical position parallel to the Langer lines, reducing tension and favoring wound healing (Figure 12).

Moreover, weight in the abdominal region starts accumulating on the flanks extending secondarily to the hypogastrium. For this reason, abdominoplasty naturally requires a more significant resection of the lateral segments15,16. The result is an anatomically positioned final scar, providing the abdomen with a long, well-defined form (Figure 13).
Partial or subtotal resection of the medial infraumbilical segment was first indicated to treat only cases with a small amount of central flaccidity of the supraumbilical skin of the abdomen. Subsequently, we realized that our approach encompassed a critical aspect, which is that primary mid-abdominoplasty can be indicated even for patients with great weight loss and great abdominal flaccidity.
We also consider that the evaluation of the abdomen must differentiate the contractility response of the skin to the liposuction of the supraumbilical and infraumbilical regions as the quality and their behavior differ.
We evaluated in these regions whether there is a predominance of lipodystrophy over skin flaccidity. In cases of marked infraumbilical lipodystrophy, liposuction is indicated, because there is a good response, generating infraumbilical contraction of the skin. Conversely, in cases of supraumbilical lipodystrophy, where the response to skin contractility is reduced, we cannot recommend performing only liposuction, because the skin of this region can become flaccid. We use a classification of abdominal defects and their treatment as an attempt to standardize these treatments according to the degree of defect, the elements of the defect, and the possible strategies1,2 (Table 1). Another point to be taken into account is the umbilicus, which contributes significantly to the abdominal aesthetics and the perception of a long abdomen7,25-27.
The appearance of the three-dimensional umbilicus is influenced by the height, width, and shape of the abdominal incision; the length of the umbilical pedicle; the diameter of the disc; the umbilical shape; and the distribution of periumbilical fat. The umbilicus can have various forms: wide, narrow, superficial, herniated, virgin, already operated, and absent28. Treatment will depend on the form and the technique chosen for this purpose.
Currently, there are many proposals for positioning the umbilicus, and all of them are valid provided there is harmony. Harmony is achieved by considering the height of the umbilicus in relation to the transverse scar of the abdominoplasty. For this reason, we try to set the umbilicus at a mean height of 14 to 16 cm, provided that the original position allows it, and according to the patient’s biotype25,26,28. The umbilicus is fixed on the aponeurosis 1 to 2 cm above its original position, with sutures on the cardinal points to decrease skin tension in the epigastrium12,29.
It is important to remember that the location changes according to sex because the male umbilicus is usually lower in the abdominal wall than the female one.
For optimal repositioning of the umbilicus, we must consider the perfusion to minimize the risk of postoperative necrosis and visible scars25. With regard to vascularization of the abdominal dermofat flap, of the Huger zones, only zone III of the lateral perforators is preserved. A study by Munhoz et al.30 in 2006 found that 80% of perforators, lymphatic vessels, and nerves could be preserved with limited dissection. Perforations of the deep upper epigastric artery are more predictable.
The association of liposuction with mid-abdominoplasty allows us to reduce the size of the scar and restructure and redefine the silhouette line and body contour12. Moreover, liposuction of the flanks moves the lateral flap toward the anterior and medial direction, causing greater lateral rotation and lift of its ends.
Liposuction and fat grafting complement the range of procedures. We used liposuction to accentuate the Alba and Spiegel31 lines. We take special care to perform the incision just above the new position of the umbilicus toward the xiphoid appendix, preserving the lower portion. High-definition liposuction is associated with abdominoplasty in specific cases, for which we think the result will be improved and will not affect the viability of the abdominal flap31.
CONCLUSION
It is necessary to improve the position of the transverse scar and adequately position the elements umbilicus, pubis, and lateral ends of the transverse abdominal scar to obtain a more harmonious result. Adequate analysis and classification of abdominal defects are necessary to establish appropriate strategies for the treatment of each case.
COLLABORATIONS
|
AMLC |
Analysis and/or data interpretation, Conception and design study, Conceptualization, Final manuscript approval, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
CD |
Analysis and/or data interpretation, Data Curation, Investigation, Visualization, Writing - Original Draft Preparation |
|
JCH |
Analysis and/or data interpretation, Data Curation, Investigation, Visualization, Writing - Review & Editing |
REFERENCES
1. Caldeira AML, Niéves AP, Oliveira AL. Cirurgia do contorno corporal – Reflexões sobre um novo enfoque da cirurgia plástica do abdome – I Parte – Classificações das deformidades abdominais e suas correlações cirúrgicas. Rev Bras Cir Plást. 1990;80(2):95-104.
2. Caldeira AML, Nieves PA, Oliveira AL. Cirurgia do contorno corporal – Reflexões sobre um novo enfoque da cirurgia plástica do abdome – II Parte. Rev Bras Cir Plást. 1990;80(3):169-86.
3. Pitanguy I. Abdominal lipectomy: an approach to it through an analysis of 300 consecutive cases. Plast Reconstr Surg. 1967;40(4):384-91.
4. Callia W. Contribuição para o estudo da correção cirúrgica do abdome penduloso e globoso. Técnica original [tese]. São Paulo (SP): Faculdade de Medicina da Universidade de São Paulo; 1965.
5. Baroudi R, Ferreira CA. Contouring the hip and the abdomen. Clin Plast Surg. 1996 Oct;23(4):551-72;discussion:572-3.
6. Elbaz JS, Flageul G. Liposuccion et chirurgie plastique de l’abdomem. Paris: Masson; 1988. DOI: https://doi.org/10.1007/978-3-319-27851-3_30
7. Dardour JC, Vilain R. Alternatives to the classic abdominoplasty. Ann Plast Surg. 1986 Sep;17(3):247-58.
8. Ribeiro L, Accorsi AJ, Buss A. Midiabdominoplasty: indications and technique. Aesthetic Plast Surg. 1998;22(5):313-7. DOI: https://doi.org/10.1007/s002669900209
9. Caldeira AML, Carrión K, Jaulis J. Repair of the severe muscle aponeurotic abdominal laxity with alloplastic mesh in aesthetic abdominoplasty. Aesthetic Plast Surg. 2018;42(4):1039-49. DOI: https://doi.org/10.1007/s00266-018-1101-6
10. Caldeira AML, Robles MBM. Challenges in abdominoplasty. In: Avelar J, ed. New concepts on abdominoplasty and further applications. Switzerland: Springer International Publishing; 2016. p. 481-95. DOI: https://doi.org/10.1007/978-3-319-27851-3_30
11. Caldeira AML, Carrión K, Jaulis J. Conceptos prácticos para el tratamiento de las deformidades abdominales complejas. Cir Plást Iberolatinoam. 2018;44(3):269-79. DOI: https://doi.org/10.4321/S0376-78922018000300005
12. Caldeira AML, Carrión K, Jaulis J. Focus on the importance of the lipomid-abdominoplasty in the body contouring surgery. Aesthetic Plast Surg. 2019;43:718-25. DOI: http://doi.org/10.1007/s00266-019-01367-9
13. Wilkinson TS, Swartz BE. Individual modifications in body contour surgery: the “limited” abdominoplasty. Plast Reconstr Surg. 1986 May;77(5):779-84.
14. Hughes CE III, Baroudi R, Lockwood TE, Matarasso A. Abdominoplasty. Aesth Surg J. 2002;22(5):465-73. DOI: http://doi.org/10.1067/maj.2002.129158
15. Lockwood T. High-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995 Sep;96(3):603-15.
16. Lockwood T. Maximizing aesthetics in lateral-tension abdominoplasty and body lifts. Clin Plastic Surg. 2004 Oct;31(4):523-37. DOI: https://doi.org/10.1016/j.cps.2004.04.001
17. Matarasso A. Abdominoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy”. Aesthetic Plast Surg. 1991;15(2):111-21.
18. Bozola AR. Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plast Surg. 2010;34(2):181-92. DOI: https://doi.org/10.1007/s00266-009-9407-z
19. Lockwood T. Lower body lift and medial thigh lift. In: Aly A, ed. Body contouring after massive weight loss. Saint Louis, MO: Quality Medical Publishing; 2006. p. 147-81.
20. Avelar J. Creation of the new umbilicus: my technique on abdominoplasty and further applications. In: Avelar J, ed. New concepts on abdominoplasty and further applications. Switzerland: Springer International Publishing. 2016; p. 107-26.
21. Pollock T, Pollock H. Progressive tension sutures in abdominoplasty. Clin Plast Surg. 2004 Oct;31(4):583-9. DOI: https://doi.org/10.1016/j.cps.2004.03.015
22. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesth Surg J. 1998 Nov/Dec;18(6):439-41.
23. Pontes R. Variantes das abdominoplastias em bloco. In: Pontes R, ed. Abdominoplastia. Rio de Janeiro (RJ): Revinter; 2004. p. 25-54.
24. Saldanha OR, Federico R, Daher PF, Malheiros AA, Carneiro PR. Lipoabdominoplasty. Plast Reconstr Surg. 2009 Sep;124(3):934-42. DOI: https://doi.org/10.1097/PRS.0b013e3181b037e3
25. Silva Júnior V, Sousa FRS. Improvement on the neo-umbilicoplasty technique and review of the literature. Aesthetic Plast Surg. 2017;41(3):600-7. DOI: https://doi.org/10.1007/s00266-017-0847-6
26. Fantozzi F. Applications of anthropometry in torsoplastic surgery. Eur J Plast Surg. 2013;36:519-26. DOI: https://doi.org/10.1007/s00238-013-0854-z
27. Villegas FJ. A novel approach to abdominoplasty: TULUA modifications (transverse plication, no undermining, full liposuction, neoumbilicoplasty, and low transverse abdominal scar). Aesthetic Plast Surg. 2014;38(3):511-20. DOI: https://doi.org/10.1007/s00266-014-0304-8
28. Shiffman MA. Adult umbilical reconstruction – Principles and Techniques. Switzerland: Springer International Publishing; 2017.
29. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plastic and Reconstructive Surgery. 2001 Nov;108(6):1787-95.
30. Munhoz AM, Kamamoto F, Saito FL, Menezes M, Gemperli R. Anatomical mapping of the perforant abdominal vessels and clinical application in the treatment of aesthetic deformities of the abdominal wall through lipoabdominoplasty. In: Saldanha O, ed. Lipoabdominoplasty. Rio de Janeiro: Di-Livros; 2006. p. 103-13.
31. Danilla S. Rectus Abdominis Fat Transfer (RAFT) in lipoabdominoplasty: a new technique to achieve fitness body contour in patients that require tummy tuck. Aesthetic Plast Surg. 2017;41(6):1389-99. DOI: https://doi.org/10.1007/s00266-017-0909-9
1. Hospital Evangélico, Instituto Avançado de Cirurgia Plástica, Rio de Janeiro, RJ,
Brazil.
2. Hospital Casa de Portugal, Universidade Santa Úrsula, Rio de Janeiro, RJ, Brazil.
Corresponding author: Alberto Magno Lott Caldeira Rua Visconde de Pirajá, 414, Ipanema, Rio de Janeiro, RJ, Brazil. Zip Code: 22410-002. E-mail: lottcaldeira@gmail.com
Article received: May 9, 2019.
Article accepted: February 22, 2020.
Conflicts of interest: none.



















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter