

Original Article - Year 2020 - Volume 35 -
Mandibular reconstruction with fibula free flap: case series
Reconstrução de mandíbula com retalho livre de fíbula: série de casos
ABSTRACT
Introduction: Mandibular reconstruction is a complex procedure aimed at correcting defects of the lower third of the face and achieving functional rehabilitation, including chewing and oral competence. Fibula free flap is the first choice for the reconstruction of segment defects of the adjacent mandible and soft tissue.
Methods: A retrospective clinical study was conducted from January 2005 to July 2017, analyzing the medical records of patients undergoing microsurgical reconstructions after resection of head and neck neoplasms at the plastic surgery service of the Clinical Hospital of the Federal University of Pernambuco (HC-UFPE).
Results: This study included six patients, of which three were men (50%), aged between 12 and 48 years and with a mean age of 24 years. In 83% of the cases, reconstructions were performed with osteomyocutaneous fibula free flaps (in one case, there was no need for skin island flap). We observed an adequate coverage of the large defects analyzed, with good functional and aesthetic appearance in all cases. Immediate reconstruction was performed in 83% of cases. The fibula and receptive area were prototyped in two cases.
Conclusion: Fibula free flaps are a great alternative for head and neck reconstruction. Our initial experience and literature show satisfactory results, partially restoring the shape and function of the affected areas.
Keywords: Microsurgery; Mandible; Surgical flaps; Printing, Three-Dimensional; Fibula; Reconstructive surgical procedures.
RESUMO
Introdução: A reconstrução da mandíbula é um procedimento complexo, que visa a correção das deformidades do terço inferior da face e reabilitação funcional, incluindo mastigação e competência oral. O retalho livre de fíbula é a primeira escolha para a reconstrução de falhas segmentares da mandíbula e tecido mole adjacentes.
Métodos: Foi realizado um estudo clínico retrospectivo, no período de janeiro de 2005 a julho de 2017, analisando os prontuários dos pacientes submetidos a reconstruções microcirúrgicas após a ressecção de neoplasias em cabeça e pescoço, operados pelo serviço de cirurgia plástica do Hospital das Clínicas da Universidade Federal de Pernambuco (HC-UFPE).
Resultados: Seis pacientes foram incluídos no estudo, sendo três do sexo masculino (50%), a idade variou de 12 a 48 anos, com média de 24 anos. Em 83% dos casos foram realizadas reconstruções com retalhos livres de fíbula osteomiocutâneos (em um dos casos não houve necessidade de confeccionar ilha de pele junto ao retalho). Observou-se uma cobertura eficaz dos extensos defeitos estudados, apresentando em todos os casos bons resultados quanto ao aspecto funcional e estético. Em 83% dos casos reconstrução imediata foi realizada. A prototipagem da fíbula e da área receptora foi realizada em dois casos.
Conclusão: Retalhos livres de fíbula constituem uma ótima alternativa para reconstrução em cabeça e pescoço. Nossa experiência inicial e a literatura mostram resultados satisfatórios, restaurando parcialmente forma e função das áreas acometidos.
Palavras-chave: Microcirurgia; Mandíbula; Retalhos cirúrgicos; Impressão tridimensional; Fíbula; Procedimentos cirúrgicos
INTRODUCTION
Mandibular reconstruction is a complex procedure and remains a challenge in plastic surgery1. Although attempts of reconstruction have been described since the 19th century, the greatest experience took place during the First and Second World War1,2. Initial reconstruction attempts using bone grafts and pediculated osteocutaneous flaps were characterized by a high incidence of postoperative complications and poor long-term outcomes2.
The advent of microsurgery has modified reconstructive plastic surgery. Microsurgical flaps have many advantages: complex and larges defects can be repaired in a single stage, reducing hospitalization time, hospital expenses, and morbidity, and it allows primary closure of the donor area. There are several indications for mandibular reconstruction, including cancer resections, traumatic injuries, and osteoradionecrosis3.4. The ultimate goal is restoring form and function and improving chewing, swallowing, speech, and oral competence5,6.
Currently, the transfer of vascularized bone through microsurgical technique is the gold standard for mandibular reconstruction7,8,9,10. Fibula free flap was first described by Taylor, 1975 Apud Hidalgo, 2002 introduced it in mandibular reconstruction in 19896. Despite the many advantages of microsurgical reconstructions, mastering this tool requires a long learning curve, and failure can lead to consequences proportional to the magnitude of technique11.
OBJECTIVES
This study aimed at evaluating a series of patients undergoing complex mandibular reconstructions performed by the plastic surgery team of the Clinical Hospital of the Federal University of Pernambuco (HC-UFPE) using fibula free flap after great tumor resections.
METHODS
A retrospective clinical study was conducted from January 2005 to July 2017, analyzing the medical records of patients undergoing microsurgical reconstructions after resection of head and neck neoplasms at the surgical service of the Clinical Hospital of the Federal University of Pernambuco (HC-UFPE).
The inclusion criteria were as follows: medical records of patients treated at the plastic surgery clinic of HC-UFPE with a diagnosis (clinical and histopathological) of mandible neoplasm undergoing resections, followed by reconstruction with fibula free flaps. The following parameters were analyzed: gender, age, etiology, type of reconstruction, and complications. The following patients were excluded from the study: those with incomplete medical records or those who were lost to outpatient follow-up.
Since our study is retrospective using secondary data from medical records, obtaining an Informed Consent Form (ICF) was impossible. The study was approved by the Ethics and Research Committee of the Federal University of Pernambuco (CAAE: 82226718.8.0000.5208).
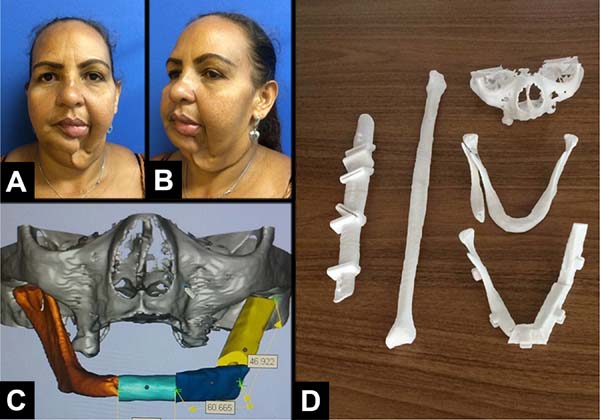
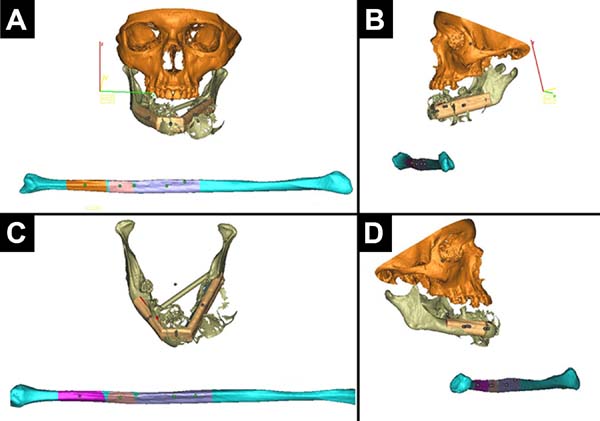
Prototyping was performed in two cases (Figures 2 and 3). The DVD containing the computed tomography of patients was sent to the Renato Archer Information Technology Center (Centro de Tecnologia da Informação Renato Archer) (Figure 1). On the day before surgery, the prototypes were taken to the surgical center, where the procedure was simulated, the margin of proximal resection was decided, the mandibular reconstruction plate was fixed, and the size of the screws for each bone segment was chosen (collected fibula). The number of osteotomies was defined in digital planning. All the fixation material was sterilized after model surgery. Skull base (with the glenoid), the donor fibula, an osteotomy guide for the fibula, and the defective mandible were prototyped (Figure 4).

RESULTS
The cases included six patients, three of whom were male (50%), aged between 12 to 48 years with a mean age of 24 years. All reconstructions were performed after the resection of head and neck neoplasms (Table 1).
| Cases | Gender | Age | Etiology | Type reconstruction | Complications | Prototyping |
|---|---|---|---|---|---|---|
| 1 | Fem | 48 | Malignant fibrohistiocytoma | Delayed | No | Yes |
| 2 | Fem | 40 | Ameloblastoma | Immediate | No | Yes |
| 3 | Male | 18 | Aneurysmal bone cyst | Immediate | No | No |
| 4 | Fem | 12 | Giant Cell Carcinoma | Immediate | No | No |
| 5 | Male | 17 | Sarcomatous Neoplasia | Immediate | Defect at the contour of the mandible |
No |
| 6 | Male | 12 | Aneurysmal bone cyst | Immediate | Osteomyelitis | No |
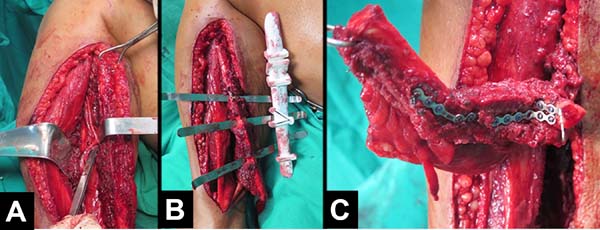
Osteomyocutaneous fibula free flaps for mandibular reconstruction were performed in 5 cases (in one case, there was no need for flap skin island). In all cases, the large defects were adequately covered, with good functional and aesthetic results and minimal morbidity of the donor area.
One case required a second surgical period for a better definition of the new mandible and underwent arthroplasty for the affected hemiface. Another case had osteomyelitis in the 3rd month postoperatively and underwent surgical debridement and received venous antibiotic therapy.
All cases of reconstruction were tracheostomized intraoperatively, with the tube being removed within three weeks. Only one patient underwent delayed reconstruction (Table 1).
The feasibility rate of the flaps performed in our study was 100%.
DISCUSSION
Microsurgical reconstructions are complex techniques needed at advanced reconstruction centers and are crucial in head and neck cancer surgeries. Over the past 50 years, several advances in these techniques and several potential flaps have been described1-5. Three decades have passed since the introduction of the osteomyocutaneous fibula flap in 1986, and this flap remains the gold standard for reconstruction of bone defects in the mandible and extremities6-8.
Mandibular rehabilitation is important because there are several functions performed by this bone, including participation in chewing, swallowing, oral competence, verbalization, and breathing support. Moreover, it significantly contributes to the contours of the middle third of the face10.
In the sample analyzed, six mandibles were reconstructed after resection of tumors in the mandible.
Delayed reconstruction of the mandible was chosen for only one of the patients (Table 1). In this case, there was no history of prior local radiotherapy. In delayed reconstruction, the chances of detecting tumor recurrence and local spread are higher, unlike immediate reconstruction, covering the primary site12,13,14. Most authors prefer immediate reconstruction. It results in better aesthetic results, decreased morbidity, faster rehabilitation of the patient, prevention of sequelae that hinder delayed reconstruction, and reduction of cost and treatment time14. In Brazil, the absence of microsurgeons, limited operating room time, lack of adequate material, and doubt about free margins often lead to delayed microsurgical mandibular reconstructions15.
Craniofacial and donor fibula was prototyped for two patients (Figures 2 and 3). The introduction of prototyping in medicine is relatively recent. With the technological advancement of radiology (tomography and resonance), high-definition images are generated, allowing detailed 3D visualization and analysis of anatomical structures. A digital printer can create a 3D model of the analyzed anatomical structure from these images (Figure 1)16,17. Computed tomography (CT) was used as a standard examination for prototype construction since the literature considered this type of image ideal18.
In cases 1 and 2 (Table 1), model surgery performed the day before provided several benefits: decreased morbidity of the donor area (capturing only what was needed); definition of resection margins (in case 2); plate fixation; choice of screws; maintenance of the mandibular transverse diameter; fitting of the condyle prosthesis to the TMJ; maintenance of the best possible occlusion; shorter surgical time, shorter anesthesia time, and lower hospital cost. An important technical detail of this prototyping is that prototyping skull base (containing the glenoid) and the fibula with the osteotomy sites were required (Figure 4)17,18,19,20.
The fibula is very important for dental rehabilitation in implant dentistry. Osseointegrated implants should be placed between 4 and 6 months, in case of bone grafts, and longer waiting periods may cause bone resorption owing to lack of load. Unfortunately, none of our patients have received osseointegrated implants owing to the unavailability of staff and material provided by the Brazilian Unified Health System (SUS)12,13.
Mandibular reconstruction has greater complications than reconstructions performed in other regions of the face. In a previous study conducted by Portinho et al., in 201311, the incidences of complications in the receiving area, in patients undergoing mandibulectomies, were as follows: fistula, 21.2%; necrosis, 13.5%; dehiscence, 13.5%; infection, 11.5%; bleeding, 9.6%; and extrusion of osteosynthesis material, 1.9%. In our study, we observed only one case that had a local infection (osteomyelitis), requiring hospitalization and use of antibiotics21,22,23.
CONCLUSION
Fibula free flaps are a great alternative for head and neck reconstruction. Our initial experience and literature show satisfactory results, partially restoring the shape and function of affected tissues. The learning curve is long but tends to improve with training of the team.
COLLABORATIONS
|
MFMBL |
Analysis and/or data interpretation, Conception and design study, Data Curation, Final manuscript approval, Methodology, Project Administration, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
JPBRM |
Supervision, Writing - Review & Editing |
|
RA |
Supervision, Writing - Review & Editing |
|
JZS |
Writing - Review & Editing |
|
KK |
Analysis and/or data interpretation, Data Curation |
REFERENCES
1. Erdmann D, Giessler GA, Bergquist GE, Bruno W, Young H, Heitmann C, et al. Free fibula transfer: analysis of 76 consecutive microsurgical procedures and review of the literature. Chirurg. 2004;75(8):799-809.
2. Wallace CG, Chang YM, Tsai CY, Wei FC. Harnessing the potential of the free fibula osteoseptocutaneous flap in mandible reconstruction. Plast Reconstr Surg. 2010;125(1):305-14.
3. Cardoso IF, Sbalchiero JC, Batista AS, Ohoma BMB, Chedid R, Cardoso GF, et al. Uso do retalho osteocutâneo microcirúrgico de fíbula na reconstrução dos defeitos complexos de mandíbula. Res Bras Cir Plást. 2011;26(1):42-7.
4. Chim H, Salgado CJ, Mardini S, Chen HC. Reconstruction of mandibular defects. Semin Plast Surg. 2010;24(2):188-97.
5. Brown JS, Lowe D, Kanatas A, Schache A. Mandibular reconstruction with vascularized bone flaps: a systematic review over 25 years. Br J Oral Maxillo Fac Surg. 2016;55(2):113-26.
6. Hidalgo DA, Pusic AL. Free-flap mandibular reconstruction: a 10-year follow-up study. Plast Reconstr Surg. 2002;110(2):438-49;discussion:450-1.
7. Deek NFA, Kao HK, Wei FC. The fibula osteoseptocutaneous flap: concise review, goal-oriented surgical technique, and tips and tricks. Plast Reconstr Surg. 2018;142(6):913e-23e.
8. Gerressen M, Pastaschek CI, Riediger D, Hilgers RD, Hölzle F, Noroozi N, et al. Microsurgical free flap reconstructions of head and neck region in 406 cases: a 13-year experience. J Oral Maxillofac Surg. 2013;71(3):628-35.
9. Wu CC, Lin PY, Chew KY, Kuo YR. Free tissue transfers in head and neck reconstruction: complications, outcomes and strategies for management of flap failure: analysis of 2019 flaps in single institute. Microsurgery. 2014;34(5):339-44.
10. Hayden RE, Mullin DP, Patel AK. Reconstruction of the segmental mandibular defect: current state of the art. Curr Opin Otolaryngol Head Neck Surg 2012;20(4):231-6.
11. Portinho CP, Sbalchiero JC, Cardoso MM, Jungblut CF, Souza THS, Collares MVM. Reconstrução microcirúrgica em cabeça e pescoço: análise retrospectiva de 60 retalhos livres. Rev Bras Cir Plást. 2013;28(3):434-43.
12. Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84(1):71-9.
13. Hidalgo DA. Aesthetic improvements in free-flap mandible reconstruction. Plast Reconstr Surg. 1991;88:574-85;discussion:586-7.
14. Wei F, Celik N, Yang WG, Chen IH, Chang YM, Chen HC. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast Reconstr Surg. 2003;112(1):37-42.
15. Liu TY, Huang YC, Leong CP, Tseng CY, Kuo YR. Home-based exercise on functional outcome of the donor lower extremity in oral cancer patients after fibula flap harvest. Biomed J. 2013;36(2):90-5.
16. Eckardt A, Swennen GR. Virtual planning of composite mandibular reconstruction with free fibula bone graft. J Craniofac Surg. 2005;16(6):1137-40.
17. Bell RB. Computer planning and intraoperative navigation in craniomaxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2010;22(1):135-56.
18. Bill JS, Reuther JF, Dittman W, et al. Stereolithography in oral and maxillofacial operation planning. Int J Oral Maxillofac Surg. 1995;24(1 Pt 2):98-103.
19. Ueda KM, Tajima SM, Oba SM, Omiya Y, Byun SI, Okada M. Mandibular contour reconstruction with three-dimensional computer-assisted models. Ann Plast Surg. 2001;46(4):387-93.
20. Schusterman MA, Reece GP, Miller MJ, Harris S. The osteocutaneous free fibula flap: is the skin paddle reliable?. Plast Reconstr Surg. 1992;90:787-793;discussion:794-8.
21. Winters HA, Jongh GJ. Reliability of the proximal skin paddle of the osteocutaneous free fibula flap: a prospective clinical study. Plast Reconstr Surg. 1999;103:846-9.
22. Yoshimura M, Shimada T, Hosokawa M. The vasculature of the peroneal tissue transfer. Plast Reconstr Surg. 1990;85:917-21.
23. Yajima H, Ishida H, Tamai S. Proximal lateral leg flap transfer utilizing major nutrient vessels to the soleus muscle. Plast Reconstr Surg. 1994;93:1442-8.
1. Hospital das Clínicas da Universidade Federal de Pernambuco, Recife, PE, Brazil.
Corresponding author: Marcel Fernando Miranda Batista Lima Rua Barão de Itamaracá 78, Apto 1203,Espinheiro, Recife, PE, Brazil. Zip Code: 52020-070. E-mail: marcelflima@hotmail.com
Article received: July 1, 2019.
Article accepted: February 22, 2020.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter