

Original Article - Year 2019 - Volume 34 -
Ronaldo Pontes block abdominoplasty technique
Técnica Ronaldo Pontes de abdominoplastia em bloco
ABSTRACT
Introduction: Abdominoplasty involves not only aesthetic characteristics but abdominal wall structural reconstruction. This study aimed to illustrate the authors' experience with abdominoplasty, focusing on the scar's aesthetic results and the evolution of application of the block resection technique of Professor Ronaldo Pontes (RP).
Methods: The study included a series of retrospective cases of 124 patients treated between March 2014 and March 2017 who underwent RP block abdominoplasty.
Results: In our studies, a minimal incidence of complications and a small number of healing alterations were noted with the RP block technique compared to those found in the literature.
Conclusion: A técnica descrita e suas variantes atendem a necessidade de diversos tipos de casos e garantem cirurgias seguras e eficazes, com resultados muito satisfatórios, sendo uma técnica reprodutível.
Keywords: Abdominoplasty; Seroma; Hematoma; Hypertrophic scar; Keloid.
RESUMO
Introdução: Abdominoplastia é um procedimento não apenas com características estéticas, mas também de reconstrução estrutural da parede abdominal. O objetivo do trabalho é mostrar a experiência dos autores em abdominoplastias, enfocando nos resultados estéticos da cicatriz e a evolução destes pacientes, aplicando as técnicas de ressecção em bloco do Professor Ronaldo Pontes (RP).
Métodos: O estudo foi uma série retrospectiva de casos de 124 pacientes, entre março de 2014 a março de 2017, submetidos à abdominoplastia em bloco pela técnica RP.
Resultados: Na nossa casuística, demonstrou-se uma mínima incidência de complicações encontradas com a técnica em Bloco RP, em comparação às encontradas na literatura, e, também, demonstrou um número pífio de casos de alterações na cicatrização.
Conclusão: A técnica descrita e suas variantes atendem a necessidade de diversos tipos de casos e garantem cirurgias seguras e eficazes, com resultados muito satisfatórios, sendo uma técnica reprodutível.
Palavras-chave: Abdominoplastia; Seroma; Hematoma; Cicatriz hipertrófica; Queloide
INTRODUCTION
In 1889, Kelly was the first to use the expression "abdominal lipectomy"1 when he performed a transverse dermal adipose excision that included the navel. Abdominoplasty is among the most commonly performed aesthetic procedures that encompass both aesthetic features and abdominal wall structural reconstruction2. Due to the number of variations and modifications of abdominoplasty procedures, it is essential that surgeons select the appropriate technique based on the patient's characteristics to minimize postoperative morbidity and disability while achieving a desirable and predictable result3.
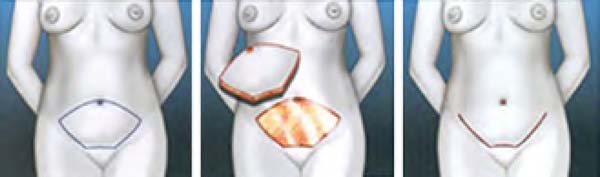
Abdominoplasties were initially performed using a low incision, cranial flap separation, treatment of the aponeurosis muscle, caudal traction, resection, navel transposition, and wound closure. This type of procedure often results in asymmetrical healing due to flap traction irregularities. In the adipose abdomen, this problem was aggravated by difficulty supporting an extremely heavy flap during the dissection4. For this reason, in the early 1960s, the previously marked flap was resected in block using lateral dissection to facilitate the surgical procedure, provide better bleeding control, and reduce the operative time. With technical improvements and experience with different cases, in 1971, four types of horizontal resections and their application were idealized in several cases by following the same principle5.
OBJECTIVE
This study aimed to demonstrate our experience with abdominoplasty focusing on the scar aesthetic results and the evolution of these patients with application of the block resection technique developed by Professor Ronaldo Pontes (RP).
METHODS
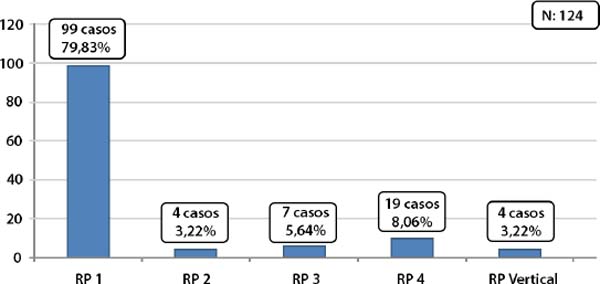
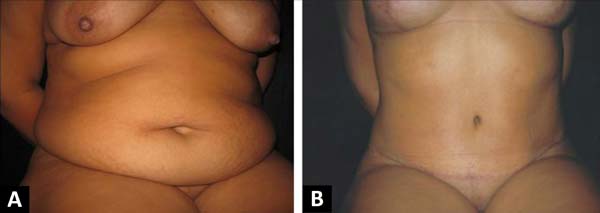
This retrospective observational series consisted of data collection from medical records comprising a total of 124 patients (122 women, 2 men) who underwent block abdominoplasty surgery (Figure 1) using the RP block resection technique between March 2014 and March 2017 with respect of the individualization of all four of its variants (Chart 1).
| 1. | Marking of the block abdominal incision (RP technique) with the patient in the standing and lying positions; |
| 2. | Pneumatic boot placement; |
| 3. | Patient in horizontal dorsal decubitus position with asepsis and antisepsis and placement of sterile fields under general anesthesia; |
| 4. | Local infiltration with anesthetic solution*; |
| 5. | Incision of excess tissue according to previous and circumferential navel marking; |
| 6. | Resection of excess tissue previously marked, keeping the navel inserted in the aponeurosis**; |
| 7. | Tunnel flap detachment up to the xiphoid process with plicature marking of the muscle-aponeurotic system of the abdominal rectum; |
| 8. | Plicature according to the marking, with number 0 Prolene thread and navel fixation in the aponeurosis with four cardinal points; |
| 9. | Flap caudal traction to mark the onphaloplasty on the skin as a Y (3-point star); |
| 10. | Review of hemostasis and introduction of a closed suction drain system (exiting in the pubic region); |
| 11. | Confection of Baroudi adhesion points; |
| 12. | Onphaloplasty, resulting in an equilateral triangle (directed to the pubis); |
| 13. | Flap synthesis in three planes; and |
| 14. | Local dressing. |
Type I (RP1) - Indicated in patients with supra- or infraumbilical flaccidity. The cranial tracing of the ellipse passes just above the umbilical scar, descending gently on both sides to the middle of the lateral part of the bikini demarcation. The lower tracing has three segments: two lateral cranial concavity segments and the suprapubic arch, which has a slight caudal concavity and a diameter inferior to that of the pubis. The two lower lateral arches must also be curved, with opposite curvature to the upper ones, to create a slightly curved scar with superior concavity.
Type II (RP2) - Also called the mini abdomen, the ellipse occupies the lower third between the navel and the pubis. This variant is indicated for patients with only infraumbilical flaccidity without the need for plicature of the rectus abdominis muscles. The indication of Type II should be extremely careful and should be denied when there is significant flaccidity in the epigastric region.
Type III (RP3) - Indicated exclusively for patients with a high umbilicus and infraumbilical flaccidity. The design is identical to that of Type II, with the difference being that the umbilical scar is sectioned at its base; after cranial dissection and plicature of the abdominal rectus muscles, it is reinserted below its original point, resulting in navel lowering of about 2 cm.
Type IV (RP4) - Indicated in patients with supra- or infraumbilical flaccidity with no indication of other variants. The marking is similar to Type I, but the cranial tracing of the ellipse passes just below the umbilical scar, where it subsequently has an original point closed longitudinally since it is not included in the area to be resected. The flap descends normally and the navel is transposed, similar to a typical abdominoplasty, resulting in an inverted T-incision.
Vertical - For cases in which there is a previous vertical supraumbilical scar or in cases with skin redundancy in which the cost-benefit favors the vertical scar.
Professor Baroudi's adhesion points were used in these abdominoplasty techniques.
The exclusion criteria in the study were: patients younger than 18 years or older than 65 years, body mass index (BMI) less than 20, previous cavitary gynecological surgery, abdominal deformities after abdominal or bariatric surgery, positive screening for breast cancer, and intentions of pregnancy.
The inclusion criteria in the study were: patients between 18 and 65 years if age, patients with supraumbilical and infraumbilical skin flaccidity, presence of abdominal rectus muscle diastasis, patients with satisfied progeny and body mass index above 20 (Table 1).
| Body mass index (kg/m2) | Frequency | % |
|---|---|---|
| 20-22 | 13 | 10.40 |
| 23-25 | 48 | 38.80 |
| 26-28 | 35 | 28.20 |
| 29-31 | 15 | 12.10 |
| 32-34 | 8 | 6.50 |
| ≥35 | 5 | 4.00 |
A detailed physical examination was performed of all patients and the implications of an abdominal plastic surgery were thoroughly discussed with the patients, as was guidance on fertility, time required for recovery, walking with some flexion of the abdomen, length of stay, and the use of suction drains (Table 2). Routine laboratory tests, total abdominal and abdominal wall ultrasonography, and venous Doppler of the lower limbs were requested.
| Comorbidity | Frequency | % |
|---|---|---|
| None (healthy patient) | 84 | 67.74 |
| Diabetes | 4 | 3.22 |
| Hypertension | 15 | 12.09 |
| Hypothyroidism | 8 | 6.45 |
| Other | 15 | 12.09 |
In the postoperative period, all patients underwent prophylactic treatment for deep vein thrombosis using pneumatic boots in the preoperative and postoperative periods and clexane in the postoperative period. A written statement of clarification was provided, and photographic documentation was routinely performed.
The patients were followed up daily for the first two postoperative days and weekly during the first month, followed by once a month. The aesthetic result was evaluated at 6 months postoperative.
RESULTS
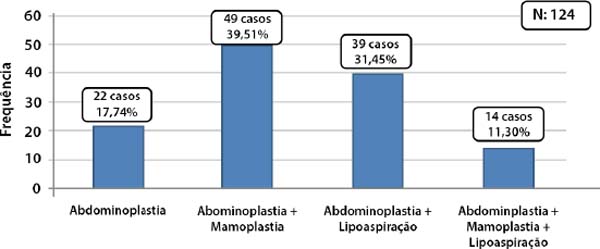
The mean patient age was 44.5 (range, 18-63) years (Table 3). The mean surgical time was 154 (range, 100-250) minutes. The mean indwelling drain time was 7 days to chart 2. The surgeries associated to abdominoplasties are presented in chart 2 and 3.
| Age (years) | Frequency | % |
|---|---|---|
| 18-30 | 20 | 16.12 |
| 31-45 | 67 | 54 |
| 46-60 | 33 | 27 |
| 61-65 | 4 | 3 |
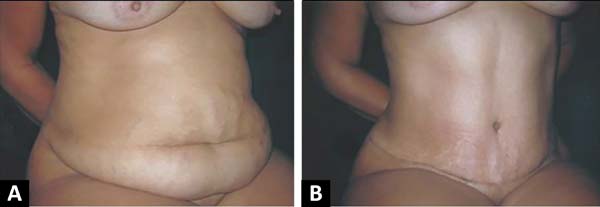
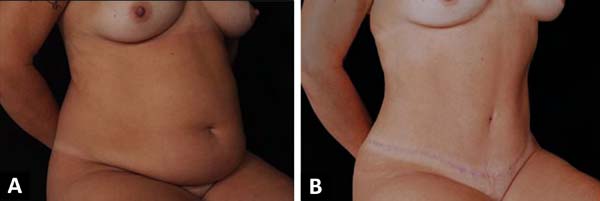
In our study, there was a decreased incidence of complications noted with the RP block abdominoplasty technique compared to those in the literature (Table 4). We observed a small number of cases of healing changes (Table 5). Patients who underwent surgery had a high degree of morphological and functional satisfaction.
| Complication | Frequency (%) | Literature (range, %) |
|---|---|---|
| Seroma | 1.61 (2 cases) | 1.0-4.2 |
| Hematoma | 0.80 (1 cases) | 5.0-6.1 |
| Surgical site infection | 0.00 (0 cases) | 2.2-7.3 |
| Flap necrosis or loss | 0.80 (1 cases) | 4.8-6.0 |
| Deep vein thrombosis | 0.00 (0 cases) | 1.0-1.1 |
| Pulmonary embolism | 0.00 (0 cases) | 0.5-0.8 |
| Complication | Frequency (N = 124) | % |
|---|---|---|
| Without complications | 118 | 95.18 |
| Wound dehiscence | 0 | 0.00 |
| Hypertrophic scar | 2 | 1.61 |
| Keloid scars | 1 | 0.80 |
Case 4
Procedure To Guarantee Ethical Aspects
The study was conducted with data obtained from the surgeon's personal files. There was no direct contact with the patients; therefore, no informed consent was required. The identity of the patients who participated in the study remained anonymous since their identities were not necessary for the study.
We agreed to abide by the ethical and moral principles that should govern all research involving human beings, including the Declaration of Helsinki, Belmont Report, Good Clinical Practice, and the Ethical Standards and Criteria set forth in codes of ethical confidentiality and/or current laws. We also respected the data confidentiality obtained from clinical records and any other data collection methods to prevent disclosing any information that would allow us to identify the subjects.
Authorization was requested from the authorities of the Niterói D'Or Hospital, as was approval from the Institutional Ethics Committee.
DISCUSSION
The methods and approaches differed greatly among the literature reviews6-12 and using comparisons with retrospective studies as a discussion point. Thus, we tried to bypass the discrepancies by defining the facts with a simple objective and comparing the most common complications with our evidence.
The practice of combined surgeries increases the risk of morbidity, consequently increasing length of hospital stay, blood transfusion index in the intra- and postoperative periods, and the incidence of thromboembolism and severe infections13-15. We believe that common sense is essential to evaluating a procedure's cost-effectiveness to enable understanding of the safety of performing surgeries combined with abdominoplasty.
The advantages of the RP technique are to simplify resection, dispense the need to hold a very long and heavy flap during dissection, facilitate bleeding control, ensure better symmetry of the resulting scar, drastically reduce procedure time, and stimulate the best preoperative planning. The flap marking to be resected is usually made the day before or in the ward, as it reduces operating room use time and patient anesthesia time5, thus minimizing complications and scar defects.
We emphasize that, among all complications, deep vein thrombosis (DVT) and pulmonary embolism are the most dramatic. The incidence of DVT in patients undergoing general surgery is reportedly 6-12%9, while the incidence of pulmonary embolism is 1.5%9. These events were avoided in our cases due to knowledge of their pathophysiology, use of preventive measures, and short surgical time.
CONCLUSION
The RP technique and its variants meet the need for several types of cases, ensure safe and effective surgeries, and are reproducible.
The prevention of hematomas and seromas occurs through rigorous hemostasis, the use of adhesion points and suction drains to prevent prolonged active drainage, and thus minimizing rates of these complications associated with adequate postoperative guidance. Therefore, knowledge of the pathophysiology, use of prophylactic measures, and the use of a technique with shorter surgical time reduced the risk of thromboembolic events and consequently the occurrence of pulmonary embolism. Hence, we provided excellent patient care and achieved a high degree of morphological and functional satisfaction.
COLLABORATIONS
|
LXB |
Conceptualization, Final manuscript approval, Investigation, Realization of operations and/or trials, Resources, Supervision, Writing - Original Draft Preparation |
|
ACAMD |
Resources, Supervision |
|
RAK |
Analysis and/or data interpretation, Data Curation, Formal Analysis, Investigation, Methodology, Writing - Original Draft Preparation, Writing - Review & Editing |
|
ROL |
Analysis and/or data interpretation, Conceptualization, Data Curation, Formal Analysis, Writing - Original Draft Preparation, Writing - Review & Editing |
|
GHP |
Final manuscript approval, Supervision, Validation, Writing - Original Draft Preparation |
REFERENCES
1. Kelly HA. Excision of the flat abdominal wall lipectomy. Surg Gynec Obstet. 1910;10:229-231.
2. Callia W. Contribuição para o estudo da correção cirúrgica do abdome pêndulo e globoso-técnica original [tese]. São Paulo: Universidade de São Paulo, Faculdade de Medicina; 1965.
3. Grazer FM. Abdominoplasty. Plast Reconstr Surg. 1973 Jun;51(6):617-23.
4. Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000;105(4):1499-516.
5. Pontes R. Abdominoplastia - Ressecção em Bloco e sua Aplicação em Lifting de Coxa e Torsoplastia. São Paulo: Revinter; 2004.
6. Dillerud E. Abdominoplasty combined with suction lipoplasty: a study of complications, revisions and risk factors in 487 cases. Ann Plast Surg. 1990 Nov;25(5):333-8.
7. Nurkim MV, Mendonça LB, Martins PAM, Silva JLB, Martins PDE. Incidência de hematoma e seroma em abdominoplastia com e sem drenos. Rev Soc Bras Cir Plást. 2002;17(1):69-74.
8. Jaimovich CA, Mazzarone F, Parra JFN, Pitanguy I. Semiologia da parede abdominal: seu valor no planejamento das abdominoplastias. Rev Soc Bras Cir Plást. 1999;14(3):21-50.
9. Abs R. Accidents thromboemboliques en chirurgie plastique: revue de la literature et proposition d´un algorithme de prophylaxie. Ann Chir Plast Esthet. 2000;45(6):604-9.
10. Anger J, Baruzzi AC, Knobel E. Um protocolo de prevenção de trombose venosa profunda em cirurgia plástica. Rev Bras Cir Plást. 2003;18(1):47-54.
11. Weinmann EE, Salzman EW. Deep-vein thrombosis. N Engl J Med. 1994;331(24):1630-41.
12. Jatene PR, Jatene MC, Barbosa AL. Abdominoplastia: experiência clínica e revisão da literatura. Rev Bras Cir Plást. 2005;20(2):65-71.
13. Almeida EG, Almeida Júnior GL. Abdominoplastia: Estudo Retrospectivo. Rev Bras Cir Plást. 2008;23(1):1-10.
14. Oliveira EA, Valera F, Monte ALR, López C. Prevenção do seromas nas abdominoplastias associadas à lipoaspiração e sem drenagem ativa. Rev Soc Bras Cir Plást. 2008;23(1):41-7.
15. Arantes HL, Rosique RG, Rosique MJF, Mélega JMA. Há necessidade de drenos para prevenir seroma em abdominoplastias com pontos de adesão?. Rev Bras Cir Plást. 2009;24(4):521-4.
1. Hospital Niterói D'Or, Serviço de Pós-Graduação em Cirurgia Plástica Prof. Ronaldo
Pontes Niterói, RJ, Brazil.
Corresponding author: Leonardo Xavier Braga Rua Otávio Carneiro, 143, Sala 401, Icaraí, Niterói , RJ, Brazil. Zip code: 24220-000. E-mail: leonardoxbraga@yahoo.com
Article received: June 4, 2018.
Article accepted: October 21, 2019.
Conflicts of interest: none.

















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter