

Original Article - Year 2019 - Volume 34 -
Rhytidoplasty practices and histological notes for the facial skin of post-bariatric patients
Condutas na ritido plastia e apontamentos histológicos na pele da face do paciente pós-bariátrica
ABSTRACT
Introduction: The number of patients classified as overweight or obese has resulted in an increased number of post-bariatric patients, generating a demand for rhytidoplasty in this public profile. expose the routine and surgical tactics in a teaching hospital, patient profiles, subcutaneous cellular tissue, and the superficial musculoaponeurotic system are compared between post-bariatric and non-post-bariatric patients, as well as histological superficial comparison of the skin.
Methods: A review of the data of 32 cases treated in 2012-2016 was conducted in a public hospital in Goiânia-GO.
Results: The tactics of rhytidoplasty used in post-bariatric patients do not differ significantly from those used in nonpost- bariatric patients. A histopathological analysis of the collected samples showed marked differences between post-bariatric and non-post-bariatric patients.
Conclusion: The surgical technique of rhytidoplasty of post-bariatric patients sustained specific details with satisfactory postoperative surgical results, skin with worse histological quality, perioperative complications within the expected range, and the need for further studies to assess the procedure's durability
Keywords: Rhytidoplasty; Bariatric medicine; Therapeutic practices; Histology; Face
RESUMO
Introdução: O número de pacientes classificados com sobrepeso ou obesos e, com isso, dos pacientes pós-bariátricas vem aumentando, gerando uma demanda por ritidoplastias neste perfil de público. O objetivo é expor a rotina e táticas cirúrgicas em um hospital de ensino, o perfil destes pacientes, além de um comparativo superficial histológico da pele, tecido celular subcutâneo e SMAS, entre os pacientes pós e não pós-bariátrica.
Métodos: Foi realizado revisão de dados do centro cirúrgico e de prontuário entre os anos de 2012 e 2016 em um hospital público na cidade de Goiânia-GO, com levantamento de 32 casos.
Resultados: A tática de ritidoplastia utilizada nos pacientes pós-bariátrica não apresenta grandes diferenças entre a utilizada nos pacientes não pós-bariátrica. A análise histopatológica das amostras colhidas evidenciou diferenças marcantes entre os pacientes pós e não pós-bariátrica.
Conclusão: Percebeu-se que a técnica operatória na ritidoplastia do paciente pós-bariátrica sustentou detalhes específicos, com resultado cirúrgico pós-operatório satisfatório, uma pele de pior qualidade histológica, com complicações perioperatórias dentro do esperado e com necessidade de maiores estudos para avaliar durabilidade do procedimento.
Palavras-chave: Ritidoplastia; Medicina bariátrica; Condutas terapêuticas; Histologia; Face
INTRODUCTION
The number of patients classified by the World Health Organization (WHO) as overweight (body mass index [BMI] > 25 kg/m2) or obese (BMI > 30 kg/m2)1 has been increasing in developing and developed countries, with an estimated 1.7 billion people in these categories2. Thus, the number of patients who manage to lose weight through lifestyle changes or bariatric surgery is also increasing.
Despite the advantages and disadvantages associated with great loss of adipose tissue after bariatric surgery, excess skin remains thereafter. This can be considered unesthetic to society and the patient himself, causing a psychological impact3, which creates a demand for surgical repair involving dermolipectomy in about one third of patients who stabilize their weight2.
Reparative plastic surgeries of patients after massive weight loss (MWL), that is those who lose at least 45 kg or 50% of their body weight, have recently increased2,4; among them, rhytidoplasty is the least performed since the face is generally less affected by substantial fat loss2,5,6. However, the demand for this surgery is growing.
Patients in whom weight loss affects the face present with a cutaneous surplus and laxity of the platysma muscle, developing something similar to a "jowl," "dewlap," or "turkey neck"2,6,7 besides evident nasogenian grooves in the middle region of the face, chin, perioral and periorbital areas, and eyelids, as well as the tip of the nose and earlobes in such a way that the context contributes to the aspect of early aging.
To correct this aspect with the most esthetic and lasting results possible, we used several surgical tactics that still meet patients' tissue quality. Due to the fact that postoperative bariatric patients do not adequately absorb nutrients, they end up experiencing a loss of skin tone and consistency and the superficial musculoaponeurotic system (SMAS)4,8-10.
OBJECTIVE
This study aimed to explore the routine surgical tactics in the treatment of cutaneous flaccidity and the SMAS in the face, neck, and platysma muscle of post-bariatric patients in a teaching hospital, in addition to a superficial histological comparison between their skin, subcutaneous cellular tissue, and the SMAS and those of the non-post-bariatric ones, showing the experience of the authors.
METHODS
Operating room and medical record data of 2012-2016 were reviewed, and we surveyed all post-bariatric patients who underwent rhytidoplasty at the Dr. Alberto Rassi Hospital - General Hospital of Goiânia (HGG) in Goiânia-GO. The authors of this study declare that the principles of the Declaration of Helsinki revised in 2000 were followed, as was Resolution 196/96 of the National Health Council. All patients signed an informed consent form prior to surgery. The present study was approved by the Research Ethics Committee of Dr. Alberto Rassi Hospital - HGG.
Patients who underwent rhytidoplasty after losing at least 22 kg or 23% of their body weight by bariatric surgery regardless of the technique and who achieved weight stability for at least 18 months were included in the study.
We aimed to determine the number of primary and secondary cases and stratify them by sex, mean age, BMI at the time of surgery, and intra- and postoperative complications.
Rhytidoplasty was the technique most commonly used by the team. This technique started with an anesthetic procedure, most of it being performed using the infiltration of anesthetic solution (0.5% lidocaine) and adrenaline (1:160,000 dilution); one extremely collaborative patient allowed the use of local analgesia only. We marked the facial midline, the area to be detached (lateral zygomatic, preauricular, posterior mandibular, and cervical regions), and the site to be incised (preauricular, intracapillary temporal, and retroauricular contour) (Figure 1). The platysma muscle was accessed using a submental incision, enabling its plicature, treatment with poliglecaprone 4.0, and simple stitches with spilled knots. In the face's detached lateral region, marking of the SMAS redundant portion is performed, plicature may be performed5,11, or when the tissue is exuberant and presents with bulging by simple plicature, SMASectomy may be performed (Figure 2). The skin flap is repositioned via resection of its excess (Figures 3 and 4) and sutured by planes with poliglecaprone 5.0 and Prolene 5.0 continuous stitches. In men, the technique is different in that we make an incision in the rib fold region. In all cases, a vacuum drain is introduced; it is removed when the output is equal to or less than 20 mL/24 hours and the aspect is serous.
Suture removal occurs at 5-10 days postoperative, with weekly return up to 28 days and results evaluated after 4-6 months.
The service routinely pays special attention to the patient's nutritional status and provides nutritional supplementation (vitamin B12, elemental iron, fat-soluble vitamins, calcium citrate, protein, etc.) whenever the results for a control laboratory test were altered in the presurgical evaluation. Whenever possible, the parenteral route was preferred for supplementation, which lasted for the period necessary to achieve the goals (minimum laboratory reference values).
Histopathological study of the skin, fat tissue, and SMAS of randomized patients was performed for comparative analysis. Samples were collected during the rhytidoplasty procedure from 6 randomly chosen post-bariatric patients at 1 year postoperative in the digestive tract and compared with 4 non-post-bariatric patients (who, for this reason, did not participate in the study sampling). The mean age of the post-bariatric patient group in this sample was 51 years, while that of the group of non-post-bariatric patients was 59 years. There was no sex-based difference in these sample groups. Samples were collected and immediately fixed in 10% formaldehyde solution. The fixed material was embedded in paraffin and subjected to microtomy and specific staining. The prepared samples were referred for analysis by the same pathologist, who followed a staining protocol consisting of hematoxylin and eosin in addition to Masson's trichrome. They were then subjected to a 100× and 200× optical microscopy assessment and images were obtained using a digital camera coupled to the microscope.
RESULTS
During the analysis period, 32 patients (24 women, 8 men; mean age, 55 years; age range, 46-61 years) underwent surgical treatment (Figures 5 and 6) and achieved weight stability for a mean 3.5 years. All patients underwent primary rhytidoplasty.
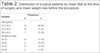
The patients had a mean BMI at the time of surgery of 27.4 kg/m2 (Table 1). The mean weight loss was about 40% of the initial weight, approximately 47 kg (Table 2). No intraoperative complications were reported; regarding postoperative complications, there were reports of small foci of unilateral preauricular epidermolysis in 6 cases (18.8%), which were treated with usual dressings and small volumes of unilaterally organized hematomas, as well as preauricular in 8 cases (25.0%), 4 of which were concomitant with epidermolysis (Table 3) and treated with simple drainage. The procedure lasted for a mean 4 hours and 20 minutes.
| Variable | Frequency | |
|---|---|---|
| n* | % | |
| Sex | ||
| Male | 8 | 25.0% |
| Female | 24 | 75.0% |
| Age | ||
| 45-55 | 15 | 46.9% |
| 55-65 | 17 | 53.1% |
* n = número de pacientes.
| Variable | Frequency | |
|---|---|---|
| n* | % | |
| BMI (kg/m2) | ||
| 18.5-24.9 | 15 | 46.9% |
| 25.0-29.9 | 10 | 31.2% |
| 30.0-34.9 | 7 | 21.9% |
| Weight loss (kg) | ||
| 20-35 | 10 | 31.3% |
| 36-50 | 8 | 25.0% |
| 51-65 | 12 | 37.5% |
| 66-80 | 2 | 6.3% |
| Postoperative complication | Frequency | |
|---|---|---|
| Number of complications | % | |
| Only unilateral pre-auricular epidermolysis | 2 | 6.3% |
| Few organized unilateral hematoma | 4 | 12.5% |
| Organized hematoma and epidermolysis concomitant and unilateral |
4 | 12.5% |
Histopathological analysis of the samples collected from the skin (Figures 7, 8, 9 e 10), adipose tissue (Figures 11 e 12), and SMAS (Figures 13 e 14) of postoperative patients indicated increased edema, peripheral lymphohistiocytic inflammatory activity, and severe epidermis hypotrophy; increased inflammatory activity and edema in all adipose tissue; and decreased fibrous collagen tissue thickness and presence of fibroconjunctive tissue with decreased vascularization in SMAS compared to non-post-bariatric patient skin.
DISCUSSION
Bariatric surgery has emerged as an effective and rapid possibility of weight control in obese patients who seek to improve their health status along the lines recommended by the World Health Organization, not only disease absence (hypertension, coronary disease, pulmonary hypertension, diabetes, dyslipidemias, gastroesophageal reflux disease, skin mycoses, etc.)7,12, but their complete physical, mental, and social well-being.
Plastic surgery plays a crucial role in healthy outcomes, promoting surgeries that, roughly speaking, could even be called inclusion procedures since the patient whose face was quickly transformed by weight loss can have his facial pattern restored. Because the face is an area that the patient cannot camouflage using clothing, the surgical procedure allows the patient to feel like the individual that he or she was before, to better accept themselves and be better accepted by society.
Rhytidoplasty is indicated for patients after MWL, when they achieve weight stability. The greatest weight loss usually occurs at about 12-18 months after bariatric surgery, and it is prudent to wait about 4-6 months after that to assess whether the plateau is maintained13. However, in our service, although we always wait for weight stability, it was not always necessary to wait for a 45-kg loss (or 50% of the initial weight, defined as massive weight loss) since many patients already complained and presented good surgical indications even before that. These patients presented satisfactory postoperative surgical results in relation to the initial flaccidity, with frank rejuvenation and restructuring of the face and neck esthetic pattern.
Knowledge about facial changes resulting from aging is better established than that involving changes in facial skin structure and histology resulting from MWL; however, this group shows turgor decreases and losses of subcutaneous fat14,15. Skin thickness tends to decrease in the facial region12,15 despite signs of increased or no difference in thickness in other regions12. Additionally, there is an increase in the expression of collagen type III, an immature collagen with lower healing capacity12,16,17; fibers become fewer and wider in number12,17,18; besides histological changes compatible with aging, such as loss of collagen fiber cohesion and enzymatic degradation of loose tissue12,14,15,17,19.
It is not uncommon for post-bariatric patients to experience nutritional changes. The literature suggests the use of nutritional supplementation to prevent or treat nutritional deficiencies resulting from anatomical changes caused by surgical techniques8,20-28.
The main complications associated with rhytidoplasty in post-MWL patients are hematomas and edemas, which usually disappear in about 2-3 weeks; paresthesia, with significant improvement by about 2-3 months postoperative; and rare reports of skin necrosis or paralysis of the mime muscles due to facial nerve injury, or even hypertrophic or keloid scars in the retroauricular zones2, but the main complications in our study were small foci of organized preauricular hematoma in 25% of cases, followed by small areas of unilateral preauricular epidermolysis in 18.8% of cases. There are authors who do not perceive an influence of MWL on the increase of postoperative complications compared to control groups29.
CONCLUSION
The surgical technique of rhytidoplasty in post-bariatric patients follows general principles except for specific details of this group of patients, such as the most aggressive plicature and treatment of the platysma muscle and the eventual need for SMASectomy. Patients in the study group presented skin of worse histological quality compared to those without the nutritional difficulties arising from weight reduction surgery. That is, postoperative bariatric skin presents a worse collagen fiber arrangement as well as exacerbation of the local inflammatory reaction, which in theory hinders the healing process and procedure durability and increases the risk of local complications. Nevertheless, perioperative complications were not different than expected, even for patients who did not undergo bariatric surgery. Further studies are needed to establish conclusions regarding the procedure's durability.
COLLABORATIONS
|
HLFG |
Analysis and/or data interpretation, Conception and design study, Conceptualization, Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Resources, Supervision, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
MGXPP |
Analysis and/or data interpretation, Data Curation, Formal Analysis, Funding Acquisition, Investigation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
DVS |
Analysis and/or data interpretation, Data Curation, Formal Analysis, Funding Acquisition, Investigation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
RKF |
Analysis and/or data interpretation, Data Curation, Formal Analysis, Funding Acquisition, Investigation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
|
RK |
Analysis and/or data interpretation, Conception and design study, Conceptualization, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation, Methodology, Project Administration, Realization of operations and/or trials, Resources, Supervision, Validation, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
REFERENCES
1. World Health Organization (WHO). Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation (WHO Technical Report Series 894. Geneva: WHO; 2000.
2. Pallua N, Demir E. Postbariatrische Plastische Chirurgie. Der Chirurg. 2008 Sep;79(9):843-53.
3. Baillot A, Brais-Dussault E, Bastin A, Cyr C, Brunet J, Aimé A, et al. What Is Known About the Correlates and Impact of Excess Skin After Bariatric Surgery: a Scoping Review. Obes Surg. 2017 Sep;27(9):2488-2498.
4. Cabbabe SW. Plastic Surgery after Massive Weight Loss. Mo Med. 2016 May/Jun;113(3):202-6.
5. Furtado IR, Nogueira CH, Lima Júnior EM. Cirurgia Plástica após a Gastroplastia Redutora: Planejamento das Cirurgias e Técnicas. Rev Bras Cir Plást. 2004;19(2):35-40.
6. Kaluf R, Azevêdo FN, Rodrigues LO. Sistemática Cirúrgica em Pacientes Ex-Obesos. Rev Bras Cir Plást. 2006;21(3):166-174.
7. Sclafani AP. Restoration of the jawline and the neck after bariatric surgery. Facial Plast Surg. 2005 Feb;21(1):28-32.
8. Nirujogi VL, Zopfi K. Considerações nutricionais para cirurgia plástica em paciente após cirurgia bariátrica. Rev Bras Cir Plást. 2015;30(2):295-302.
9. Gunnarson GL, Frøyen JK, Sandbu R, Thomsen JB, Hjelmesæth J. Plastic surgery after bariatric surgery. Tidsskr Nor Legeforen. 2015 Jun;135(11):1044-9.
10. Migliori FC, Robello G, Ravetti JL, Marinari GM. Histological alterations following bariatric surgery: pilot study. Obes Surg. 2008 Oct;18(10):1305-7.
11. Stocchero IN, Stocchero GF, Stocchero GF, Fonseca ASF. Método de avaliação da suspensão do SMAS no rejuvenescimento facial. Rev Bras Cir Plást. 2012;27(3):392-397.
12. Choo S, Marti G, Nastai M, Mallalieu J, Shermak MA. Biomechanical properties of skin in massive weight loss patients. Obes Surg. 2010 Oct;20(10):1422-8.
13. Chandawarkar RY. Body contouring following massive weight loss resulting from bariatric surgery. Adv Psychosom Med. 2006;27:61-72.
14. Halawi A, Abiad F, Abbas O. Bariatric surgery and its effects on the skin and skin diseases. Obes Surg. 2013 Mar;23(3):408-13.
15. Narasimhan K, Ramanadham S, Rohrich RJ. Face lifting in the massive weight loss patient: modifications of our technique for this population. Plast Reconstr Surg. 2015 Feb;135(2):397-405.
16. Manzoni APDS, Weber MB. Skin changes after bariatric surgery. An Bras Dermatol. 2015 Apr;90(2):157-68.
17. Light D, Arvanitis GM, Abramson D, Glasberg SB. Effect of weight loss after bariatric surgery on skin and the extracellular matrix. Plast Reconstr Surg. 2010 Jan;125(1):343-51.
18. Orpheu SC, Coltro PS, Scopel GP, Gomez DS, Rodrigues CJ, Modolin ML, et al. Collagen and elastic content of abdominal skin after surgical weight loss. Obes Surg. 2010 Apr;20(4):480-6.
19. Prist IH, Salles AG, Lima TM, Modolin ML, Gemperli R, Souza HP. Extracellular matrix remodeling derangement in ex-obese patients. Mol Cell Biochem. 2017 Jan;425(1-2):1-7.
20. Luna ICG, Cavalcanti ELF, Salgado IV, Melo DSF, Almeida ALMC, Pereira RMR. Cirurgia plástica pós-gastroplastia: perfil das deficiências nutricionais com implicações na cicatrização. Rev Bras Cir Plást. 2014;29(4):557-561.
21. Weng TC, Chang CH, Dong YH, Chang YC, Chuang LM. Anaemia and related nutrient deficiencies after Roux-en-Y gastric bypass surgery: a systematic review and meta-analysis. BMJ Open. 2015 Jul;5(7):e006964.
22. Bordalo LA, Teixeira TFS, Bressan J, Mourão DM. Cirurgia bariátrica: como e por que suplementar. Rev Assoc Med Bras. 2011;57(1):113-120.
23. Stein J, Stier C, Raab H, Weiner R. Review article: the nutritional and pharmacological consequences of obesity surgery. Aliment Pharmacol Ther. 2014 Sep;40(6):582-609.
24. Dagan SS, Goldenshluger A, Globus I, Schweiger C, Kessler Y, Sandbank GK, et al. Nutritional Recommendations for Adult Bariatric Surgery Patients: Clinical Practice. Adv Nutr. 2017 Mar;8(2):382-94.
25. Xanthakos SA. Nutritional deficiencies in obesity and after bariatric surgery. Pediatr Clin North Am. 2009 Oct;56(5):1105-21.
26. Gletsu-Miller N, Wright BN. Mineral malnutrition following bariatric surgery. Adv Nutr. 2013 Sep;4(5):506-17.
27. Bordalo LA, Mourão DM, Bressan J. Deficiências nutricionais após cirurgia bariátrica. Por que ocorrem?. Acta Med Port. 2011;24(S4):1021-1028.
28. Agha-Mohammadi S, Hurwitz DJ. Potential impacts of nutritional deficiency of postbariatric patients on body contouring surgery. Plast Reconstr Surg. 2008 Dec;122(6):1901-14.
29. Fearmonti RM, Blanton M, Bond JE, Pestana IA, Selim MA, Erdmann D. Changes in dermal histomorphology following surgical weight loss versus diet-induced weight loss in the morbidly obese patient. Ann Plast Surg. 2012 May;68(5):507-12.
1. Hospital Estadual Geral de Goiânia Dr. Alberto Rassi - HGG , Goiânia, GO, Brazil.
2. Hospital Universitário Ciências Médicas, Belo Horizonte, MG, Brazil.
Corresponding author: Hugo Leonardo Freire Gomes Avenida Dr. Ismerino Soares de Carvalho, 804 , Setor Aeroporto, Goiânia, GO, Brazil. Zip code: 74075-040. E-mail: hugoleo@yahoo.com.br
Article received: April 24, 2019.
Article accepted: October 21, 2019.
Conflicts of interest: none.

































 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter