

Original Article - Year 2019 - Volume 34 -
Secondary mammaplasty with monobloc resection and implant repositioning in the partial retropectoral pocket
Mamoplastia secundária com ressecção em monobloco e neoposicionamento do implante no espaço retropeitoral parcial
ABSTRACT
Introduction: Breast augmentation with silicone implants is one
of the most common plastic surgery procedures. The objective
of this study was to evaluate patients with previous silicone
implantations undergoing secondary mammaplasty, presenting
an alternative approach with en block resection of breast tissue,
fibrous capsule, and silicone implant, followed by implant
repositioning in the partial retropectoral pocket.
Methods: This study included 24 cases of secondary mammaplasty with
implant repositioning. It presents the indications for surgery and
details the surgical approach for easier procedures and more
satisfactory results.
Results: All the included cases presented
breast changes on physical examination, such as breast ptosis,
capsular contracture, improper implant position, and breast
asymmetry. In the studied cases, the use of polyurethane-coated
implants and their complete adherence to the fibrous capsule
resulted in a more practical resection even with varying degrees
of capsular contracture. Fibrous capsules of textured implants
were thinner, and implant instability due to the presence of
residual seroma or pockets bigger than necessary resulted in
more difficult resection.
Conclusion: Secondary mammaplasty
with en bloc resection, along with implant replacement
and repositioning in the partial retropectoral pocket with
sutures involving muscle and breast tissue is an alternative
to optimize the procedure, providing greater muscle stability
until complete healing and new fibrous capsule formation.
Keywords: Breast; Breast implant; Mammaplasty; Pectoral muscles; Capsular contracture in implants
RESUMO
Introdução: As cirurgias de aumento de mamas com implantes de silicone estão entre os procedimentos de cirurgia plástica mais realizados. O objetivo desse estudo é avaliar os casos de pacientes com prótese de silicone, submetidas à mamoplastia secundária, apresentando uma alternativa de abordagem com ressecção em monobloco do tecido mamário, cápsula fibrosa e prótese de silicone; e o neoposicionamento do implante em loja retromuscular peitoral parcial.
Métodos: Foram analisados 24 casos de mamoplastia secundária com neoposicionamento da prótese, apresentando os motivos da indicação da cirurgia e o detalhamento da abordagem cirúrgica para maior facilidade na execução do procedimento e a obtenção de resultados mais satisfatórios.
Resultados: Todos os casos operados apresentavam alterações no exame físico das mamas, como: ptose mamária contratura capsular, posicionamento inadequado dos implantes e assimetrias mamárias. Nos casos estudados, as próteses com revestimento de poliuretano e sua completa adesão à cápsula fibrosa permitiram a ressecção mais prática, mesmo com variáveis graus de contratura capsular. As cápsulas fibrosas que envolviam implantes texturizados tinham características mais finas e a instabilidade das próteses, pela presença de seroma residual ou pelo excessivo tamanho da loja da prótese, desencadearam maior dificuldade na ressecção.
Conclusão: A realização de mamoplastia secundária com troca de prótese, empregando a ressecção em monobloco e neoposicionamento do implante no espaço retromuscular peitoral parcial com suturas do músculo ao tecido mamário, oferece uma alternativa para otimizar o procedimento, maior estabilidade do músculo até completa cicatrização e a formação de nova cápsula fibrosa.
Palavras-chave: Mama; Implante mamário; Mamoplastia; Músculos peitorais; Contratura capsular em implantes
INTRODUCTION
Breast augmentation with a silicone implant is one of the most common plastic surgery procedures in Brazil and worldwide1-3. Considering that some of these patients may need some type of secondary intervention4-7, ranging from minor scar-repairing procedures to complex surgeries for complete breast reconstruction, it is important for plastic surgeons to be prepared to meet patient expectations and deal with possible difficulties.
Over the last decades, the rate of reoperations for breast augmentation has remained unchanged at about 20% after 3 years regardless of the type of implant8.
Therefore, it is important to know different secondary surgical methods in order to provide solutions for complex cases, inadequate results, and patients dissatisfied with primary surgery results.
OBJECTIVE
The objective of this study was to evaluate patients with previous silicone implantations undergoing secondary mammaplasty, presenting an alternative approach with en block resection of breast tissue, fibrous capsule, and silicone implant, followed by implant repositioning in the partial retropectoral pocket.
Methods
This was a cross-sectional retrospective study to analyze medical records and photographic documentation of patients who had undergone a primary breast implant surgery at least 6 months before the secondary breast surgery in the period from January 2013 to March 2017. All patients were operated by the author in his private clinic.
The analysis followed the principles of the Declaration of Helsinki (2000) and resolution 466/2012 of the National Health Council regarding ethical and legal aspects of research involving human beings in Brazil.
This study included 24 cases of breast surgery with en block resection and implant replacement and repositioning in the partial retropectoral pocket during the abovementioned period.
The patients were operated by the same professional, regardless of where the primary intervention was conducted. After an initial consultation with general evaluation and surgical planning, the patients underwent clinical and cardiological evaluation and were considered fit for the procedure.
The patients underwent laboratory screening, chest radiographic examinations, and breast imaging exams. According to age and need for diagnostic clarification, some patients underwent breast ultrasound, mammography, and/or nuclear magnetic resonance imaging. Patients had a consultation preferably one day before surgery for photographic documentation and clarification of any questions.
The surgery indication was based on the presence of at least one of the following criteria: patient’s motivation to improve breast esthetics; and changes on physical examination and/or imaging exams that justified mammaplasty with implant replacement.
Therefore, the objectives of the surgery were defined considering, above all, the patient’s expectations regarding breast size.
Progress and results were evaluated by comparative physical examination and using photographic records 60 days and 6 months after the procedure at regular postoperative consultations and considering the patients’ validation of results. Ultrasound examination was requested for all cases 6 months after the procedure to verify proper placement of the breast implants.
Preoperative marking
After marking the midline throughout the chest, breast markings began at point A, bilaterally. Point A corresponded to the new position of the nipple-areola complex (NAC), and so it was positioned on the mammary midline above the anterior projection of the mammary fold9-12. Points A were marked strictly equidistant to the thoracic midline (TML) and to the sternal notch to identify and correct NAC asymmetries.
Vertical lines were delimited by skin traction (medially and laterally) in relation to a point on the mammary fold (called point X), positioned at a distance 1 to 2 cm shorter than the distance from point A to the TML. After the vertical markings were defined, the points corresponding to the height of the lower border of the new areola position (called points B and C) and the future point of the junction of the vertical incisions in the mammary fold (called points D and E) were marked.
The distances of points B and C and D and E from point A were between 3.5 and 4 cm and 10 and 11 cm, respectively. This marking was based on overall breast characteristics (skin, breast tissue density, base diameter, and need for projection) and size of the implant to be used.
Next, horizontal resection lines were delimited by lines marked between points D and E and the medial and lateral extremities of the mammary fold line. During these markings, skin traction was very carefully applied so that points D and E were more distant than point X from the medial and lateral borders of the inframammary fold scar, in order to prevent over-resection and excessive tension in vertical sutures, especially with the use of larger implants.
Subsequently, all markings were photographed (Figure 1) and the positions of the future scars were shown to the patient.
The patients underwent general anesthesia or epidural block associated with intravenous sedation in a hospital environment, respecting the anesthetic criteria and the joint decision of the anesthetist and the patient. Analgesic, anti-inflammatory, and antibiotic medications were used during and after surgery.
Operative technique
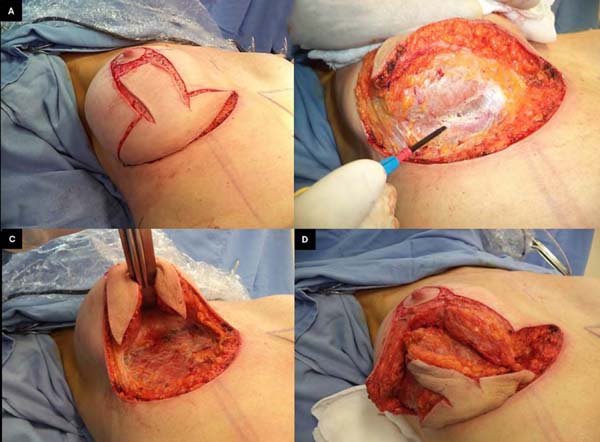
The patient was placed in the supine position with approximately 30° of elevation; skin incisions on the previous marking lines and de-epidermization of the periareolar skin were then performed (Figure 2A) for subsequent superior rotation of the NAC with the superior or superomedial pedicle13, according to the previously defined point A position or the need to adapt to breast tissue resections and size of the new implant. En bloc resection included excess skin and breast tissue at the lower breast pole, capsule, and implant (Figures 2B, 2C, and 2D). Microdissection needles (Colorado Type, Black & Black Surgical, Inc.) were used for electrocautery detachment to facilitate hemostasis and the perfect separation of the capsule and surrounding tissues.
After complete resection of the mammary tissue, capsule, and implant, no scar tissue or residual capsule was left. The detached area was then exhaustively washed with 0.9% saline solution and protected with a wet compresses for subsequent hemostatic testing when necessary.
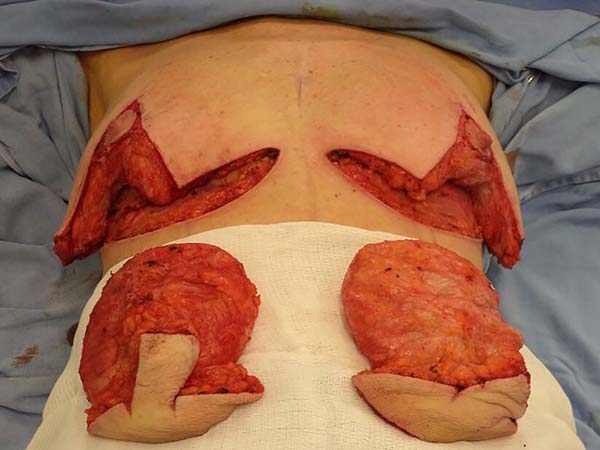
The same procedure was performed on the contralateral breast, followed by bilateral total en bloc resection of the structures (Figure 3). The capsule was opened outside the surgical field for analysis of integrity, deformities, type, and size of the patient’s implant (Figure 4). After delimitation and symmetrization of the detached areas in both breasts, bilateral retromuscular pockets were made starting with the incision of the pectoral muscle in the nearest portion of the mammary fold3,7 (Figure 5).
After detachment of the pectoralis major muscle up to the medial insertion limit - as necessary to accommodate the new implant and to avoid superior displacement due to pressure resulting from muscular action - hemostasis was rigorously tested in the anterior and posterior regions of the muscle, bilaterally.
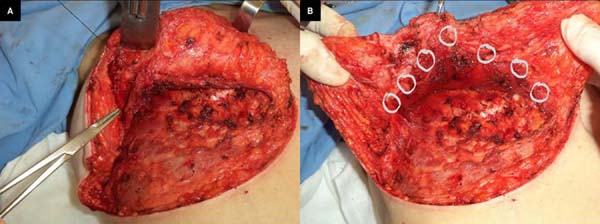
The pectoral muscle was sutured to the breast tissue to facilitate implant accommodation in the retromuscular pocket, avoiding migration of the implant to the anterior part of the muscle and providing muscle flap stability to the breast tissue. Suturing was started with a stitch on the mammary midline corresponding to the point of support at the level of the 4th or 5th intercostal space and NAC projection (Figure 6A). After that, two to four stitches were made on each side along the lower border of the pectoralis major muscle using Mononylon® 3.0 and inverted knot sutures so that the thread was not in direct contact with the silicone implant (Figure 6B).
After the implant (textured, round, high or super high profile, Eurosilicone, Mentor Corporation, or Natrelle brands) was accommodated in a partial retromuscular pocket, mammary suture was started at the junction of the pillars at the X-point projection, respecting anatomical planes and perfect accommodation of mammary, subdermal, and dermal tissue (Figure 7).
Closed suction drains were used for 1 to 5 days, depending on the volume and appearance of the drained fluid. The drains were placed in the submuscular pocket with some holes in the inferior lateral portion of the breast (Figure 8B). Right after surgery, it was possible to see adequate mammary tissue coaptation with the implant and greater breast support compared to those preoperatively (Figures 8A and 8B).
All patients received verbal and written instructions on specific postoperative care in order to avoid implant displacement, especially in the first 60 postoperative days.
RESULTS
The mean age of the operated patients was 50 years (minimum 24 and maximum 73 years) and the mean time since the first implant surgery was 10.1 years (minimum 1 year and maximum 25 years).
This study included 24 secondary mammaplasty procedures involving mammary implant replacement and repositioning in the partial retropectoral pocket during the study period. All cases presented breast changes on physical examination, including breast ptosis (moderate to severe), capsular contracture, improper implant positioning, and breast asymmetries.
Dissatisfaction with the results of the primary surgery was reported in 10 (41.6%) cases, and most of these patients had undergone breast augmentation mammaplasty less than 10 years before. The other 14 (58.4%) patients reported being satisfied with primary surgery results; however, the changes that appeared over time motivated them to undergo a new surgery.
Implant-related changes in image examinations (mammography, ultrasound, and/or nuclear magnetic resonance) were described in 7 (29.1%) cases. Capsular contracture (Baker Classification II14 or above) was identified during physical examination and in imaging exams in 7 (29.1%) cases, and 2 (8.3%) cases showed evidence of intracapsular implant rupture. Six (25%) primary breast augmentation procedures were performed by the author and 18 (75%) by other professionals.
Of the cases in which the patient’s clinical history was not available, the implant volume was accurately reported or some type of implant documentation was maintained in only 4 (22.2%). Thus, implants with volumes different than those reported by patients were found in 14 cases, corresponding to 77.7% of surgeries. Implant volume could not be identified in one case because the patient had no relevant information on volume and it was a ruptured smooth implant. It was the oldest implant (25 years) analyzed. During surgery, textured implants were identified in 16 (66.6%) patients, polyurethane-coated implants in 7 (29.1%), and smooth implants in 1 (4.1%).
The mean volume of the implants replaced during surgery was 233 cc (minimum 135 cc and maximum 300 cc) on the right side and 235 cc (minimum 135 cc and maximum 375 cc) on the left side. The mean volume of the implants repositioned during surgery was 341 cc (minimum 200 cc and maximum 450 cc) on the right side and 341 cc (minimum 220 cc and maximum 450 cc) on the left side. The mean volume of the implants used was the same for both sides, although different sized implants were used to compensate for asymmetries that could not be corrected only by resecting excess skin and breast tissue. Implant volume tends to be larger in secondary surgeries to compensate for glandular atrophy and provide greater breast tissue support, especially when placed in the retromuscular plane.
Table 1 shows information on patients’ complaints, medical evaluation, types of implant coating, and volume of implants replaced and repositioned in this study.
| Patient | Age | Time | Contracture | Rupture | Asymmetry | Ptosis | Image | Dissatisfaction | Others | Type of implant |
Right Pre | Right Post | Left Pre | Left Post |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CF | 45 | 5 | X | X | X | Textured | 260 | 350 | 260 | 350 | ||||
| SPP | 54 | 8 | X | Textured | 280 | 325 | 280 | 325 | ||||||
| TPB | 62 | 25 | X | X | X | X | X | X | Smooth | 280 | 280 | |||
| GP | 73 | 1 | X | X | X | Textured | 220 | 200 | 220 | 220 | ||||
| MDV | 52 | 9 | X | Textured | 240 | 325 | 240 | 325 | ||||||
| GDS | 61 | 17 | X | X | X | X | X | Polyurethane | 135 | 400 | 135 | 400 | ||
| IK | 41 | 9 | X | Textured | 300 | 300 | 300 | 300 | ||||||
| AS | 54 | 10 | X | X | X | X | Polyurethane | 260 | 325 | 260 | 325 | |||
| FR | 38 | 10 | X | X | Textured | 235 | 375 | 235 | 375 | |||||
| MG | 54 | 20 | X | X | X | Textured | 260 | 375 | 260 | 375 | ||||
| VP | 47 | 8 | X | Textured | 220 | 325 | 220 | 325 | ||||||
| RS | 47 | 12 | X | X | X | Textured | 175 | 375 | 175 | 375 | ||||
| IR | 60 | 2 | X | X | X | Polyurethane | 240 | 400 | 240 | 400 | ||||
| MFR | 24 | 4 | X | X | X | Textured | 285 | 350 | 285 | 375 | ||||
| LRL | 57 | 12 | X | Textured | 230 | 350 | 230 | 350 | ||||||
| EO | 39 | 4 | X | X | X | Textured | 250 | 350 | 250 | 350 | ||||
| AA | 46 | 15 | X | X | X | X | Polyurethane | 140 | 450 | 140 | 450 | |||
| JM | 33 | 3 | X | X | X | Textured | 260 | 350 | 260 | 350 | ||||
| BV | 58 | 13 | X | Textured | 280 | 350 | 280 | 350 | ||||||
| CF | 70 | 17 | X | X | X | X | Polyurethane | 190 | 300 | 190 | 300 | |||
| EA | 41 | 13 | X | X | Polyurethane | 175 | 375 | 175 | 375 | |||||
| IG | 51 | 10 | X | X | X | X | Polyurethane | 155 | 240 | 155 | 240 | |||
| RO | 49 | 6 | X | X | Textured | 300 | 310 | 375 | 265 | |||||
| EC | 44 | 10 | X | X | X | X | Textured | 285 | 420 | 255 | 420 |
There was no implant displacement, retroglandular migration, or breast asymmetry requiring corrective surgery at the evaluation 60 days after the surgery, using physical examination, photographic records, surgeon’s technical validation, and patients’ approval as parameters. The patients had no complaints of residual excess skin at the time of this evaluation. Mild to moderate mammary ptosis was reported in 3 (12.5%) cases, mainly related to weight loss during the period, previous presence of stretch marks, and sagging body skin. Additional skin resection was scheduled, without any need for direct intervention on breast implants.
The patients underwent breast ultrasound examinations 6 months after the surgery, which showed no implant rupture, contour irregularities, residual seroma, or other changes related to the surgery analyzed in this study.
Surgical complications included 4 cases of unilateral suture dehiscence in the inframammary fold, representing 8.3% of the 48 operated breasts. Partial unilateral areola necrosis occurred in one patient, corresponding to 2.8% of the operated breasts. This specific patient had undergone the primary procedure and two breast repair surgeries. All complications were resolved under local anesthesia. Complete suture dehiscence, hematoma, infection, or other major complications were not reported in the patients undergoing the procedure described in this study.
DISCUSSion
Given the significant number of women undergoing breast augmentation or breast repositioning surgeries with silicone implants in recent years, surgeons should find practical and objective secondary mammaplasty solutions, providing satisfactory results to patients and avoiding excessively long procedures or high blood loss.
In 2001, Melega et al.15 described the surgical approach for en bloc resection in cases of capsular contracture correction through an incision on the previous scar, dissecting the fibrous capsule with blunt scissors. This procedure was called “capsulectomy without capsulotomy”.
En bloc resection of the skin, mammary gland, fibrous capsule, and implant has multiple benefits during a highly complex surgery such as mammaplasty associated with implant replacement.
Some of the benefits are as follows:
a) Practical skin incisions: skin incision becomes practical with the support provided by the implant and its fibrous capsule, often hardened by capsular contracture, allowing precise incisions even on thin skin or with stretch marks;
b) Detachment plane control: implant stability prevents the capsule from bending during traction, facilitating detachment of the medial, lateral, and posterior portions and virtually eliminating the risk of capsule residues;
c) Hemostasis control: it is easier to visualize and cauterize blood vessels during resection when the contour of the fibrous capsule is detached, keeping the operative field clean and resulting in minimal blood loss;
d) Avoiding silicone and/or intracapsular secretion extravasation into the mammary tissue: the risk of contamination in implant replacement surgeries is significantly reduced without opening the capsule for implant removal. Even if the capsule is opened, it is possible to easily aspirate the intracapsular liquid content, avoiding contact of this content with adjacent tissues;
e) Objective mammary tissue resection and implant removal: reduced surgical time in the initial phase of the procedure provides safer mammary restructuring, reducing complications related to long-term surgery.
Different techniques to approach the fibrous capsule have been proposed in previous studies15-20, many of them preserving the whole capsule or part of it, with favorable results. However, the maintenance of fibrous tissue in contact with the implant, probably incorporating silicone gel extravasation residues, can have disastrous consequences, especially the occurrence of potential bacterial contamination and local infection, which would result in implant removal15,21-24.
A broad review of the literature on capsular contracture management shows that both capsulotomy and capsulectomy can be effective, suggesting total capsulectomy in cases of retroglandular implant contracture25.
In 2006, Spear20 described a technique for capsular contracture correction with total or partial capsulectomy and implant repositioning to the retropectoral plane using marionette half-mattress sutures to obliterate the subglandular space, obtaining satisfactory results with low risk of capsular contracture.
The complexity of the surgery and the instability of the structures mobilized in the presented procedure evidently require preventive measures to avoid implant detachment and migration to the retroglandular space, which would be disastrous, especially if unilateral. Thus, we used resistant and non-absorbable thread for direct suture with multiple stitches to achieve perfect adherence of the lower border of the pectoral muscle to the mammary tissue.
Although implants are not completely covered by the pectoral muscle, covering the superomedial portion of the implant provides a natural result. In addition, a careful detachment of the lower part of the pectoral muscle and the maintenance of medial and lateral insertions allow implant accommodation, providing greater stability and reduced risks of postoperative displacement3,19,26 (Figures 9A-9D).
In the studied cases, the use of polyurethane-coated implants and their complete adherence to the fibrous capsule resulted in a more practical resection even with varying degrees of capsular contracture. Fibrous capsules of textured implants were thinner, and implant instability due to the presence of residual seroma or pockets bigger than necessary resulted in more difficult resection.
The complication rate corroborated the results of previous studies, even considering the complexity of the procedure and the fact that these are secondary breast surgeries2,4,5,15,19. No interventions were required for surgical repair of residual breast ptosis, implant displacement, or breast asymmetries during the postoperative follow-up of the studied cases. Moreover, none of the cases presented capsular contracture until this manuscript was prepared. The results of this study show implant stability and low long-term capsular contracture index, even considering the relatively short follow-up period.
Proper planning and implant positioning are essential in breast augmentation surgeries. Therefore, it is important to know different secondary or reparative surgery methods in order to provide solutions for complex cases, inadequate results, and patients dissatisfied with primary surgery results.
CONCLUSION
En bloc resection and implant repositioning in the partial retropectoral pocket with sutures attaching the pectoralis major muscle to breast tissue is an alternative to improve secondary breast surgery, providing favorable results in cases of excessive mobility or capsular contracture in implants initially placed in the retroglandular position.
REFERENCES
1. Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2004 Oct;114(5):73E-81E. PMID: 15457008
2. Pitanguy I, Amorim NFG, Ferreira AV, Berger R, Análise das trocas de implantes mamários nos últimos cinco anos na Clínica Ivo Pitanguy. Rev Bras Cir Plást. 2010 Dec;25(4):668-674. DOI: https://doi.org/10.1590/S1983-51752010000400019
3. Zeitoune GC, Subpeitoral ou subglandular: qual é a melhor localização do implante para pacientes com hipomastia?. Rev Bras Cir Plást. 2012;27(3):428-34. DOI: https://doi.org/10.1590/S1983-51752012000300017
4. Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006 Mar;117(3):757-67. DOI: https://doi.org/10.1097/01.prs.0000201457.00772.1d
5. Sperly A, Bersou Júnior A, Freitas JOG, Michalay N. Complicações com próteses mamárias. Rev Soc Bras Cir Plást. 2000;15(3):33-46.
6. Slavin SA, Greene AK. Augmentation mammoplasty and its complications. In: Thorne CH, editor. Grabb & Smith’s plastic surgery. Philadelphia: Lippincott Williams & Wilkins; 2007. p.575-584.
7. Tebbetts JB. Dual plane breast augmentation: Optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006 Dec;118(7 Suppl):81S-98S. DOI: https://doi.org/10.1097/00006534-200612001-00012
8. Teitelbaum S. Abordagem do aumento das mamas em plano duplo. In: Aston SJ, editor. Cirurgia Plástica Estética. Elsevier. 2011;(54):675-687.
9. Hidalgo DA, Spector JA. Mastopexy. Plast Reconstr Surg. 2013 Oct;132(4):642e-656e. PMID: 24076713 DOI: https://doi.org/10.1097/PRS.0b013e31829fe4b4
10. De Benito J, Sánchez K. Key points in mastopexy. Aesthetic Plast Surg. 2010 Dec;34(6):711-5. PMID: 20499062 DOI: https://doi.org/10.1007/s00266-010-9527-5
11. Graf R, Biggs TM. In search of better shape in mastopexy and reduction mammoplasty. Plast Reconstr Surg. 2002 Jul;110(1):309-17;discussion:318-22. DOI: https://doi.org/10.1097/00006534-200207000-00053
12. Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011 Dec;128(6):1282-301. DOI: https://doi.org/10.1097/PRS.0b013e318230c884
13. Wada A, Millan LS, Gallafrio ST, Gemperli R, Ferreira MC. Tratamento da ptose mamária e hipomastia utilizando técnica de mamoplastia com pedículo súpero-medial e implante mamário. Rev Bras Cir Plást. 2012;27(4):576-583. DOI: https://doi.org/10.1590/S1983-51752012000400018
14. Spear SL, Baker Júnior JL. Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg. 1995 Oct;96(5):1119-23;discussion:1124. DOI: https://doi.org/10.1097/00006534-199510000-00018
15. Meiega JM, Amaral AB, Cunha KN. Arantes HL, Kawasak MC. A Capsulectomia sem Capsulotomia no Tratamento das Contraturas Capsulares. Rev Bras Cir Plást. 2001;16(2):37-48.
16. Handel N. Secondary mastopexy in the augmented patient: a recipe for disaster. Plast Reconstr Surg. 2006 Dec;118(7 Suppl):152S-163S;discussion:164S-167S. DOI: https://doi.org/10.1097/01.prs.a0000246106.85435.74
17. Young VL. Guidelines and indications for breast implant capsulectomy. Plast Reconstr Surg. 1998 Sep;102(3):884-91;discussion:892-4. DOI: https://doi.org/10.1097/00006534-199809010-00043
18. Saraiva JAC. Tratamento das contraturas nas mamoplastias de aumento retroglandulares: implante retropeitoral com retalho capsular. Rev Bras Cir Plást. 2013 Jul/Sep;28(4):607-610.
19. Tebbetts JB. “Out points” criteria for breast implant removal without replacement and criteria to minimize reoperations following breast augmentation. Plast Reconstr Surg. 2004 Oct;114(5):1258-62. PMID: 15457046 DOI: https://doi.org/10.1097/01.PRS.0000136802.91357.CF
20. Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to “dual-plane” positioning: technique and outcomes. Plast Reconstr Surg. 2003;112(2):456-66. PMID: 12900603 DOI: https://doi.org/10.1097/01.PRS.0000070987.15303.1A
21. Virden CP, Dobke MK, Stein P, Parsons CL, Frank DH. Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg. 1992;16(2):173-9. PMID: 1570781 DOI: https://doi.org/10.1007/BF00450610
22. Tamboto H, Vickery K, Deva AK. Subclinical (biofilm) infection causes capsular contracture in a porcine model following augmentation mammaplasty. Plast Reconstr Surg. 2010 Sep;126(3):835-42. DOI: https://doi.org/10.1097/PRS.0b013e3181e3b456
23. Spear SL. Capsulotomy, capsulectomy, and implantectomy. Plast Reconstr Surg. 1993;92(2):323-4. PMID: 8337283 DOI: https://doi.org/10.1097/00006534-199308000-00018
24. Peters W, Smith D, Fornasier V, Lugowski S, Ibanez D. An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann Plast Surg. 1997 Jul;39(1):9-19. PMID: 9229086 DOI: https://doi.org/10.1097/00000637-199707000-00002
25. Dinah W, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. 2016 Mar;137(3):826-41. DOI: https://doi.org/10.1097/01.prs.0000480095.23356.ae
26. Mahler D, Hauben DJ. Retromammary versus retropectoral breast augmentation: a comparative study. Ann Plast Surg. 1982 May;8(5):370-4. DOI: https://doi.org/10.1097/00000637-198205000-00003
1. Centro de Cirurgia Plástica e Bem Estar, Pato Branco, PR, Brazil.
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil.
Corresponding author: Vinicius Julio Camargo Rua Tapir 757, Centro, Pato Branco, PR, Brazil. Zip Code: 85501-032. E-mail: viniciusjcamargo@yahoo.com.br
Article received: January 12, 2019.
Article accepted: July 08, 2019.
Conflicts of interest: none.



















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter