

Articles - Year 2002 - Volume 17 -
Incidence of Hematoma and Seroma in Abdominoplasty with and without the Use of Drains
Incidência de Hematoma e Seroma em Abdominoplastia com e sem uso de Drenos
ABSTRACT
Based on the experience with 69 patients submitted to abdominoplasty, the authors compare the use of capillary tubes, suction drains and not using drains in the postoperative period as to the effictiveness in preventing hematomas and seromas under the abdominal flap. They also study the association of these fluid collections with known risk factors. They describe the indications and surgical technique employed in their cases and compare results obtained with data available in literature.
Keywords: Abdominoplasty; dermolipectomy; hematoma; seroma; drains
RESUMO
Os autores, baseados na experiência de 69 pacientes submetidos a abdominoplastia, comparam a utilização de dreno de capilaridade, de sucção e a não utilização de drenos no pós-operatório quanto à eficácia na prevenção da formação de hematomas e seromas sob o retalho abdominal, bem como estudam a associação dessas coleções com fatores de risco conhecidos. Descrevem as indicações e técnica cirúrgica empregadas em sua casuística e comparam seus resultados com dados presentes na literatura.
Palavras-chave: Abdominoplastia; dermolipectomia; hematoma; seroma; drenos
Until the end of the 19th century, abdominal wall surgery limited itself to small resections and corrections of abdominal hernias. In these cases, abdominal dermolipectomy facilitated herniorraphy, but it also provided the patient with the resection of any excess fat(1,2,3). With the enhancement of this technique, abdominal plastic surgelry developed to the current stage, with a low transversal incision, detachment of the flap to the lower level of the rib cage, muscular plicature, repositioning of the umbilical scar and resection of any excess cutaneous tissue.
Hematoma and seroma comprise the most frequent complications of abdominoplasty. Such fluid collections are diagnosed by a physical exam or ultrasound(4,5), and most surgeons, according to the literature, recommend the use of drains in the immediate postoperative period (PO), because the presence of fluids can compromise scar healing, since they delay healing and may lead to infections(6,7).
With this study, we intended to verify the effectiveness of drains in preveming hematoma and seroma, as well as to relate the incidence of these fluid collections with risk factors: systemic arterial hypertension (HAS), use of non-steroid anti-inflammatory drugs (NSAID) and smoking.
PATIENTS AND METHODS
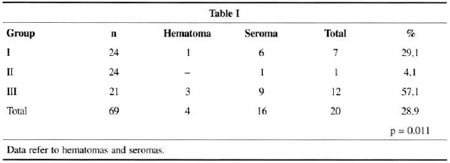
This study was based on the evaluation of patients submitted to abdominoplasty in the Plastic Surgery Service of São Lucas Hospital / PUCRS from January 1999 to November 2000. By means of a randomized prospective study, we evaluated a total of 69 patients divided imo three groups: group I (n=24) - in which we used a latex drain (penrose®); group II (n = 24) - in which we used a rigid suction drain tube (Portovac® or similar); and group III (n=21) - in which we did not use any drains.
All patients were female, with ages varying from 19 to 67 years old (average of 35.6 years old) , with clinical indication for abdominal dermolipectomy, associated or not to diastases of rectus abdominis muscles.We applied the Chi-square test to correlate the incidence of collections, the body mass index (BMI), the mentioned risk factors and the resected flap weight.
The surgery, with the patient in supine position under general or epidural anesthesia, starts with a low transversal abdominal incision made over a previous marking at the suprapubic level, extended to the level of the antero-superior iliac crest, followed by a thorough detachment at the supra-aponeurotic level up to the subcostal and subxiphoid region, with de-insertion of the umbilical scar of the dislocated flap. After rigorous hemostasis, we perform a plicature of rectus abdominis muscles (if diastasis is present). Then, we reposition and fix the umbilical scar and resect any excess skin fat.We fix the flap on the suprapubic region, and the incision is sutured with simple inverted mononylon 3.0 and 4.0 sutures on the subdermic plan, and intradermic suture with mononylon 3.0 or monocryl 3.0 on the dermic plan. We use a dry occlusive dressing with gauze and micropore over the incision and umbilical scar. In the case of a latex drain tube, we use two penrose® nº 1 tubes, placed through orifices made at the pubic hair region, extending over the abdominal flap up to the umbilical region, and remaining in place for 24 hours. In the case of a suction drain, we use a Portovac® or similar tube with 1/4 to 1/8 diameter, placed through an orifice made at the pubic hair region, extending over the flap up to the umbilical region.
The suction drain remains for at least five days or drainage under 30ml/day, connected to a suction mechanism (Folley catheter, syringe or serum flask), and drained whenever necessary, until the drain is removed in the patient's first outpatient review visit (7th PO in average). All patients wear a compressive abdominal elastic waistband, for at least 30 days, and are recommended to avoid abdominal effort.
In the postoperative period, we used antibiotics (ATB) -cefalotine 1g EV 6/6h for 24 hours and oral cefalexine 500mg 6/6h or cefadroxil 500mg 12/12h for five days. During the outpatient follow-up, we analyzed the incidence of hematoma and/or seroma under the abdominal flap by wall palpation. If present, collections were drained with sterilized material under aseptic conditions, and the volume collected measured. If new collections were present in subsequent reviews, they were always drained and measured.
RESULTS
In table I, group I (capillary tube) there were 7 cases of collection (29.1%); in group 2 (suction drain) we had only one case of collection (4.1%); in grou p 3 (without a drain) there were 12 collections (57.1%). Seroma was the most freguem collection (23.2%). We applied a Chi-sguare test with statistical significance (p= 0.011) to verify associations among the 3 groups and the incidence of collections. Average patient follow-up was 12 weeks.
Some of the complications encompassed a case of operative wound infection (group I), a late seroma (group I) and one case of tube obstruction (group II), which was removed on the 3rd PO day. This patient presented clinical evidence of fluid collection under the abdominal flap on the 7th PO day (1st outpatient review), and needed drainage. All patients with collections diagnosed in outpatient reviews were treated with drainage. There was no statistical significant relation between the aforementioned risk factors and the incidence of collections or with other variables researched. None of the patients referred discomfort.
DISCUSSION
In the literature, most authors recommend drainage in postoperative abdominoplasty to prevent the occurrence of subcutaneous fluid collections. Shestak(8) presented 4% of seroma incidence using suction drains, similar to our cases. Other authors, like Mohammad et als.(4), had a high incidence of collection (42% seroma and 9% hematoma), in spite of suction drains. We believe this is due to early removal of drains from all patients, around the 2nd PO. Some professionals in our area use the drain tube in the PO period for up to 10 days or more. We believe this is excessive time, which can even increase the risk of infection and cause patient discomfort. We believe a period of five days or drainage inferior to 30ml/24h is pertinent criteria for the decision to remove the suction drain. Others, such as Matarasso(9) and Muhlbauer(10), had collection rates similar to ours. Grazer(7) presented a large incidence of collections (67%) using capillary tubes. In our cases, the highest incidences occurred without the use of drain tubes and with the use of capillary tubes. In our study, the suction drain proved to be more effective in preventing collections: despite long drain tube permanence time during the home phase, all patients could stand it well, with little discomfort and absence of pain (data calculated through the Hutchinson scale) due to the suitable information received. Likewise, we had no increase in infection rates because of long drain tube use.
CONCLUSION
We conclude with this study that there is no isolated causal factor for subcutaneous fluid collections in PO abdominoplasty. We believe that in large detachments, insufficient hemostasis, abusive use of eletrocautery, as well as early patient activity and unsuitable abdominal compression are important predisposing factors to these collections.
We believe suction drains prevent hematomas and seromas effectively through prolonged active drainage, and do not result in more complication rates thanwhen not utilizing drains or utilizing capillary tubes.
REFERENCES
1. Ely JF. Cirurgia Plástica, 32. p. 600-11.
2. Grazer FM. Abdominoplasty. In: May JR, Littler JW, editors. Plastic Surgery Philadelphia : WB Saunders; 1990. Vol. 6, p. 3929-63.
3. Pitman GH. Liposuction and body contouring. In: Aston SI, Beasley RW,Thorne CHM, editors. Grabb and Smith's Plastic Surgery: 5. ed. Philadelphia : Lippincott-Raven; 1997. p. 669-92.
4. Mohammad JA, et al. Ultrasound in the diagnosis and management of fluid collection complications following abdominoplasty. Ann Plast Surg. 1998;41 (5)498-502.
5. Stocchero IN. Ultrasound and seromas [letter]. Plast Reconstr Surg. 1993;91(1):198.
6. Hay-Roe V. Seroma after lipoplasty with abdominoplasty. Plast Reconstr Surg. 1991;87(5) :997-8.
7. Grazer FM, Goldwyn RM. Abdominoplasty assessed by surve, with emphasis on complications.Plast Reconstr Surg. 1977;59(4):513-7.
8. Shestak KC. Marriage abdominoplasty expands the mini-abdominoplasty concept. Plast Reconstr Surg. 1999;103(3):1020-31.
9. Matarasso A, Matarasso SL. When does your liposuction patient require an abdominoplasty? Dermatol Surg. 1997;23(12):1151-60.
10. Muhlbauer W. Radical abdominoplasty including body shaping representative cases. Aesth Plast Surg.1989;13(2): 105-10.
I - Resident Physician of the Plastic Surgery Service of São Lucas Hospital - PUCRS.
II - Resident Physician of the General Surgery Service of Nossa Sra. de Pompéia Hospital.
III - Preceptor of the Plastic Surgery Service of PUCRS Medical School.
IV - Professor, Surgery Department of PUCRS Medical School. Preceptor of the Plastic Surgery Service of HSL/PUCRS.
V - Full Professor of Plastic Surgery of FAMED/PUCRS. Head ofthe Plastic Surgery Service of HSL/PUCRS. Plastic Surgery Service of São Lucas Hospital / PUCRS.
Address for correspondence:
Márcio Vinicius Nurkim, MD
Av.Ipiranga, 6690 90610-000
Porto Alegre - RS Brazil
Phone: (55 51) 320-3000 r. 2359


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter