

Articles - Year 2002 - Volume 17 -
Temporomandibular Joint (TMJ) Dysfunction
Disfunção da Articulação Temporomandibular (ATM)
ABSTRACT
The authors report the treatment of TMJ dysfunction in 656 consecutive patients, using simple relative TMJ rest, with immediate cures in more than 80% of the patients. The anatomophysiology of the TMJ and mainly the pain mechanism are discussed. The authors studied the occurrence of TMJ dysfunction without pain in the population and observed that treatment is not necessary in 35% ofthe cases. More severe cases require surgery (4%). The major steps of surgical treatment and final results are described.
Keywords: Temporomandibular dysfunction; myofacial pain; temporomandibular pain; temporomandibular joint syndrome; myogenic craniomandibular dysfunction; Costen syndrome; painful temporomandibular joint syndrome
RESUMO
Os autores reportam o tratamento da disfunção da ATM em 656 pacientes consecutivos, com o simples repouso relativo das ATMs, em que obtiveram mais de 80% de cura imediata. Discorrem sobre a anatomofisiologia da ATM e principalmente sobre o mecanismo da dor.
Pesquisam na população quanto à ocorrência da disfunção da ATM, sem sintomatologia dolorosa, e apuram 35% de incidência que não necessitam qualquer tratamento. Os casos mais graves têm indicação cirúrgica (4%). Descrevem as etapas principais do tratamento cirúrgico e resultados finais.
Palavras-chave: Disfunção temporomandibular; dor miofacial; dor têmporo-mandibular; síndrome da articulação temporomandibular; disfunção craniomandibular miogênica; síndrome de Costen; síndrome dolorosa da articulação temporomandibular
Pain, crepitation, temporomandibular joint (TMJ) blockage, diffused pain to the face and ear, in a greater or lesser degree affect a large population, varying from 3% to 20%(1,2,3), although only a minority seeks first a dentist and afterwards (and now increasingly more often) a bucomaxillofacial surgeon for treatment and relief. Limited knowledge of the physiopathology of TMJ makes it difficult to prescribe subsequent treatment for these patients.
In the last 5 years, 656 patients with TMJ pain were seen. All cases were treated with the same basic orientation and most cases were followed up clinically. In the mean time, a survey was conducted to identify the incidence of any TMJ dysfunction in the general population that did not cause patients to go to a specialist. Results are shown in the present study.
DEFINITION
Dysfunction is the partial ar total abnormal derangement of a functioning organ. A syndrome is a set of signs and symptoms that freguently occur together in the same condition. Dysfunctions of the joint and of musdes related to the joint should not be grouped together(4), although it is impossible to separate them. Therefore, a TMJ dysfunction is any alteration of normal movement, with or without pain.
The most frequent signs and symptoms are: localized or diffused facial pain, earache, pain upon joint movement, crepitation, blockage and dislocation. Only patients with pain seek a specialist for treatment. Although this accounts for only a minority, the incidence rate in the general population is high.
Monson was the first to point out the condition in 1920 and 1921,(5,6) although Costen was responsible for its dissemination in 1934(7). He associated earache to compression of the Eustachian tube caused by a deep overbite due to missing molars, which makes the condyle compress the auriculo temporalis nerve that runs through the retroarticular fossa. Later anatomic and clinical studies revealed aspects that differed from what Costen believed (8).
TMJ FUNCTIONAL ANATOMY
TMJ is part of a highly specialized functional unit. It is part of the masticatory system, along with the teeth and their structure, the mandible and its musdes, and, to a lesser degree, swallowing and phonation, that takes part in TMJ movement.
The mandibular condyle (condyloid process) is a semicylindrical structure, 15 to 20 mm long and 8 - 10 mm wide. Its largest axis forms a straight angle with the mandibular angle.
The articular fossa opposite the condyle (glenoid cavity) is situated on the temporal squama, anterior to the tympanic bone, and is called the articular eminence or tubercle in its most anterior portion. Similar to the capitulum mandibulae, its lining is also fibrous. An oval, fibrous, avascular, highly pressure-resistant disc is found between the two articular surfaces. It is thin in the center and thickens towards the edge to adjust both convex structures, from the condyle to the articular eminence. The disc is 1 mm thick in its central portion, highly resistant to pressure and slides easily, dividing the TMJ into 2 compartments: a higher wide, sliding compartment and a much smaller, lower one that barely covers the capitulum of the condyloid process.
All of the above elements are covered by a fibrous capsule that is strong on the outside and delicate on the inside, and sufficiently loose to allow ample joint movement (Figs. 1 and 2).

Fig. 1 - Drawing representing TMJ. Note the external pterygoid muscle with its 2 heads: one to pull the disc and another for the condyle.

Fig. 2 - During the glicling movement (anteroposterior), and open mouth, the disc passes between the condyle and articular eminence. In a dislocated-reduced joint, the disc is traumatized and may cause pain.
TMJ INNERVATION
At the retromandibular fossa or space, the auriculotemporal nerve is responsible for joint sensitivity. Other branches deviate to innerve the tympanum and the anterior wall of the external ear canal. Continuous and intense stimulus of a nerve through signals at the central nudeus, together with the neurons intimately related to the stimulated nerve produce reflex pain. This is a central phenomenon with a peripherally originated stimulus. As an example, the intense pain of a mandible tooth (lower dental nerve zone) may lead to trigeminalgia. This explains pain in the trigeminal region originated at the TMJ from the neurological point of view and may make it difficult to make a correct diagnosis(9).
There is a marked difference between free movements and chewing movements. In the former, the muscles are relaxed, while during chewing the power of musde contraction gives TMJ a different dynamics. There are 3 basic movements:
1. Rotating, around the condyle axis, in the anteroposteriar direction, as in a hinge.
2. Gliding, with the condyle head and disc sliding over the glenoid cavity of the temporal squama.
3. Torsion, when the movement of both structures becomes asymmetric, with a lateral deviation.
The combination of these movements gives the mandible a wide and varied range of movement.
CREPITATION MECHANISM
The click of the joint heard by the patient, and sometimes by the exarniner, is not a very well understood articular crepitation. It comes and goes spontaneously in 50% of the population(10). It occurs due to a lack of coordination between the condyle and the disc during the gliding movement, in which alignment is lost for a moment.
In more severe cases of TMJ blockage, the articular disc can dislocate to the frant or fold in onto itself, as arthragraphies performed with computerized radiographs (11) have shown.
The click of the joint without blockage or pain is clinically insignificant, as it does not lead to a dysfunction, which would justify more aggressive treatment. It is as frequent as with the movements of the cervical spine.
BLOCKAGE
TMJ blockage is a phenomenon of the interarticular disc which, for some reason, does not allow the condyle to perform the gliding movement (posteroanterior) smoothly. Clinically, the blockage is the partial or total interruption of the mandibular movement. Since the mandible is a rigid arch, TMJ blockage on one side deviatesthe chin to the homologous side, creating a ratation movement. During total blockage, the mouth opens to the limit of the blockage.
BRUXISM
During the sleep of an unconscious patient, all body musdes are relaxed, induding musdes used in mastication. Teeth grinding during sleep means that muscular stimuli are coming fram the subconscious.
When the patient is not told by an observer, worn incisors and TMJ pain in the morning can facilitate the diagnosis. Bruxism is almost always accompanied by a large amount of tension, which worsens the picture. Not all individuals with bruxism experience pain.
DISLOCATION - SPONTANEOUS REDUCTION
The interarticular disc places itself between the condyle and the articular eminence upon maximum opening of the mouth (Fig. 2). When the limit is surpassed, the condyle dislocates and the patient's mouth stays open and cannot dose, which calls for manual reduction or surgery. In 35% of the normal general population, however, dislocation is followed by unperceived spontaneous reduction. Depending on how loose the capsule is and how large or small the prominence of the articular eminence, the disc may or may not be traumatized during the movement, resulting in pain.
CAUSES OF PAIN
Didactically, there are many possible causes of TMJ pain, but they are always associated with some local factor of the joint itself:
1. In protrusive occlusion, the mandible compresses the articular process and the anterior border of the disc.
2. In reverse occlusion, the mandible compresses the posterior border of the disc and the retromandibular space through which ali nerves pass.
3. In deep overbite with worn tooth surfaces, the condyle compresses the highest part of the joint. The phenomenon would also occur during strong and continuous chewing. A deep overbite is when the upper incisors overlap the lower incisors by more than 50%.
4. In a forced mouth opening, the condyle is projected, compressing the disc against the articular eminence, and distending the capsule and ligaments. This frequently occurs after the extraction of a molar or wisdom tooth. Continuous or intermittent trauma leads to edema of regional tissue with consequences to the auriculotemporal nerve, producing referred pain in the innervated regions (ear, ear canal, tympanum, face) (Fig.2).
5. Possibly in synovitis with edema and production of synovial liquid distending the articular capsule and leading to spontaneous pain upon movement.
6. The muscle tonus involved in moving the TMJ is greatly influenced by emotional tension. In 75% of cases(12), TMJ dysfunction sufferers are known to undergo a great amount of tension. Muscle contractions due to stress, fear, anger, etc., in addition to bruxism or clenching of the teeth, are prevailing factors that trigger pain.
7. Aside from traumatic causes, the TMJ suffers the same effects of rheumatic arthrosis phenomena, as do other joints.
DIAGNOSIS OF THE DYSFUNCTION
The presence of pain in the TMJ region upon rest or movement is the most common sign. Earache may be the first symptom. Sometimes diffuse facial pain without a precise location, at times in the temporal region, at times in the parotid, or in the teeth, confuses the patient and leads him/her to go to many different specialists without obtaining relief (reflex pain and referred pain). A background of poor relationship at home or at work, apprehension, fear, are almost always present. When the individual has a closed mouth and a resting maxilla, teeth do not touch, and the simple perception that teeth are actually touching means some form of existing tension.
Pain may be spontaneous and go unnoticed, or it may occur during sleep while pressing one's face on the pillow at the side where the pain is, or after intense food chewing. The click may or may not be present. The inability to fully open the mouth may be caused by the pain itself, or by TMJ blockage, possibly due to the interarticular disc condition, either because of perforation, callosity or an incorrect gliding movement due to spasm of the external pterygoid muscle.
Upon examination, there is pain when the joint and/ or subjacent areas are pressed digitally. Whenever present, crepitation can be felt when the mouth is opened. Deviation of the mouth to one side means partial or total blockage on the same side, which is not always the side where the pain is located. The blockage forces the opposite joint to greater gliding and torsion (on its own axis) leading to symptoms. Therefore, the affected joint is not always the painful one. Excessive mobility of TMJs has not been the main cause of pain, as 34% of normal individuals have this condition.
The absence of molars or the presence of a prosthesis or malocclusion may be present but may not be the cause of the condition. Worn teeth, mainly incisors indicate the patient is tense and grinds his/her teeth. The diagnosis is eminently clinical. Radiographs are unrevealing. Normal TMJ radiological variations are so diversified that they are of little or no help at all in the diagnosis(13).
Dynamic Magnetic Resonance (MR) is very valuable for diagnosis because it allows the movement of the disc and the condyle, and the relationship between them to be observed. An MR should not be performed in the acute phase because it would certainly show some impairment. Blood tests would only play a diagnostic role in rheumatism.
CLASSIFICATION OF DYSFUNCTIONS
Many causes of TMJ dysfunction lead to pain. We can divide them into 2 large groups: intrinsic dysfunctions, directly involved with the joint and its capsule; and extrinsic dysfunctions that work at a distance and are extracapsular, such as an emotional state and muscle dystonias. As in anything, the more the professional knows about the pathophysiology of the masticatory system and its peculiarities, the easier it is to recognize and point to the appropriate treatment path(14).
TMJ dysfunctions can be divided into categories:
1. INTRINSIC FACTORS
a) Articular disc disorder
b) Capsulitis and Synovitis
c) Arthritis
d) Arthrosis
e) Capsular fibrosis
f) Bone ankylosis
g) Development defects
h) Tumors
2. EXTRINSIC FACTORS
a) Muscle disorders
b) Fibrosis and extracapsular ankylosis
c) Tumors
TREATMENT
ACUTE PHASE
The immediate treatment of acute pain is fundamentally conservative, and should always be considered and practiced before any other more aggressive measure, regardless of etiology. Conservative treatment consists of resting the joint without immobilizing it.
Small excursion mouth opening and closing movements help the disc to return to its anatomical site. The cause that triggers pain leads to edema of the disc and articular capsule. The disc is irrigated by osmosis and the edema only resolves in 2 to 3 weeks. These small excursion movements therefore should continue for 1 month. Limiting mouth opening should be respected even during yawning. Soft diet (non-sticky foods), with foods that do not require any effort during shredding should equally be offered during the same period.
Muscle contraction of external pterygoid muscles should be encouraged and painkillers along with muscle relaxants should be prescribed for pain. Tension and stress are almost always present, therefore, the patient should be told to relax the mandible when he/she feels teeth are touching when the mouth is closed.
A convincing and simple explanation of how the joint works allows the patient to understand and collaborate in treatment more actively.
TREATMENT OF BRUXISM
The cause of bruxism lies in the subconscious. In this specific case, two attitudes should be added to the treatment described. The first is to seek help from psychology to try to better understand the cause, and the other is to use an acrylic or silicone mouth guard at night to prevent the contraction of powerful chewing muscles that leads to teeth grinding; and to keep the space between the teeth and not compress the interarticular disc against the glenoid cavity. A mouth guard does not cure bruxism; it only protects the TMJ until the underlying cause is can be found.
SURGICAL TREATMENT
A small percentage of patients with TMJ dysfunction are candidates for surgical treatment. In most cases, the problem is in the interarticular disc which, for some reason, is dislocated in relation to its normal position, leading to deficient and painful dynamics. Surgical removal of the interarticular disc is indicated.
In arthroplasty as in surgery of the parotid, the major concern is not to injure the branches of the facial nerve. The temporal branch of the nerve crosses the region and great care must be taken as not to damage it. A nerve stimulator is used during the surgical procedure to identify the nerve (Figs. 3 and 4). The anesthetist must not use any fast-metabolizing muscle relaxants or paralyzing drugs. Access is through a pre-auricular incision passing through the tragus. The dermofat flap is dislocated to the region of the joint. The parotid gland is crossed with care in order to preserve the frontal branch of the facial nerve. A 1: 100,000 adrenaline solution decreases bleeding, avoiding eletrocauterization, which is harmful to the facial nerve, and improves the field of vision. The articular capsule is open under the zygomatic arch, inunediately exposing the interarticular disc that presents itself better when the chin is forced towards the contralateral side, separating the condyle from the glenoid cavity. Local examination reveals the disc dislocated from its normal position, or to the front or to the side. When it is removed, surface irregularities, callosity or perforations that cause dysfunction can be seen. The disc is removed with delicate, curved or angular scissors. The procedure begins at the anterior and less irrigated portion, following its contour until it is completely removed.

Fig. 3 - Incision (bold dotted line) similar to rhytidoplasty. The frontal branch of the facial nerve on the parotid gland surface crosses the site of access to the joint.

Fig. 4 - Bipolar nerve stimulator with a continuous charge of 0 to 10 mA for identifying facial nerve branches.
Sometimes there is profuse bleeding due to injury to the mesial vessels, making cauterization difficult. Packing with wet gauze and light pressure on the site, forcing the chin to the same side and waiting for 5 minutes, normally leads to hemostasis. We see no need to suture either the capsule or the deep planes. We leave a Penrose drain and remove it after 24 hours.
During the immediate post-operative period the patient remains in the Fawler position, with ice on the operated side and painkillers. The patient is free to decide on how much to move his/her mouth.
CASES
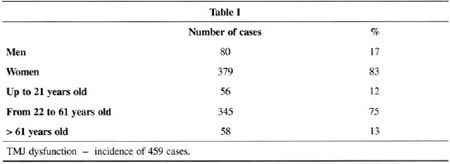
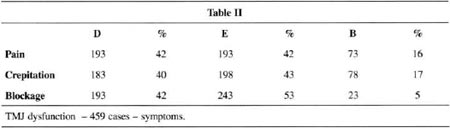
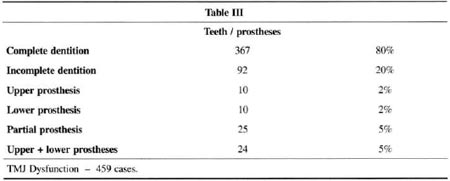
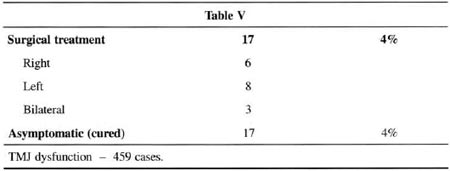
Six hundred and fifty-six patients with TMJ dysfunction and localized and diffuse facial pain were treated from August 1996 to August 2000. Ofthose, we followed up on 459. Remission of acute symptoms occurred in 84% after the first treatment attempt, by resting the joint for 30 days. Finally,the pain remission rate reached more than 90% on the second attempt. Only 5% did not improve with treatment.
At the same time, a survey with 100 consecutive cases of individuals without any TMJ pain symptoms was conducted. In 35% of these "normal" subjects no TMJ dysfunction was observed, corroborating the work of Costa(15)(see charts I to V).

COMMENTS
TMJ acute or chronic treatment is fundamentally clinical(16,17,18).Surgical treatment should be left for a specific minority with joint impairment not treatable by conservative methods(19).
Initial phase diagnosis is simple, even if the presentation is atypical. Onset of pain, recurrences, painful exacerbations due to major or minor trauma and muscular pain almost always coincide with an episode of tension (pre-menstrual, emotional conflict, stress at work). The psychic threshold of irritability varies from one individual to another and, therefore, the response to pain also varies. Undoubtedly there is an appropriate anatomic site that justifies the pain, although the latter is almost always associated with a heavy dose of psychic tension. Stress alone, regardless of intensity, does not lead to joint pain if there is no anatomical dysfunction or muscular spasm. Sometimes, slight dysfunction and great tension trigger pain. The fact is that in 85% of the cases some form of tension is present, and even more frequently in women. It does not seem plausible, however, that the fact that women are affected by dysfunctions or more marked anatomical differences than men justifies the higher number of women affected (83%).
Total or partial lack of teeth, dental malocclusion and a deep overbite are not major factors, although we do not have statistical data regarding the presence of malocclusion in the general population and its relation to TMJ dysfunction. Knowing that any form of TMJ dysfunction without pain is quite common, varying between 20 and 50% of the general population (3,20), relatively few individuals develop pain. If there is no pain, treatment is justified only in more severe cases of TMJ blockage with difficult mouth opening and recurring dislocations. Treatment differs from the condition under discussion. Conservative treatment with relative TMJ rest, associated with muscle analgesics and antidystonics or sedatives, have been sufficient to cure the acute phase in more than 90% of patients. A thorough, simple explanation to the patient in lay language about how the joint works and the possible causes of pain has been very valuable in securing the patient's trust, assuring cooperation during treatment and, at times, even avoiding the use of sedatives.
Surgical treatment is indicated for 5% of cases that cannot be solved clinically. Surgery for bruxism should be avoided unless psychological treatment has had some effect but the dysfunction persists. Handling facial innervation with care (mainly the frontal branch) is important. Neuropraxia (or trauma by nerve distension) is common, and paralysis of the homologous eyebrow disappears in up to 6 months. Stimulators have been very valuable in identifying and preserving the nerve.
It is absolutely mandatory that anesthetists do not use any muscular relaxants, including fast metabolizing relaxants. Mouth movement is allowed and even stimulated. The scar contraction phase also works on the TMJ, and opening and closing mouth exercises should be stimulated during this period.
CONCLUSIONS
1. TMJ dysfunction affects 35% of the general population, although only a small percentage of the group has pain symptoms.
2. The incidence is 4 times higher in females.
3. An emotional factor triggers pain in 85% of cases.
4. Treatment during the painful phase is relative rest of the joint and medication for symptoms which relieve pain in 90% of patients treated.
5. The few surgical cases are limited to severe intraarticular blockage, recurring dislocations, to symptomatic mandibular dysmorphism.
6. Intermaxilar blockage treatment is not very helpful in relieving pain during the acute phase.
7. Special attention should be given to treating bruxism.
REFERENCES
1. Agerber G, Carlson GE. Symptoms of functional disturbances of the mastigatory system. A comparison of freguencies in a population sampleand in a group of patients. Acta Odnt Scandinav. 1975;33:183-91.
2. Helkimo M. Epidemiological surveys of disfunction of the mastigaroy system. Oral Science Rev. 1976;7:54-60.
3. Locker D, Slade G. Prevalence of symptoms associated with temporomandibular disorders in a Canadian population. Community Dent Oral Epidemiol. 1988;16(5):310-3.
4. Laskin DH. Etiology of the pain-dysfunction syndrome.J Am Ass. 1969;79:147-52.
5. Monson G. Occlusion supplied to crow and bridgework. Nat Dent A J. 1920;7:399-405.
6. Monson G. Impaired function as a resulted of closed bite. Nat Dent A J. 1921;8:33-838.
7. Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Rolog Larynggol.1934;43:1-7.
8. Sicher H. Temporomandibular articulation in mandibular overclosure. J Am Dent Ass. 1948;36: 131-6.
9. Travell J, Rinzler SH. The myofacial genesis of pain. Postgrad Med. 1952;11:425-9.
10. Ramfjord S, Ash MA. Occlusion. 3. ed. Philadelphia: WB Saunders; 1983. p. 249.
11. Isacsson G, Linde C, Isberg A. Subjective symptoms in pacients with temporomandibular joint disk displacement versus patients with myogenic craneomandibular disorders. J Prost Dent. 1989;61:70-8.
12. THOMPSON H. Mandibular dysfunction syndrome. Brit Dent J. 1971;130:187-93.
13. Bezuur JN, Habets LL, Hanson TL. The recognition of craneomandibular disorders. J Oral Rehabil, 1988;6:549.
14. Miranda ME. Disfunções craniomandibulares. Perspectivas e tratamento. Review em ATM e oclusão. São Paulo: Quintessence; 1988. p. 149- 54.
15. Costa EA, Pitanguy I, Cruz RL, Ceravolo ML. Síndrome articular temporomandibular. Rev Bras Cir.1981;71:195-202.
16. Gerke DC, Richards LC, Gross AN. Discriminants function analysis of clinical and psychological variables in temporomandibular joint disfunction. Aust Dent J. 1989;34:44-52.
17. Okeson JP, Hayes DK. Long-term results of treatament for temporomandibular disorders: an evaluation by patients. J Am Dent Ass. 1986;12:473-9.
18. Wedell A, Carlsson GE. A four years follow up, by means of questionaire of patients with functional disturbances of the mastigatory system. J Oral Rehabil. 1986;13:105-13.
19. Wilkers CH. Internal Derangements of the temporomandibular joints. pathological variations. Arch Otolaryn Head Neck Surg. 1989;115:469- 75.
20. Wanrnan A, Agerberg G. Relationship between signs and symptoms of mandibular dysfunction in adolescents. Com Dent Oral Epidem. 1986;14:225-31.
I - Member of the Brazilian Society of Plastic Surgery.
II - Member ofthe Brazilian Sociery of Plastic Surgery and of the American Society of Maxillofacial Surgery.
Address for correspondence:
José Badim,MD
R. São Francisco Xavier, 390
20550-013 - Rio de Janeiro - RJ Brazil
Phone: (5521) 3978-6000
e-mail: jbadim@uol.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter