

Review Article - Year 2019 - Volume 34 -
Injection of platelet aggregates in facial rejuvenation: a systematic review
Injeção de agregados plaquetários no rejuvenescimento facial: uma revisão sistemática
ABSTRACT
Introduction: This systematic review was conducted to assess whether the use of a platelet aggregate injection with or without associated facial rejuvenation techniques favors facial rejuvenation in adult patients.
Methods: Randomized clinical trials that compared the use of techniques for facial rejuvenation alone with the same techniques coupled with the injection of platelet aggregates were searched. The search was performed in indexed databases and in the gray literature. The Cochrane Collaboration bias risk tool was applied to assess the quality of the studies.
Results: In total, 7137 articles were identified. Only four studies remained in the qualitative synthesis, and the others were considered as having undefined bias risk in the key domains.
Conclusion: There are few studies in the literature that compare the use of platelet aggregates in facial rejuvenation and those that are available have a risk of "undefined" or "high" bias. There is a need for more well-designed clinical studies comparing the use of platelet aggregate injection with or without associated facial rejuvenation techniques.
Keywords: Skin; Rejuvenation; Platelet-rich plasma; Platelets; Fibrin; Review
RESUMO
Introdução: Essa revisão sistemática foi conduzida para avaliar se a associação da
aplicação da injeção de agregados plaquetários quando comparada a outras
terapias faciais favorece no rejuvenescimento facial em pacientes
adultos.
Métodos: A pesquisa buscou ensaios clínicos randomizados que compararam uso de
técnicas de rejuvenescimento facial isoladas com as mesmas técnicas aliadas
à injeção de agregados plaquetários. A busca foi realizada em bases de dados
indexadas e literatura cinzenta. A ferramenta de risco de viés da "Cochrane
Collaboration" foi aplicada para a avaliação da qualidade dos estudos.
Resultados: Foram identificados 7137 artigos. Apenas quatro estudos permaneceram na
síntese qualitativa, e os demais foram considerados com risco indefinido de
viés nos domínios chaves.
Conclusão: Existem poucos estudos na literatura que comparam o uso de agregados
plaquetários em rejuvenescimento facial e os que estão disponíveis têm risco
de viés "indefinido" ou "alto". Há necessidade de realizar mais estudos
clínicos bem delineados que comparem o uso de injeção de agregados
plaquetários associados ou não às técnicas de rejuvenescimento facial.
Palavras-chave: Pele; Rejuvenescimento; Plasma rico em plaquetas; Plaquetas; Fibrina; Revisão
INTRODUCTION
Currently, physical appearance is directly related to self-esteem, which also influences the acceptance of others1. A decrease of vascularization, the replacement of cells, fat atrophy, and loss of muscle tonus are some of the factors that trigger skin aging2. In addition, the combination of genetic factors (intrinsic aging) with environmental factors (photo aging) directly influences skin aging, a common biological process, which triggers clinical manifestations such as wrinkles, alteration of surface texture, and pigmentation, among others3. Thus, the treatment of facial rejuvenation is increasingly being exploited for a more effective and lasting achievement1.
Aesthetic facial rejuvenation can be divided into operational and non-operational procedures2. Operating procedures include facial liposculpture surgery, a procedure in which the tissues are carved with filling using intricate layers of infiltrated autologous tissue like fat for example4.
The prevention and treatment of skin aging are leveraging technological innovations in the cosmetic field; these innovations include mesotherapy and platelet-rich plasma (PRP), a potential tool for skin rejuvenation, capable of promoting the remodeling of the tissue as it is an autologous human platelet concentrate in a small volume of plasma, containing large reservoirs of bioactive proteins, including growth factors, which are able to facilitate collagen fibroblasts, increasing the proliferation of keratinocytes and the generation of hyaluronic acid, thus increasing, dermal elasticity1,3-5. In addition, a study proved that PRP in conjunction with aesthetic facial fat filling significantly reduced the post-treatment recovery time, thus favoring overall patient satisfaction6.
OBJECTIVE
There are many methods and techniques used in the treatment of facial rejuvenation, making it difficult to understand which facial therapies best favor this rejuvenation. We conducted a systematic review to compare the injection of platelet aggregates to other facial therapies in the facial rejuvenation of adult patients.
METHODS
Protocol and record
This study protocol was recorded in the PROSPERO database (CRD42017075650) and followed the recommendations of PRISM7, held from August to December 2017 at the Universidade Positivo in Curitiba, Paraná, Brazil.
The following controlled vocabulary search (MeSH terms) and keywords of the search strategy were established based on the acronym PICOS:
1. Population (P): Adult patients
2. Intervention (I): Injection of platelet aggregates Comparison (C): Other facial therapies
3. Primary outcome (O): Facial rejuvenation
4. Study design (S): Randomized clinical trials (RCTs)
The search included indexed electronic databases such as PubMed, Scopus, Web of Science, the Latin American Health Sciences Literature database (LILACS), the Brazilian Library of Dentistry (BBO), and the Cochrane Library (Chart 1).
| Pubmed= 714 (09/10/2017) | ||
| #1
((((((((((((Rejuvenation [MeSH Terms]) OR [MeSH Terms]) OR "Skin Aging" [MeSH Terms]) OR "Adults humans" [Title/Abstract]) OR "Adult human" [Title/Abstract]) OR Wrinkles [Title/Abstract]) OR ""Expression marks" "[Title/Abstract]) |
#2 (((((((((((((((((((((Plasma skin regeneration[MeSH Terms]) OR Platelet rich plasma[MeSH Terms]) OR Fibrin[MeSH Terms]) OR Platelet aggregation[MeSH Terms]) OR Blood platelets[MeSH Terms]) OR Injections[MeSH Terms]) OR Injection[MeSH Terms]) OR Growth factors[MeSH Terms]) OR "Plasma skin regeneration"[Title/Abstract]) OR "Platelet rich plasma"[Title/Abstract]) OR Fibrin[Title/Abstract]) OR "Platelet aggregation"[Title/Abstract]) OR "Blood platelets"[Title/Abstract]) OR Injections[Title/Abstract]) OR Injection[Title/Abstract]) OR "Growth factors"[Title/Abstract]) OR "Platelet rich fibrin"[Title/Abstract]) OR PRP[Title/Abstract]) OR PRF[Title/Abstract]) OR "Skin regeneration"[Title/Abstract]) OR "Platelet concentration"[Title/Abstract])) | #3 ((randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR ("clinical trial"[tw]) OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR (placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR comparative study[pt] OR evaluation studies as topic[mh] OR follow-up studies[mh] OR prospective studies[mh] OR control*[tw] OR prospective*[tw] OR volunteer*[tw]) NOT (animals[mh] NOT humans[mh]))) |
| #1 AND #2 AND #3 | ||
| Scopus= 5467 (09/10/17) | ||
| #1 ( ( TITLE-ABS-KEY ( rejuvenation ) OR TITLE-ABS-KEY ( "Skin Aging" ) OR TITLE-ABS-KEY ( "Adult human" ) OR TITLE-ABS-KEY ( wrinkles ) OR TITLE-ABS-KEY ( "Expression marks" ) ) ) | #2 ( ( TITLE-ABS-KEY ( "Plasma skin regeneration" ) OR TITLE-ABS-KEY ( "Platelet rich plasma" ) OR TITLE-ABS-KEY ( "Platelet aggregation" ) OR TITLE-ABS-KEY ( "Blood platelets" ) OR TITLE-ABS-KEY ( "Growth factors" ) OR TITLE-ABS-KEY ( injection ) OR TITLE-ABS-KEY ( rejuvenation ) OR TITLE-ABS-KEY ( "Platelet rich fibrin" ) OR TITLE-ABS-KEY ( prp ) OR TITLE-ABS-KEY ( prf ) OR TITLE-ABS-KEY ( "Skin regeneration" ) OR TITLE-ABS-KEY ( "Platelet concentration" ) ) ) AND ( LIMIT-TO ( SUBJAREA , "MEDI " ) OR LIMIT-TO ( SUBJAREA , "PHAR " ) OR LIMIT-TO ( SUBJAREA , "DENT " ) ) | |
| #1 AND #2 | ||
| Web of Science- 752 (09/10/2017) | ||
| #1 Topic:
(Rejuvenation) OR Topic: ("Skin Aging"") OR Topic: ("Adult human") OR Topic: (wrinkles) OR Topic: ("Expression marks) ) ) |
#2 Topic: ("Plasma skin regeneration") OR Topic: ("Platelet rich plasma") OR Topic: (Fibrin) OR Topic: ("Platelet aggregation") OR Topic: ("Blood platelets") OR Topic: (Injection*) OR Topic: ("Growth factORs") OR Topic: ("Platelet rich fibrin") OR Topic: ("Skin regeneration") OR Topic: ("Platelet concentration"). | |
| #1 AND #2 | ||
| Lilacs and BBO= 03 (03/00) - (09/10/17) | ||
| #1 (((MH:Rejuvenation OR MH:"Skin Aging" OR "Adults humans" OR "Adultos humanos" OR "Humanos Adultos" OR "Adult human" OR "Adulto humano" OR "Humano adulto" OR Wrinkles OR Arrugas OR Rugas OR "Expression marks" OR "Marcas de expression" OR "Marcas de expressão"))) | #2 (tw:((MH:"Plasma skin regeneration" OR MH:"Platelet rich plasma" OR MH:Fibrin OR MH:"Platelet aggregation" OR MH:"Blood platelets" OR MH:Injections OR MH:Injection OR MH:"Growth factors" OR "Platelet rich fibrin" OR "Plaquetas ricas em fibrina" OR "Plaquetas ricas en fibrin" OR PRP OR PRF OR "Skin regeneration" OR "Regeneração da pele" OR "Regeneración de la piel" OR "Platelet concentration" OR "Concentração plaquetaria" OR "Concentración plaquetaria"))) | |
| #1 AND #2 | ||
| Cochrane Library = 181 (09/10/2017) | ||
| #1 MeSH descriptor:
[Rejuvenation] explode all trees #2 MeSH descriptor: [Skin Aging] explode all trees #3 "Adults humans":ti,ab,kw or "Adult Human" or Wrinkles or "Expression Marks" (Word variations have been searched) #4 #1 or #2 or #3 |
#5 MeSH descriptor: [Plasma Skin
Regeneration] explode all trees #6 MeSH descriptor: [Platelet-Rich Plasma] explode all trees #7 MeSH descriptor: [Fibrin] explode all trees #8 MeSH descriptor: [Platelet Aggregation] explode all trees #9 MeSH descriptor: [Blood Platelets] explode all trees #10 MeSH descriptor: [Injections] explode all trees #11 "Growth factors":ti,ab,kw or "Platelet rich fibrin" or PRP or PRF or "Skin regeneration" (Word variations have been searched) #12 "Platelet concentration":ti,ab,kw (Word variations have been searched) #13 #5 or #6 or #7 or #8 or #9 or #10 or #11 |
|
| #4 AND #13 | ||
In addition, a search was made in the gray literature including: abstracts of the annual conference of the International Association for Dental Research (IADR) and its regional divisions (1990-2017), ProQuest databases, Capes Journals database, clinical trial records: Current Controlled Trials, International Clinical Trials Registry Platform, ClinicalTrials.gov, and EU Clinical Trials Register. No language, date, and publication restrictions were applied.
Eligibility criteria
Randomized clinical trials (RCTs) with parallel or split face designs in humans comparing the technical use of facial rejuvenation alone versus the technical use of facial rejuvenation together with platelet aggregates were included. The RCTs were excluded if: 1) they performed different rejuvenating treatments associated with platelet aggregates on both sides; 2) the comparison of the use of the treatment together or separate from the platelet aggregates was not directly related to facial rejuvenation.
Study selection and data collection process
Articles were selected considering the titles first, followed by the abstract, and then articles in their entirety, in accordance with the eligibility criteria described. Relevant information from each article selected such as the study design, number and age of participants, interventions, evaluation time, and number of patients lost during treatment (Chart 2), as well as the methods of evaluations of the results (Chart 3) were extracted by researchers (C.F.AQ, C.T.T) using a personalized file.
| Study (ID/year) |
Study Design | Mean age (±SD) | Male patients | Total number of patients | Treatment | Evaluation Time | Patients lost |
|---|---|---|---|---|---|---|---|
| Seied Omid Keyhan 2013 | Clinical face divided | 46,5 ± 31,81 | 8 (32%) | 25 | Fat + PRP Fat + FRP |
1 and 12 months after the procedure | 0 |
| Heba I Gawdat 2017 | Clinical face divided | 41 ± 5,15 | 0 | 20 | Side A (mesotherapy) Side B (PRP) |
1 and 6 months after the final session | 30% - 6 Patients |
| Qiang Hui 2016 | Clinical face divided | 42,1 ± 7,37 | 0 | 13 | Side PRP + Ultra-pulsed fractional
CO2 laser Saline side + Ultra-pulsed fractional CO2 laser |
3 months after the final session | 0 |
| Min Kyung Shin 2012 | Clinical pilot | 43,7 ± 6,0 | 0 | 22 | 11 - laser 11 - laser + PRP | 1 month after the final session | 0 |
| Treatments | Expectation | Pictures | Objective clinical evaluation | OCT | PSL | Histological Analysis | Adverse Effects |
|---|---|---|---|---|---|---|---|
| Fat + PRP x Fat + FRP | Filling/ Rejuvenation | X | X | NR | N.R | NR | X |
| Mesotherapy x PRP | Rejuvenation | X | X | X | X | NR | X |
| CO2 Laser x CO2 Laser + PRP | Rejuvenation | X | X | NR | X | X | X |
| Laser x Laser + PRP | Rejuvenation | X | X | NR | X | NR | X |
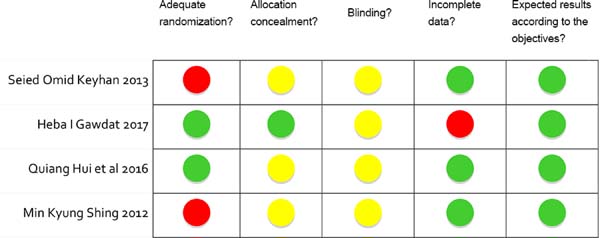
Risk of bias of individual studies
The assays were examined using the Cochrane risk-of-bias tool of the Cochrane Collaboration8.
The evaluation criteria included five items: suitable generation of sequences, allocation concealment, blinding of evaluators and participants, incomplete data results and reports, and selective outcome. The risk of bias for each aspect of quality assessment was in accordance with the recommendations described in the Cochrane Handbook for Systematic Reviews 5.1.0 (http://handbook.cochrane.org)8.
Two of the five areas of Cochrane risk of bias were considered as key areas (randomization and allocation), thus qualifying the studies as “Low risk” of bias if there was an adequate sequence generation and allocation concealment. If one or more criteria were not met, the study would be considered “high” risk of bias and judged as “undefined” when the authors did not report how randomization or allocation was performed.
RESULTS
Study selection
After screening the databases and removing duplicates, 5918 studies were identified (Figure 1). After the removal by titles, 378 studies remained. This number was reduced to 10 after reading the abstracts and full texts were evaluated to verify eligibility. Among them, 6 were excluded: 1) four for not including rejuvenation9-12, 2) one for not comparing one technique to another13, 3) one due to unavailable full text14, and 1 pilot clinical case was added because the information provided fit the proposed subject5.
Characteristics of the studies included
The qualitative synthesis of the four studies included in this review revealed that three presented a study design with a split face1,3,4 and one was a pilot study5. The studies included presented the following comparisons of Fat + PRP x Fat + FRP (Fibrin Rich Plasma), in which the main expectation was facial rejuvenation through facial filling in the cheek/malar region, to refine the facial contour4; mesotherapy x PRP, in which the expectation was facial rejuvenation by intradermal injection of a solution of readymade growth factors - mesotherapy (side A) and PRP (side B) to decrease the signs of aging such as wrinkles, sagging, and pigmentary changes3(Chart 4).
| Results | Objective Clinical evaluation | OCT | PSL | Histological Analysis |
|---|---|---|---|---|
| Fat + PRP x Fat + FRP | p < 0.05 | N.R | N.R | NR |
| Mesotherapy x PRP | p > 0.05 | p > 0.05 | p < 0.05 + PRP | NR |
| CO2 Laser x CO2 Laser + PRP | p < 0.05 | N.R | p < 0.05 + PRP | NR |
| Laser x Laser + PRP | p > 0.05 | N.R | p > 0.05 | p < 0.05 + PRP |
In the study comparing mesotherapy x PRP, evaluations were performed by the evaluators one and six months after the last treatment session by using the Global Aesthetic Improvement Scale (GAIS) through a comparison of photos, besides the Patient Satisfaction Level (PSL), registering their opinion on the benefits of the treatment, and by Optical Coherence Tomography (OCT), comparing epidermal and dermal thickness. Despite the absence of a significant difference (p>0.05) in improvement between the two treated areas by the GAIS and OCT, PSL was significantly higher (p<0.05) in area B (PRP)3.
In the study with ultra-pulsed fractional CO2laser + injection of PRP, evaluations were performed three months after the last treatment session by using the VISIA Complexion Analysis System, also by the comparison of photos, which presented a statistical difference in texture and elasticity (p<0.05) that was higher for the side with the application of ultra-pulsed fractional CO2laser + injection of PRP. Moreover, the PSL of patients who registered their opinion about the benefits of the treatment also showed no significant difference (p<0.05), with results favorable to the ultra-pulsed fractional CO2laser experimental group + injection of PRP1.
In the pilot study, the evaluations were performed one month after the last treatment session, through the application of the GAIS Scale by evaluators through comparison of photos and PSL, registering their opinion about the benefits of the treatment; and, by the histological analysis in which 3 of 7 factors analyzed presented a statistically significant difference (p<0.05), which were higher for the Fractional Laser therapy + PRP5.
Regarding adverse effects, there were no cases of massive edema, prolonged hematomas, or severe pain in the study of facial liposculpture surgery4. When comparing the mesotherapy and PRP treatments, a transient erythema was observed on both sides, which resolved in two days; there was a statistically significant difference in relation to burning sensation (p> 0.01), which was higher on the mesotherapy side3. Erythema, edema, and crusting were evaluated, and were significantly (p >0.05) lower on the ultra-pulsed fractional CO2laser + PRP side1. In the pilot study, there were no serious or persistent side effects during treatment. The duration of erythema was 1-3 days, with no significant difference between the two groups (p >0.05) 5.
Compared to the FRP, PRP presented lower efficacy in relation to the maintenance of facial filling with fat. However, when associated with the other treatment and when compared to mesotherapy, its effectiveness was superior both in the improvement of rejuvenation and the reduction of adverse effects.
Assessment of risk of bias
The assessment of risk of bias of the articles selected is shown in Figure 2. Some authors did not report how concealment of allocation was performed. One study was determined to have a “low» risk of bias (reference), one study presented an “undefined” risk of bias, and the other two were classified as having a “high” risk of bias.
DISCUSSION
The main idea behind the use of platelet aggregates together with another technique of facial rejuvenation involves the bioregenerative action of PRP that stimulates the removal of components of the extracellular matrix and induces the synthesis of new collagen by dermal fibroblasts, thus increasing skin elasticity2,15. The present systematic review was carried out to clarify this issue.
Half of the studies included in this systematic review reported no significant differences in the results when comparing the two types of treatment3,5. Although all selected papers reported expected results in accordance with the objective, the other key areas were classified as “undefined” or with a “high” risk of bias, thus reducing the reliability of the results.
Fat grafts have always been a challenge when inducing the necessary neoangiogenesis in facial liposculpture surgery, which results in significant resorption. Some studies have indicated that FRP provides better fat graft survival compared to PRP due to its retention and the slow release of platelet growth factors4.
To reduce this resorption, a study was carried out to compare the efficiency of PRP versus FRP combined with a fat graft. The results indicated that FRP associated with fat is more effective than a combination of PRP and fat. The difficult injection technique and the lack of FRP fibrin clot are the main disadvantages of FRP and fat compared to PRP4.
In a critical review of the current literature, five of the six selected studies showed an improvement in fat graft survival with the addition of platelet preparation16.
Liang et al.17assessed the efficacy of nanofat-derived stem cells (NFSCs) in facial rejuvenation by intradermal injection of nanofat combined with FRP applied in 103 patients compared to a control group of 128 patients undergoing hyaluronic acid (HA) injections. They concluded that both the injection of nanofat-FRP and HA showed an improvement in the condition of the skin, but the first was associated with a greater patient satisfaction, as well as an improvement in skin texture, suggesting that the injection of nanofat-FRP is safe, highly effective, and a long-lasting method for skin rejuvenation.
Compared to mesotherapy, PRP was superior due to increased patient satisfaction, fewer side effects, and more sustainable results, without a significant difference between the two areas treated regarding improvement according to GAIS and OCT. However, the durability of PRP compared to mesotherapy needs to be better evaluated, since the superiority of PRP was only perceived at the 6-month follow-up. This suggests a shorter life of readymade products when compared to the longevity of the effects of growth factors induced naturally by PRP, a point that suggests more detailed research with longer follow-up periods3.
In addition to a reduction in adverse effects, several studies have reported that PRP led to a clinical improvement when analyzing the effectiveness of PRP combined with fractional carbon dioxide laser ablation in the treatment of atrophic acne scars21. As the MTZ produced by ultra-pulsed CO2 laser has similar histopathological changes to those of wounds, laser therapy associated with PRP accelerates healing and reduces the adverse effects1.
The results of a study involving PRP associated with an ablative carbon dioxide laser showed that despite greater patient satisfaction, there was a greater duration of adverse effects on the experimental side (with the association of PRP), although this was not statistically significant. This worsening of adverse effects can be attributed to the accumulated evidence, demonstrating that platelets contribute to the initiation and propagation of the inflammatory process18.
When PRP was combined with microneedling, no articles were found relating to facial rejuvenation per se, but mostly, the safety and efficacy of treatment in facial aesthetics was assessed, together with the improvement of post-acne atrophic scars.
Facial harmonization is a set of aesthetic procedures that aim to harmonize the teeth aesthetically and functionally with the mouth and face. Although it is not yet a specialty in dentistry, it is important to know the definition of the area of action, which, according to Resolution 176, dated September 6, 2016, authorizes the use of botulinum toxin and facial fillers by a dental surgeon for functional and/or aesthetic therapeutic purposes if they do not extrapolate their anatomical area of activity.
Given that the clinical-anatomical area of the dental surgeon includes above the hyoid bone, up to the nasal point (bones of the nose) and anterior to the tragus, covering adjacent structures and the like, and for the cases of non-surgical procedures, of the aesthetic purpose of facial harmonization in its breadth, it also includes the upper third of the face.
Furthermore, according to resolution 158/2015 of the Federal Official Journal, the Federal Council of Dentistry regulated the use of platelet aggregates for non-transfusion purposes in dentistry, making it possible to collect blood to obtain PRP and FRP in a dental or surgical center. This establishes that not only dermatologists, but also the qualified dental surgeons, have the possibility and competence to perform a facial rejuvenation treatment with the use of platelet aggregates.
This systematic review showed that, due to the scarce evidence and the risk of “undefined” bias, there is need for further research, especially randomized controlled trials, that test alternatives to assess the best form of application of platelet aggregates for facial rejuvenation.
Therefore, further randomized controlled clinical studies should be performed that compare the use of platelet aggregates with other facial rejuvenation techniques, since even with good results, few are found in the literature.
CONCLUSION
This systematic review found that there are few studies in the literature that compare the use of platelet aggregates in facial rejuvenation, and those that are available have an “undefined” or “high” risk of bias. Further well-designed clinical studies are needed that compare the use of platelet aggregates associated with facial rejuvenation techniques.
COLLABORATIONS
|
CLMS |
Final manuscript approval, supervision. |
|
CFA |
Data curation, writing - original draft preparation. |
|
LHKC |
Data curation. |
|
LMW |
Analysis and/or data interpretation, conception and design study, formal analysis. |
|
JLG |
Analysis and/or data interpretation, conception and design study. |
|
JCZ |
Writing - review & editing. |
REFERENCES
1. Hui Q, Chang P, Guo B, Zhang Y, Tao K. The Clinical Efficacy of Autologous Platelet-Rich Plasma Combined with Ultra-Pulsed Fractional CO2 Laser Therapy for Facial Rejuvenation. Rejuvenation Res. 2017;20(1):25-31. DOI: https://doi.org/10.1089/rej.2016.1823
2. Conde Montero E, Fernández Santos ME, Suárez Fernández R. Platelet-rich plasma: applications in dermatology. Actas Dermosifiliogr. 2015;106(2):104-11. DOI: https://doi.org/10.1016/j.ad.2013.12.021
3. Gawdat HI, Tawdy AM, Hegazy RA, Zakaria MM, Allam RS. Autologous platelet-rich plasma versus readymade growth factors in skin rejuvenation: A split face study. J Cosmet Dermatol. 2017;16(2):258-64. DOI: https://doi.org/10.1111/jocd.12341
4. Keyhan SO, Hemmat S, Badri AA, Abdeshahzadeh A, Khiabani K. Use of plate- let-rich fibrin and platelet-rich plasma in combination with fat graft: which is more effective during facial lipostructure? J Oral Maxillofac Surg. 2013;71(3):610-21.
5. Shin MK, Lee JH, Lee SJ, Kim NI. Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol Surg. 2012;38(4):623-30. DOI: https://doi.org/10.1111/j.1524-4725.2011.02280.x
6. Willemsen JCN, Van Dongen J, Spiekman M, Vermeulen KM, Harmsen MC, van der Lei B, et al. The Addition of Platelet-Rich Plasma to Facial Lipofilling: A Double-Blind, Placebo-Controlled, Randomized Trial. Plast Reconstr Surg. 2018;141(2):331-43.
7. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. PMID: 19622551 DOI: https://doi.org/10.1136/bmj.b2535
8. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. DOI: https://doi.org/10.1136/bmj.d5928
9. Ibrahim MK, Ibrahim SM, Salem AM. Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: a split face comparative study. J Dermatolog Treat. 2018;29(3):281-6. PMID: 28782384
10. Nofal E, Helmy A, Nofal A, Alakad R, Nasr M. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg. 2014;40(8):864-73.
11. Chawla S. Split Face Comparative Study of Microneedling with PRP Versus Mi- croneedling with Vitamin C in Treating Atrophic Post Acne Scars. J Cutan Aesthet Surg. 2014;7(4):209-12. DOI: https://doi.org/10.4103/0974-2077.150742
12. Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol. 2016;15(4):434-43. PMID: 26748836
13. Hersant B, SidAhmed-Mezi M, Niddam J, La Padula S, Noel W, Ezzedine K, et al. Efficacy of autologous platelet-rich plasma combined with hyaluronic acid on skin facial rejuvenation: A prospective study. J Am Acad Dermatol. 2017;77(3):584-6. PMID: 28807118
14. Kang BK, Shin MK, Lee JH, Kim NI. Effects of platelet-rich plasma on wrinkles and skin tone in Asian lower eyelid skin: preliminary results from a prospective, randomised, split-face trial. Eur J Dermatol. 2014;24(1):100-1.
15. Arshdeep, Kumaran MS. Platelet-rich plasma in dermatology: boon or a bane? Indian J Dermatol Venereol Leprol. 2014;80(1):5-14. PMID: 24448117
16. Sclafani AP, Azzi J. Platelet Preparations for Use in Facial Rejuvenation and Wound Healing: A Critical Review of Current Literature. Aesthetic Plast Surg. 2015;39(4):495-505. DOI: https://doi.org/10.1007/s00266-015-0504-x
17. Liang ZJ, Lu X, Li DQ, Liang YD, Zhu DD, Wu FX, et al. Precise Intradermal Injection of Nanofat-Derived Stromal Cells Combined with Platelet-Rich Fibrin Improves the Efficacy of Facial Skin Rejuvenation. Cellular physiology and biochemistry. Cell Physiol Biochem. 2018;47(1):316-29. DOI: https://doi.org/10.1159/000489809
18. Zhu JT, Xuan M, Zhang YN, Liu HW, Cai JH, Wu YH, et al. The efficacy of autologous platelet-rich plasma combined with erbium fractional laser therapy for facial acne scars or acne. Mol Med Rep. 2013;8(1):233-7. PMID: 23653117 DOI: https://doi.org/10.3892/mmr.2013.1455
1. Universidade Positivo, Escola de Ciências
da Saúde, Curitiba, PR, Brazil.
Corresponding author: Carmen Lucia Mueller Storrer, Rua Professor Pedro Viriato Parigot de Souza, 5300, Campo Comprido, Curitiba, PR, Brazil, Zip Code: 81280-330. E-mail: carmen.storrer@gmail.com
Article received: December 13, 2018.
Article accepted: February 10, 2019.
Conflicts of interest: none.









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter