

Ideas and Innovation - Year 2019 - Volume 34 -
Preoperative imaging assessment of hidradenitis suppurativa
Avaliação pré-operatória por imagem da hidradenite supurativa
ABSTRACT
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease characterized by painful deep subcutaneous nodules with phlogistic signs, which are initially hard and progress to have a soft consistency. It occurs in 1-4% of the world population. Etiology of HS is still poorly understood and is suggested to occur due to occlusion of the apocrine duct of the hair follicles by triggering factors such as friction of the adipose tissue and poor hygiene, among others. Diagnosis is eminently clinical, through the identification of typical recurrent lesions that include nodules, abscesses, sinus tracts, or scars. There are no pathognomonic tests used to confirm its presence. Progression is variable and difficult to manage, which can be done with topical or systemic therapy or surgical excision. This work reviews the imaging assessment of HS and shows images of a case assessed by magnetic resonance imaging. Imaging assessment, although not specific enough for a diagnosis, is useful to determine the extent of the disease and to exclude differential diagnoses. Moreover, magnetic resonance imaging has an important role in the assessment of anogenital lesions and a potential to reduce recurrences.
Keywords: Hidradenitis suppurativa; Magnetic resonance imaging; Reconstructive surgical procedures; Ultrasonography; Abscess
RESUMO
A hidradenite supurativa (HS) é uma doença inflamatória crônica da pele caracterizada por apresentar nodulações em níveis profundos da pele, dolorosas e com sinais flogísticos, inicialmente enrijecidas e que evoluem para consistência amolecida. Ocorre em 1 a 4% da população mundial. A sua etiologia ainda é pouco conhecida, sugere-se que aconteça devido à oclusão do ducto apócrino dos folículos pilosos por fatores precipitantes como fricção de tecido adiposo, higiene precária, entre outras. Seu diagnóstico é eminentemente clínico, pela identificação de lesões típicas recorrentes em forma de nodularidades, abcessos, tratos fistulosos ou cicatrizes. Não há testes patognomônicos. Sua evolução é variável e de difícil manejo, o qual pode ser feito com terapia tópica, sistêmica ou por exérese cirúrgica. Este trabalho revisa a avaliação por imagem da hidroadenite supurativa e demonstra imagens de um caso avaliado por ressonância magnética. A avaliação por exames de imagem, apesar de pouco específica para firmar diagnóstico, é muito útil na determinação da extensão da doença, assim como na exclusão de diagnósticos diferenciais, destacando-se o papel da ressonância magnética na avaliação das lesões anogenitais, com potencial de reduzir recorrências.
Palavras-chave: Hidradenite supurativa; Imagem por ressonância magnética; Procedimentos cirúrgicos reconstrutivos; Ultrassonografia; Abscesso
INTRODUCTION
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory skin disease characterized by painful deep subcutaneous nodules with phlogistic signs, which are initially hard and progress to have a soft consistency. Complications include the formation of fistulas and suppuration.
HS occurs in 1-4% of the world population, most commonly in the second and third decades of life, with a higher incidence at 23 years of age, and is more common in women (3.3F:1M), with an estimated prevalence of 1 in 300 adults. It mostly affects the inframammary (23%) and inguinal (93%) regions in women and the gluteal (40%) and perianal regions (51%) in men, all rich in apocrine glands1.
Etiology of HS is still poorly understood and is suggested to occur due to occlusion of the apocrine duct of the hair follicles by triggering factors such as friction of the adipose tissue, poor hygiene, excessive sweating, heat, tight clothing, depilation, and deodorants. Diagnosis is eminently clinical through the identification of typical recurrent lesions that include suppurative and/or painful nodules, abscesses, sinus tracts, or scars1,2.
There are no pathognomonic tests, but laboratory abnormalities in leukocyte counts and C-reactive protein levels can be detected. The possible differential diagnoses are abscesses, carbuncles, lymphogranuloma venereum, inflammation of the Bartholin’s gland, furunculosis, and infection of epidermoid cysts, among others.
HS is a disease with variable progression and is difficult to manage, which can be done with topical or systemic therapy or by surgical excision. Imaging assessment, although not specific enough for a diagnosis, is useful to determine the extent of the disease, can exclude differential diagnoses, and allow for planning of the surgical procedure. The objective of this work was to review the imaging assessment of HS and to depict a case with magnetic resonance imaging.
METHODS
This article is a literature review. Articles in English, Portuguese, and Spanish were selected in the SciELO, PubMed, Bireme, and Google databases from January 2017 to February 2018. The following keywords were used: “hidradenitis suppurativa,” “magnetic resonance,” “ultrasound,” “acne inversa”.
RESULTS
Although the diagnosis of HS is clinical, exams can have an important role in the grading, characterization, assessment of differential diagnoses, and surgical planning, especially magnetic resonance imaging, with the potential to reduce postoperative recurrences.
DISCUSSION
HS is a chronic and slowly-evolving disease. The signs and symptoms of the disease can emerge years after the first presentation and its clinical diagnosis is based on three criteria2:
1. Typical lesions (that is, painful deep-seated nodules): abscesses, bridge scars, draining fistulas, and pseudocomedones
2. Lesions in at least one typical area: armpits, inframammary region in intermammary folds, groin, perineum, or buttocks
3. Two recurrences of the lesions in a period of 6 months
Hurley’s classification stratifies the disease in three stages. Stage I is characterized by the presence of an abscess, single or multiple, without draining fistulas or scars. Stage II is characterized by a recurrent abscess, single or multiple, with draining fistulas, scars and well-spaced lesions. In stage III, there is diffuse involvement or with multiple interconnected fistulas and abscesses throughout the region2.
There is no single effective or curative treatment for HS, but there is a wide-range of therapies for its management, which include diverse treatments such as antibiotic therapy, immunosuppression, TNF-alpha inhibitor drugs, surgery, and radiation2. Most therapies for HS have low levels of evidence (categories C and D).
The surgical approach of mild to moderate cases of HS (Hurley stages I and II) is performed through local excisions and primary closure. In the more severe cases (Hurley stage III), the radical surgical approach is the treatment of choice and has presented better results, with low recurrence rates. It consists in more extensive surgeries with closure by secondary intention or grafts2.
Assessment using only clinical parameters generally underestimates the extent and staging of the lesions3. Based on ultrasound findings, Zarchi & Jemec4 changed the conduct in 28 of 32 patients (82%), due to under-staging of the clinical assessment. Moreover, Worstman et al.5 identified collections not clinically diagnosed in 26 of 34 patients (76%) by ultrasonography, in addition to subclinical fistulas in 10 patients (29%).
There is evidence that 64% of patients with HS in the anogenital region present anal fistulas and its incomplete resection is one of the major causes of HS recurrence (up to 25%). Therefore, clinical assessment using imaging methods becomes fundamental and Doppler ultrasonography and magnetic resonance imaging (MRI) stand out among the existing imaging techniques. Ultrasonography is a more accessible and available method and is a powerful tool for the initial imaging exam in the assessment of HS. On the other hand, MRI stands out for observations of fistulous tracts, especially in anogenital lesions3, providing high-definition images of the hypodermis and deep tissues, and is useful when there is an association with other diseases, such as Crohn’s disease3.
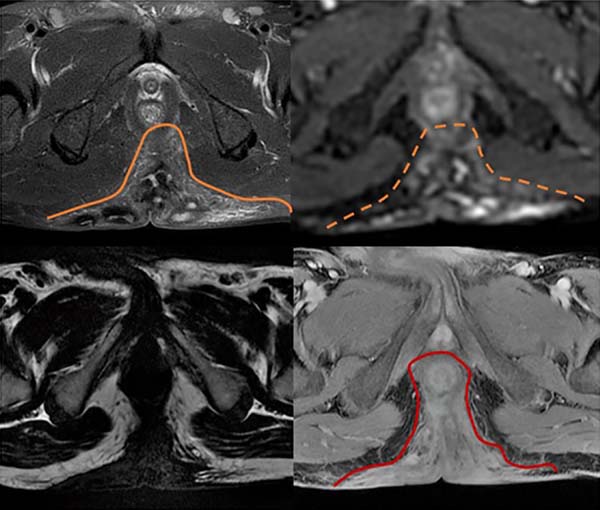
The imaging results include fistulas, granulomas, abscesses, scar bridges, and dermal and subcutaneous thickening of well-delimited borders6. Abscesses are characterized by circumferential morphology in the subcutaneous tissue, with a low signal in T1 and high in T2, with evident contrast enhancement due to the contrast medium and restricted diffusion (Figures 1 to 3). Fistulas in the subcutaneous and dermal tissues of the anal canal and the distal part of the rectum can mimic Crohn’s disease or cryptoglandular disease. These diseases can also coexist with HS, which impairs the ability to determine a diagnosis6,7.
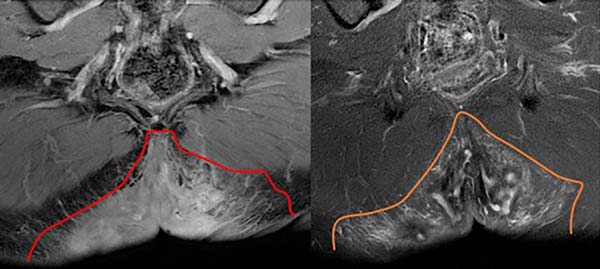
To differentiate HS from cryptoglandular disease, the time to disease progression should be considered, which tends to be shorter for the latter. Moreover, cryptoglandular disease is limited to the perianal region. In relation to Crohn’s disease, HS presents more inflammatory findings (subcutaneous edema and granulomas), greater bilaterality, less occurrence of fistulas and less sphincter involvement8. Biopsies are required in cases of doubt with other diagnoses such as atypical perianal Crohn’s disease, carcinoma, and tuberculous ulcer.
CONCLUSION
Although the diagnosis of hidradenitis suppurativa is eminently clinical, the complementation of the clinical assessment with imaging exams has the potential to reduce postoperative recurrences due to better staging and characterization of the lesions.
The most important imaging methods for the assessment of HS include Doppler ultrasonography and magnetic resonance imaging. MRI is particularly relevant in more severe cases of the disease and is a useful technique to establish a diagnosis for HS, determine the extent of the lesion, and plan the optimal therapeutic management. MRI results are relatively nonspecific, with thickening of dermal and subcutaneous tissues, with low intensity signal in T1 and high in T2 and STIR. However, the presence of these findings together with fistulas, sinus tracts, and scars, especially in the anal canal, are highly suggestive of HS.
COLLABORATIONS
|
AAL |
Analysis and/or data interpretation, conception and design study, final manuscript approval, methodology, writing - original draft preparation, writing - review & editing. |
|
GNM |
Analysis and/or data interpretation, conception and design study, data curation, writing - original draft preparation. |
|
BMMLD |
Conception and design study, data curation, writing - original draft preparation. |
|
GDS |
Conception and design study, conceptualization, project administration, supervision, writing - review & editing. |
|
LQS |
Conceptualization, methodology, project administration, resources, supervision. |
REFERENCES
1. Martorell A, Segura Palacios JM. Ultrasound examination of hidradenitis suppurativa. Actas Dermosifiliogr. 2015;106 Suppl 1:49-59. DOI: https://doi.org/10.1016/S0001-7310(16)30007-2
2. Revuz J. Hidradenitis suppurativa. Presse Med. 2010;39(12):1254-64. PMID: 20965688 DOI: https://doi.org/10.1016/j.lpm.2010.08.003
3. Wortsman X. Imaging of Hidradenitis Suppurativa. Dermatol Clin. 2016;34(1):59-68. DOI: https://doi.org/10.1016/j.det.2015.08.003
4. Zarchi K, Jemec GB. The role of ultrasound in severity assessment in hidradenitis suppurativa. Dermatol Surg. 2014;40(5):592. DOI: 10.1111/dsu.12437 DOI: https://doi.org/10.1111/dsu.12437
5. Wortsman X, Moreno C, Soto R, Arellano J, Pezo C, Wortsman J. Ultrasound in-depth characterization and staging of hidradenitis suppurativa. Dermatol Surg. 2013;39(12):1835-42. DOI: https://doi.org/10.1111/dsu.12329
6. Montaña CN, Labra WA, Panussis FD. Hidradenitis supurativa: evaluación por resonancia magnética. 2014. Rev Chil Radiol. 2014;20(4):159-63.
7. Kelly AM, Cronin P. MRI features of hidradenitis suppurativa and review of the literature. AJR Am J Roentgenol. 2005;185(5):1201-4. PMID: 16247134 DOI: https://doi.org/10.2214/AJR.04.1233
8. Monnier L, Dohan A, Amara N, Zagdanski AM, Drame M, Soyer P, et al. Anoperineal disease in Hidradenitis Suppurativa : MR imaging distinction from perianal Crohn’s disease. Eur Radiol. 2017;27(10):4100-9. DOI: https://doi.org/10.1007/s00330-017-4776-1
1 . Hospital de Base do Distrito Federal, Brasília,
DF, Brazil.
2 . Universidade Católica de Brasília, Brasília,
DF, Brazil.
Corresponding author: Arthur Ataíde Lopes, SEPS 710/910, Ed. Via Brasil, Galeria, Loja 40, Asa Sul, Brasília, DF, Brazil, Zip Code 70390-108. E-mail: arthurbsb@gmail.com
Article received: April 22, 2018.
Article accepted: April 16, 2019.
Conflicts of interest: none.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter