

Ideas and Innovation - Year 2019 - Volume 34 -
Reconstruction of the lower eyelid using a full-thickness upper eyelid transposition flap
Reconstrução de pálpebra inferior com uso do retalho de transposição da pálpebra superior de espessura total
ABSTRACT
Introduction: The best method to reconstruct an anatomical unit is to replace the injured area with the same tissues.
Methods: Three patients with basal cell carcinoma in the lower eyelid underwent full-thickness lower eyelid excision, followed by immediate reconstruction with a single-stage fullthickness transposition of the upper eyelid tissue.
Results: The patients had almost no complications, and the functions of total closure and protection of the eyeballs of the eyelids were maintained.
Conclusion: The flap proved to be feasible and is an alternative choice for reconstruction of the lower eyelid.
Keywords: Palpebral neoplasm; Surgical flap; Reconstructive surgical procedure; Basal cell carcinoma
RESUMO
Introdução: O melhor método para reconstruir uma unidade anatômica é substituir a área
lesada pelos mesmos tecidos.
Métodos: Três pacientes que apresentavam carcinomas basocelulares na pálpebra inferior
foram submetidos à excisão, seguida de reconstrução imediata com a
transposição em espessura total de tecido da pálpebra superior em um só
tempo.
Resultados: Os pacientes evoluíram quase sem complicações, as pálpebras mantiveram suas
funções de fechamento total e proteção do globo ocular.
Conclusão: O retalho se mostrou factível e é mais uma alternativa para reconstruir a
pálpebra inferior.
Palavras-chave: Neoplasias palpebrais; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Carcinoma basocelular
INTRODUCTION
The best method for reconstructing an anatomical unit is the replacement of the injured area with the same tissues. However, in many situations, when this is not possible, the surgeon must use similar structures. This occurs with the current techniques described for the reconstruction of defects of total thickness that compromise more than one third of the extension of the lower eyelids. Local flaps associated with cartilage and mucous grafts are then used to recover the delicate components of the eyelid (thin skin, orbicular muscle, tarsus, and conjunctiva).
OBJECTIVE
In this study, we aimed to describe a technique for reconstruction of the lower eyelid that allows tissue reconstruction according to the precepts mentioned.
METHODS
Three patients with basal cell carcinoma underwent full-thickness lower eyelid excision followed by immediate reconstruction. The surgeries were performed in a hospital operating room. The patients were in supine position under sedation. In all of them, an eyelid protector was placed, and the solution was locally infiltrated with lidocaine and adrenaline. In two patients, half of the extension was reconstructed; and in one, two thirds. The reconstructions were performed using the technique herein.
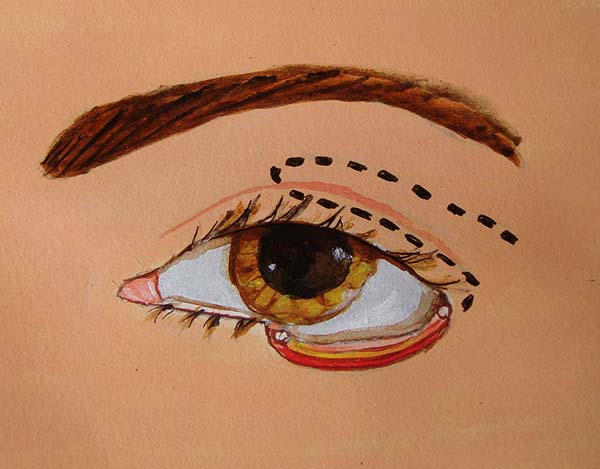
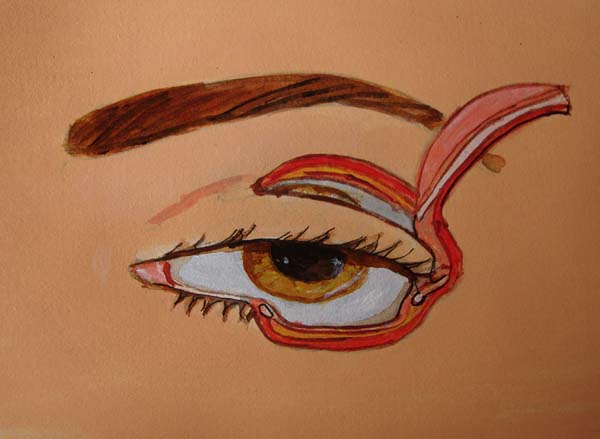
In the upper eyelid, a full-thickness lateral flap was raised, with the lower edge located 2 mm below the eyelid groove with sufficient width and length to cover the defect. The conjunctiva, part of the tarsus (2 mm wide), orbicular muscle, and skin were included in the flap. The septum and aponeurosis of the eyelid lift were sectioned. The flap was then transposed to cover the defect.
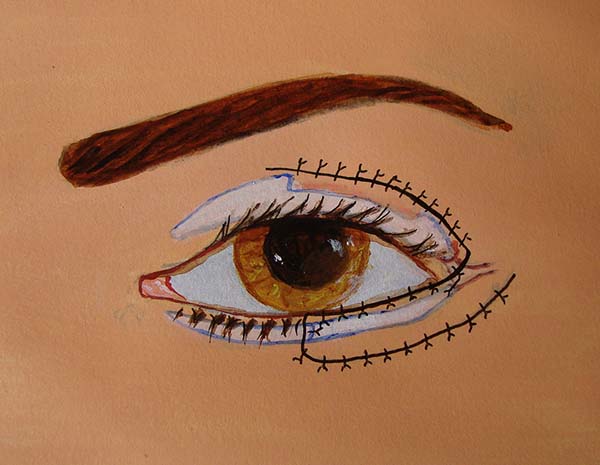
The conjunctiva was sutured with the remaining conjunctiva using Vicryl 6-0. The medial edge of the tarsus was sutured with the lateral edge of the remaining lower tarsus and the lateral edge at the edge of the upper tarsus; thus, the lateral corner was reconstructed. The orbicular muscle was sutured with the inferior remnant, and finally, the skin was sutured with Mononylon 6-0. Few simple sutures of Vicryl 6-0 were made in the conjunctiva and skin, constituting the lower edge of the eyelid. The donor area was closed in layers. The septum, palpebral elevator aponeurosis, and orbicular muscle were sutured to the cranial edge of the tarsus with Mononylon 5-0, and the skin was sutured with Mononylon 6-0 (Figures 1 to 6).
The patients were followed-up monthly for 6 months. Occlusive dressings were not required. They were instructed to use eye drops for 15 days for moisturizing the eye and an ointment when sleeping. The stitches were removed in 7 days.
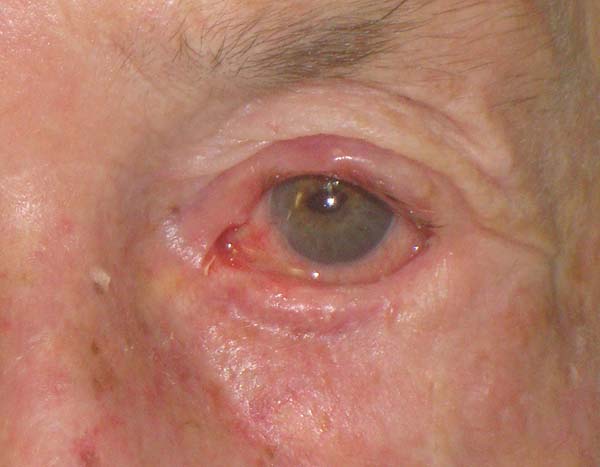
RESULTS
The patients had no complications except for a dot granuloma, which was removed under local anesthesia, and a temporary asymptomatic retraction of the upper eyelid. The functions of total closure and protection of the eyeball of the eyelids were maintained. Scar retraction, ectropion, entropion, or lagophthalmos was not observed. The aesthetic result was very satisfactory, with discrete scars in the donor and recipient areas (Figures 7 and 8).
DISCUSSION
The tissues that are part of the eyelid are unique and cannot be easily replaced with similar tissues. Although most eyelid tumors appear at more advanced ages and show tissue redundancy, it should be noted that the upper eyelid tissue, which is important for the corneal protection function, is used in transposition flaps; therefore, it is essential to evaluate the degree of tissue elasticity and redundancy in the preoperative period. In addition to reconstructing the defect with equal amounts of the tissues (skin, tarsus, and conjunctiva), the proposed flap is transposed in a monoblock, thus, ensuring circulatory safety, less postoperative edema, and increased simplicity of operation.
Fricke1 described a similar pattern of upper eyelid skin transposition, but without parts of the tarsus and conjunctiva, thus, being useful for reconstruction of only superficial defects. Papp et al.2 described a flap of total advancement thickness by continuously incising the lower and upper eyelids and sectioning the lateral ligament. The most frequently used current techniques reconstruct the anterior and posterior lamellae with different methods.
The most commonly used flap for the anterior lamella is the rotation flap for the facial skin described by Mustardé3. In Brazil, the V-Y advancement technique of Destro et al. is worth mentioning4,5. The posterior lamella is reconstructed with compound grafts, such as the mucoperichondrial of the nasal septum or flap in two-stage tarsal and conjunctiva of the upper eyelid (Hughes6). In all cases, the lamellae are constructed separately, which often results in very heavy eyelids with some degree of retraction.
CONCLUSION
The full-thickness eyelid transposition flap enabled functional and aesthetic reconstruction of the half or two-thirds of the lower eyelid in patients who underwent single-stage exeresis of the eyelid tumors.
REFERENCES
1. Fricke JCG. Bildung neuer Augenlieder (Blepharoplastik) nach Zerstorüngen und darduch hervorgebrachten Auswärtswendungenderselben. Hamburg: Pethes und Bessler: 1829.
2. Papp C, Maurer H, Geroldinger E. Lower eyelid reconstruction with the upper eyelid rotation flap. Plast Reconstr Surg. 1990;86(3):563-5. DOI: https://doi.org/10.1097/00006534-199009000-00031
3. Mustarde JC. Repair and reconstruction of the orbital region. 2nd ed. Edinburgh: Churchill Livingstone; 1980.
4. Destro MW, da Silva AL, Speranzini MB. Lower eyelid repair utilising triangular skin flaps with subcutaneous pedicles. Br J Plast Surg. 1991;44(5):363-7. PMID: 1873616 DOI: https://doi.org/10.1016/0007-1226(91)90150-I
5. Lima DA. Reconstrução total de pálpebra inferior com associação dos retalhos de Hughes e Destro. Rev Bras Cir Plást. 2018;33(3):364-73.
6. Hughes WL. Total lower lid reconstruction: technical details. Trans Am Ophthalmol Soc. 1976;74:321-9. PMID: 867633
1. Clínica Dr. Jason Figueiredo, Jundiaí, SP,
Brazil.
Corresponding author: Jason César Abrantes de Figueiredo, Rua 23 de maio, 790, sala 41, Vianelo, Jundiaí, SP, Brazil. Zip Code: 13207070.. E-mail: figueiredoaj@uol.com.br
Article received: January 25, 2019.
Article accepted: April 21, 2019.
Conflicts of interest: none.














 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter