

Original Article - Year 2019 - Volume 34 -
Post-Bariatric surgery: six surgeries in two steps
Cirurgia pós-bariátrica: seis cirurgias em dois tempos
ABSTRACT
Introduction: Weight reduction achieved after bariatric surgery can result in deformities of various parts of the body. The need for reduction of leftover skin and body remodeling makes patients seek body contouring surgery to improve their quality of life. The aim of the study was to present a protocol for post-bariatric plastic surgery at Daher Hospital.
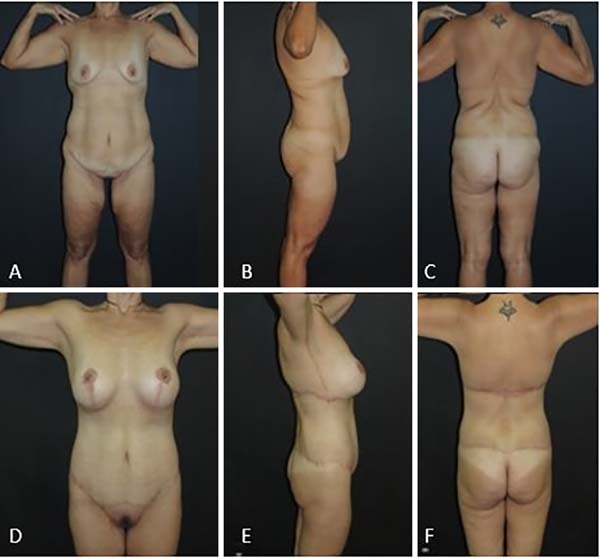
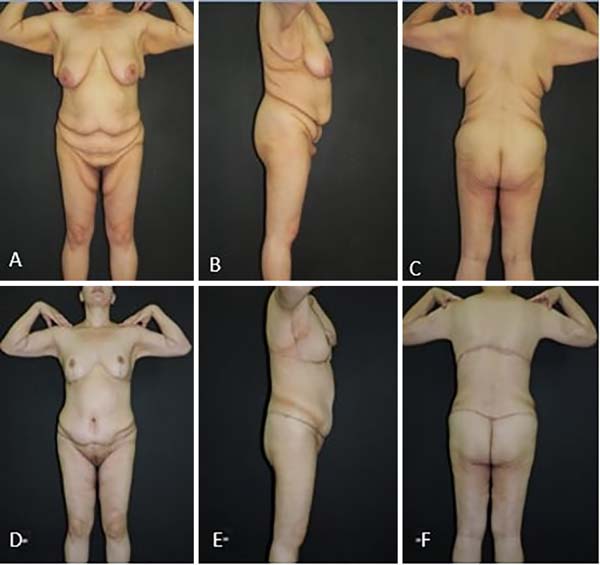
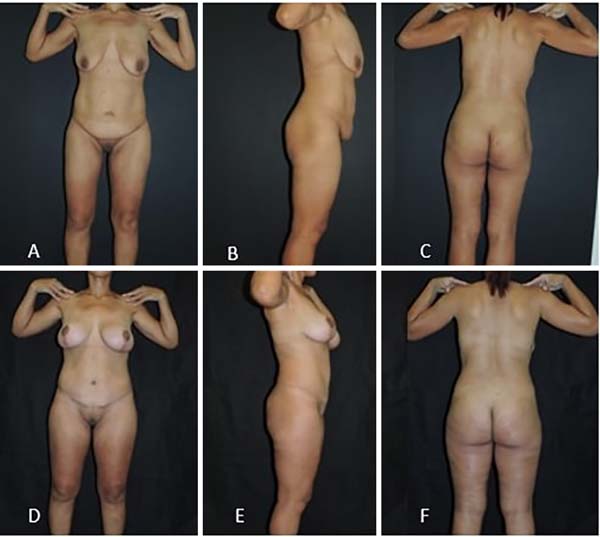
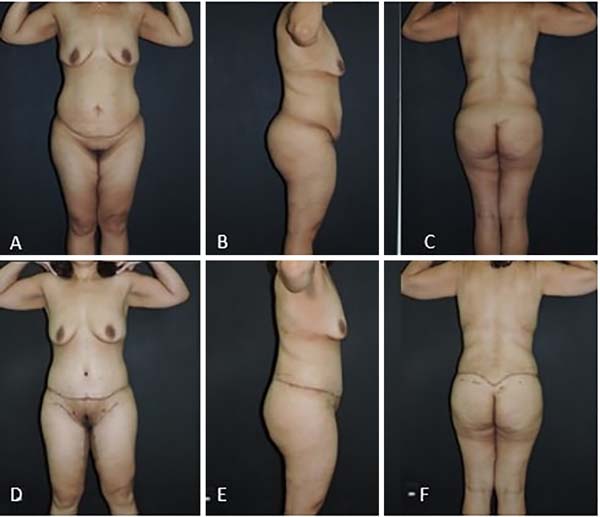
Methods: This was a retrospective longitudinal observational study. As routine protocol, we divided the procedures into two steps, performed in different surgical stages, which we termed the two-level principle. Herein we describe the routine of pre, intra, and postoperative care, as well as details of the surgical techniques. Photographic images were analyzed by an external evaluator.
Results: The study included 13 ex-obese patients, with a mean age of 44 years. Of them, 6 patients underwent lower- and upper-level surgeries and another 6 underwent lower-level surgeries. The mean surgical time for the lower level was 4 hours and 54 minutes and that for the upper level was 4 hours and 5 minutes. A total of 92.30% of the patients were satisfied with the results. An external evaluator classified 92.30% of the cases as good or great.
Conclusion: Circumferential abdominoplasty has immense benefits and complementary surgeries are vital for a satisfactory result. Reduction of the surgical time requires great synchronization of the surgical team, which allows procedures to be performed simultaneously by multiple surgical teams working in different body parts. Satisfactory results and low complication rates allow the applicability of our routine in post-bariatric patients.
Keywords: Plastic surgery; Bariatric surgery; Obesity; Protocols; Reconstructive Surgical Procedures
RESUMO
Introdução: Redução ponderal conseguida após cirurgia bariátrica pode resultar em
deformidades de diversos segmentos corporais. Necessidade da redução das
sobras de pele e da remodelação do corpo faz com que a cirurgia do contorno
corporal seja procurada por pacientes para melhorar a qualidade de vida.
Objetivo do estudo é apresentar a rotina de cirurgia plástica pós-bariátrica
do Hospital Daher.
Métodos: Estudo observacional longitudinal retrospectivo. Como rotina, dividimos os
procedimentos em duas etapas realizadas em atos operatórios distintos:
princípio dos dois andares. Descrevemos a rotina dos cuidados pré, intra e
pós-operatório, bem como detalhes das técnicas cirúrgicas. Imagens
fotográficas foram analisadas por um avaliador externo.
Resultados: Estudo composto 13 pacientes ex-obesos, média de idade de 44 anos. Seis
pacientes foram submetidos a cirurgia do andar inferior e superior e outros
6 apenas do andar inferior. Tempo médio da cirurgia do andar inferior foi de
4 horas e 54 minutos e do andar superior foi de 4 horas e 5 minutos. 92,30%
dos pacientes mostraram-se satisfeitos com o resultado. Avaliação externa
revelou uma taxa de 92,30% dos casos classificados como bons ou ótimos.
Conclusão: Abdominoplastia circunferencial traz grandes benefícios e as cirurgias
complementares são primordiais para um resultado satisfatório. Redução do
tempo cirúrgico exige grande sincronização da equipe cirúrgica, permitindo
realizar procedimentos combinados por times cirúrgicos trabalhando em
compartimentos corporais diferentes, em tempo simultâneo. Resultados
satisfatórios obtidos e baixos índices de complicação possibilitam
aplicabilidade da nossa rotina em pacientes pós-bariátricos.
Palavras-chave: Cirurgia plástica; Cirurgia bariátrica; Obesidade; Protocolos; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
The prevalence of overweight and obesity is increasing globally. More than one in 10 persons worldwide is obese and it is believed that 2.2 billion people are overweight, causing millions of deaths per year1,2. Brazil ranks fifth in the world ranking of this disease, with about 60 million overweight people and 22 million obese people, which corresponds to 17% of its population3.
Obesity leads to increased mortality due to the risk of other diseases, such as diabetes mellitus type 2 (DM2), systemic arterial hypertension (SAH), dyslipidemia, sleep apnea, cardiovascular diseases, and certain types of cancers, besides undeniable discomfort and a low quality of life (QOL) due to body deformity4. Bariatric surgery provides, in addition to sustained weight loss, additional benefits to people with obesity-related comorbidities and reduces the relative risk of death in these patients5,6. Consequently, the demand for surgical treatment of this disease has increased significantly in recent years.
The weight reduction achieved after bariatric surgery is around 40% to 60% of the initial weight and may result in deformities in several body parts. Consequently, some patients have excess skin that can cause problems related to movement, wearing clothes, dermatitis, changes in posture, psychological problems, poor self-esteem, and a low QOL as a result of the surgery3.
Due to the need to remodel the body contour, body contour surgery is performed. It is defined as a reconstructive and functional surgery. Data from the literature indicates that more than 70% of patients with massive weight loss seek this type of procedure to improve their quality of life7,8.
OBJECTIVE
The present study aims to describe the routine planning, marking and method of execution, and the results of plastic surgery at Daher Lago Sul Hospital performed for post-bariatric body contour surgery cases, describing the two-level principle.
METHODS
This is a retrospective, longitudinal, observational study conducted at the Plastic Surgery Department of Daher Lago Sul Hospital, Brasília - Federal District, from March 2015 to April 2017.
This research paper followed the legal guidelines approved by the Resolution 196/96 of the National Health Council with regard to research involving human beings and in accordance with the principles of the Declaration of Helsinki.
This study followed a nonrandom sample selection technique and was based on whether post-bariatric lower and/or upper level lift procedures were performed.
The inclusion criteria in the study were:
1. Ex-obese patients with stable weight for a minimum of 6 months and body mass index (BMI) between 18.5 and 29.9 kg/m2;
2. Presence of body contour deformities arising from weight loss in the lower and/ or upper parts of the body;
3. Patients classified as ASA 1 or ASA 2 according to American Society of Anesthesiology criteria.
The exclusion criteria were:
1. Stable weight for less than 6 months;
2. BMI > 29.9 kg/m2;
3. Patients classified as ASA greater than or equal to 3.
The variables evaluated were sex, age, weight loss after bariatric surgery, surgery time, time between the first and second surgical procedure, post-operative surgical complications, weight of the patient, BMI, and length of hospital stay.
The patient’s level of satisfaction with the surgical outcome was assessed during post-operative follow-up visits. The patients responded whether they were satisfied or not satisfied with the procedure.
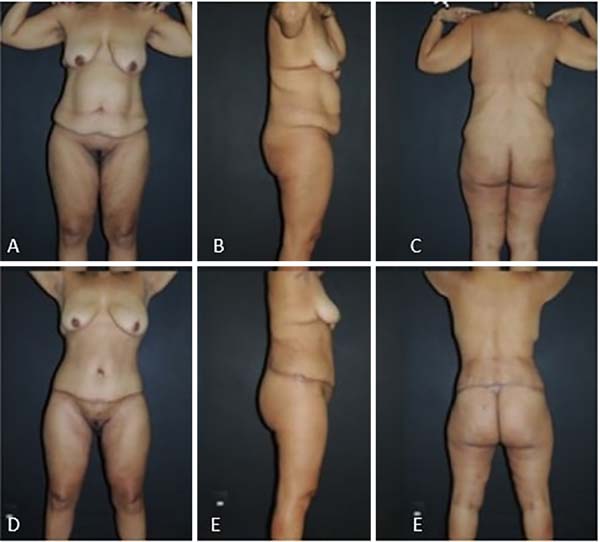
A comparative analysis of pre-operative and at least 2 months post-operative photographic images was performed by a plastic surgeon associated with the Brazilian Society of Plastic Surgery (BSPS) who did not participate in the surgical procedures, and the results were classified as great, good, fair, and poor.
Surgical Technique
The surgery was divided into 2 stages according to protocol: lower level (abdomen, lower back, buttocks, and thighs) and upper level (upper back, breasts and arms). The order of the procedure was variable, according to the patient’s complaints; but always performed in two stages, and according to the patient’s preference to start with either the lower or upper level.
The markings were always performed with the patient in the orthostatic position initially, and then completed in dorsal, ventral, and seated positions.
General anesthesia was routinely used. Asepsis and antisepsis were always performed 360 degrees, allowing for a change to a decubitus position at the operating table, according to the surgical procedure and was performed sequentially, shortening the surgical time. The legs were also bandaged to prevent venous thrombosis. Antibiotic prophylaxis with 1 g of cefazolin was routinely administered, and was repeated if the surgery exceeds 4 hours.
The surgical team consisted of at least 5 members, including the primary surgeon, with at least 3 assistant surgeons, and a surgical technician.
Lower body:
A solution of saline and adrenaline (1: 500,000) was administered with 2 ampoules of 2% lidocaine.
The procedure started with the patient in the ventral decubitus position and a “gull wing” incision was performed (or with a dorsal incision facing upwards, if there were large, well-defined folds in the back) limited up to the previous mark. A liposculpture of the back and/or flanks was initially performed, followed by a detachment of the suprafascial dermal-fat flap. The dermal-fat tissue resection was marked with an excess flap marking clamp, while checking the previous pinch test mark. The pinch test was performed without any deformation of the genitalia as described by Roxo9,10. Sutures were placed in two planes with nylon threads.
When the patient was changed to a dorsal decubitus position, we began liposuction of the anterior abdomen, with all the aspirated fat conditioned for the indicated lipografts and refinement of the final result. Subsequently, abdominoplasty was performed.
The patient was then placed in a dorsal decubitus position for either a “classic” or an “anchor” (depending on tissue surpluses and existing scars) abdominoplasty. An incision was made in the lower abdomen while taking special care of any detachment, which should be very restricted in the lateral areas, especially in cases where there was liposuction as described by Saldanha11. A plication of rectus abdominis muscles was performed with nylon threads; followed by an umbilicoplasty using the skin mini-circle technique12, caudal traction of the abdominal flap, resection of surplus dermal-fat tissues, and approximation of the planes by means of Baroudi’s adhesion points13. Vacuum drains were routinely used and externalized by minimal incisions in the inguinal folds. Sutures were placed according to the anatomical planes with nylon threads.
Next, an incision was performed in the crural region at the inguinal area up to the subgluteal fold (which could extend to the sides of the thigh in cases of large riding breeches) and added to the vertical incision on the inner thighs (which extended to the knee joint if required), followed by suprafascial detachment, and resection of the dermal-fat surplus (determined by the pinch-test maneuver and confirmed with the flap withdrawal marking clamps). Sutures were then placed according to the anatomical planes with nylon threads. Particular attention was paid not to deform the genitalia while performing a cranial traction of the flaps and their anchorage. The deformity was verified with the thighs in adduction and abduction positions.
Upper body:
A solution consisting of saline (1: 300,000) with 2 ampoules of 2 % lidocaine without a vasoconstrictor was applied to all the areas to be operated.
A torsoplasty was performed with the patient in the ventral decubitus position, in the indicated cases. The pinch test maneuver was performed and any surplus tissue from the upper back was resected, while trying to place scars on the breast topography when possible (in the case of female patients). It should be remembered that dorsal scars in the lower body tend to rise, and upper dorsal scars tend to lower in the medium-term post-operative period.
The 360-degree incisions do not always cross the spine. In this region, especially in the lower dorsal area, the closure should be of very low tension, avoiding wound dehiscence.
The patient was moved to a dorsal decubitus position and breast markings were performed (using the Pitanguy technique). Mammoplasties during these procedures usually have indications for associated silicone implants, which were always placed retroglandular, respecting the principle of a “tight skin”. Round and textured silicone implants were routinely placed in the retro-glandular position and the rise of areola-papillary plaques was performed using the classic Pitanguy technique, with adaptations for flap ascension when necessary by the Skoog, Silveira Neto, or areola plug flap 10 technique. Next a brachioplasty was conducted, beginning with liposuction of the flaps in the suprafascial area, with an incision in the medial face of the arms, an anterior incision in the topography of the brachial sulcus, and a suprafascial detachment and resection of the dermal-fat surplus (verified by the resection marking clamp). Sutures were placed in the anatomical planes with nylon threads.
The brachioplasty incision may be continuous with the sub mammary sulcus incision, to develop bilateral upper back traction. Therefore, in cases where it is indicated, a 360-degree dorsal incision should be avoided.
Pre and post-operative care
Pre-operative
All the patients underwent laboratory tests (including serology for HIV, hepatitis B, and hepatitis C), cardiac and anesthesia evaluation prior to the procedure, with the approval of the bariatric surgeon to perform the restorative surgery.
Abdominal wall imaging (computed tomography or ultrasonography) was performed in all the cases to detect any change. In women who underwent upper level surgery, due to the mammary approach, a mammography ultrasound and mammography or a complete breast cancer prevention protocol was also conducted.
Post-operative
An intravenous infusion of 1 g of cefazolin was maintained every 8 hours for as long as the patient was hospitalized. After discharge, 500 mg of cefadroxil was prescribed orally every 12 hours for 7 days.
All the patients were strongly encouraged to ambulate early and were instructed to bend their legs and perform feet flexion and extension movements before the surgery. A subcutaneous infusion of 40 mg of enoxaparin, was started 10 to 12 hours after the surgery and was maintained for 6 more days, with one dose administered every 24 hours.
Surgical overalls were worn by the patients from the first post-operative day and maintained for at least 30 days. The use of isolated surgical bras was avoided post-mammoplasty with silicone implant to prevent of cranial mobilization of the implants.
The patients were allowed to take baths with running water on the first post-operative day. The surgical wounds were washed with bactericidal soap and 70% alcohol was applied until they were completely healed. The drains were maintained until the flow rate was less than 60 mL/24 hours.
All the patients were instructed not to expose themselves to the sun until all bruises were absorbed. After this period, they were allowed to perform all physical activities, including sun exposure.
In addition, a protein rich diet was prescribed.
After hospital discharge, the patient returned to the clinic weekly until all external stitches were removed and all the wounds healed. Outpatient reviews were performed 30, 90, 180, and 365 days post-surgery for reevaluation and photographic records.
RESULTS
Thirteen patients were analyzed, including 10 women and 3 men. Seven patients underwent only lower level surgeries and the other 6 patients underwent lower and upper surgeries (at different times).
The ages ranged from 30 to 59 years, with a mean age of 44 years. The weight loss after bariatric surgery ranged from 26 to 122 kg, with a mean of 66.11 kg. At the time the patients underwent post-bariatric surgery, the mean BMI of the patients was 26.15 kg/m2.
The mean surgery time on the lower level was 4 hours and 54 minutes. The mean operative time of upper level surgery was 4 hours and 5 minutes. The time elapsed between lower level and upper level surgeries ranged from 6 to 10 months, with a mean of 8 months.
If the procedures on each part of the body were performed separately and by a single team, the approximate times were:
4. Abdominoplasty: 4 hours
5. Mammoplasty: 3 hours and 20 minutes
6. Brachioplasty: 3 hours (1 hour and 30 minutes on each side)
7. Cruroplasty: 3 hours (1 hour and 30 minutes for each side)
The total time taken for all the procedures together was 13 hours and 20 minutes. Therefore, room hours (costs and security) of approximately 9 hours was saved in addition to a decrease in the amount of patient isolation time due to repeated surgeries.
Out of all the cases, 8 patients (61.53%) underwent abdominoplasty with a 360° incision, and 1 case was performed with a dorsal incision, 3 patients (23.07%) underwent a conventional incision and only 1 patient (7.69%) underwent anchor abdominoplasty. Out of all the patients who underwent upper-level surgeries, 4 patients (66.67%) underwent a cutaneous resection in the upper back.
For surgeries performed on the lower level, the weight of surgically resected tissue from the abdomen and back varied from 1.30 to 3.16 kg, with a mean of 2.37 kg. The weight of the resected tissue from both the thighs ranged from 0.240 to 0.504 kg, with a mean of 0.374 kg. For procedures performed on the upper level, the weight of the resected tissue from brachioplasty ranged from 0.280 to 0.882 kg, with a mean of 0.554 kg.
The lengths of hospital stay in all the cases did not exceed 24 hours and all patients were discharged a day after surgery.
Post-operative complications consisted of: 4 cases of small wound dehiscence in the thighs, 3 cases of small wound dehiscence in the abdomen, and 2 cases of wound dehiscence in the breasts; all were treated conservatively with serial dressings. Seromas were observed in 4 cases (2 cases in breasts and 2 in thighs) and were treated with punctures and lymphatic drainage. One patient had a clinically treated pulmonary thromboembolism. No surgical complications such as hematoma, flap necrosis and/or infection were observed (Table 1).
| Complications | Total | % |
|---|---|---|
| Breast dehiscence | 2 | 33,33 |
| Thigh dehiscence | 4 | 30,76 |
| Abdomen dehiscence | 3 | 23,07 |
| Breast seroma | 2 | 33,33 |
| Thigh seroma | 2 | 15,38 |
| Thromboembolism | 1 | 5,26 |
| Pulmonary |
A total of 92.30% patients reported that they were very satisfied with the final results obtained with no complaints regarding the size and position of scars. All the patients who underwent the two-level approach were satisfied with the surgery (Table 2).
| Satisfied | Dissatisfied | |
|---|---|---|
| 2 Levels (lower and upper) | 6 | 0 |
| 1 Level (lower) | 6 | 1 |
The results of the procedure were examined by an external evaluator and classified as great, good, fair, and poor. Out of the 6 cases that underwent lower and upper level procedures, 2 were classified as great, 3 as good and 1 as fair. Out of the 7 cases that underwent only to the lower level procedures, 5 were classified as great and 2 were good. Overall, according to the external evaluator, 53.84% of the cases had a great surgical result, 38.46% were good and 7.69% were fair. No results were classified as poor (Table 3).
| Lower + upper | Lower | Total | |
|---|---|---|---|
| Great | 2 (33.33%) | 5 (71.42%) | 7 (53.84%) |
| Good | 3 (50%) | 2 (28.57%) | 5 (38.46%) |
| Fair | 1 (16.67%) | 0 (0%) | 1 (7.69%) |
| Poor | 0 (0%) | 0 (0%) | 0 (0%) |
The images of the cases are given below (Figures 1 to 6).
Patients who underwent lower and upper body surgeries (Figures 7 to 13).
DISCUSSION
Abdominal adipose tissue resection was first described by Demar and Marx in 1890 in France. Kelly, in 1899, was probably the first to use the terminology “abdominal lipectomy”, where he performed a transverse dermal-adipose excision including the navel14,15.
A circumferential abdominal dermolipectomy was described initially by Somalo, in 194016. After decades, Carwell and Horton described a torsoplasty, which started a new era of technique enhancement, which also included suspension of gluteal ptosis.
Other authors such as Gonzáles-Ulloa, Baroudi, Pitanguy, among others, described their techniques for liposuction and developed advances for surgical demarcation to position the posterior scar properly 15,17.
With the advent of bariatric surgery, and an increase in demand for dermolipectomy, improved surgical techniques to adapt to new circumstances have been developed for post-operative bariatric surgery. Currently, multiple variations of surgical techniques are available to improve body contour14 which are indicated according to the case.
After bariatric surgery, patients have dermal-fat leftovers distributed in the anterior wall of the abdomen, and throughout the abdominal circumference. According to the literature, circumferential abdominoplasty has tremendous benefits, such as better distribution of the remaining tissues throughout the trunk circumference, decreased waist circumference, and suspension of the gluteal region.
Another advantage of this procedure is that the scar can be easily concealed by intimate clothing. However, in patients with a median longitudinal incision from conventional bariatric surgery or those with excess dermal fat in the epigastric region, an anchor abdominoplasty is indicated to obtain a satisfactory result18.
Complementary surgeries, such as mammoplasty, brachioplasty, cruroplasty, flankplasty, and torsoplasty, in addition to liposuction, are necessary to improve body contour and obtain a satisfactory surgical result7,8.
This study included 13 ex-obese patients who underwent post-bariatric surgery. In half of the patients, both the upper and lower levels were treated and, in the other half, only the lower level. This study was composed of young men and women, with a mean age of 44 years and a mean BMI of 26.15 kg/m², similar to that found in literature1,19,20.
Complications were related to the patient’s general condition and the extent of the procedure, which were classified into major and minor21 complications. In this study, the most prevalent complications were wound dehiscence (mainly in the thighs) and seroma, and were treated in an outpatient setting, with dressings, drainages, or punctures. There was one case of pulmonary thromboembolism, which was treated with low molecular weight heparin, without any complications.
Several authors have reported higher complication rates, especially for torsoplasty or abdominoplasty, with a complication rate around 35%15,18,22,23. The incidences of major and minor complications in this study were consistent with literature15,18,22,23.
In this study, the mean surgery time for the lower level was 4 hours and 54 minutes and 4 hours and 5 minutes for the upper level. Baroudi defined as surgical time limit as 360 minutes. Surgical procedures that exceed this time limit are associated with post-operative complications24.
A reduction in the surgical time requires a high level of coordination of the surgical team, since it allows multiple procedures to be performed simultaneously by surgical teams working separately on different areas of the body .
If the procedures on each body part were performed at separate times and by a single team, the surgery would have lasted a total of 13 hours and 20 minutes (abdominoplasty: 4 hours; mammoplasty: 3 hours and 20 minutes; brachioplasty: 3 hours; cruroplasty: 3 hours). Therefore, approximately 9 hours room hours were saved (costs and security), in addition to a decrease in the patient’s isolation period due to repeated surgeries.
The patients had a satisfaction level of 92.30% at the post-operative follow-up. This percentage demonstrates a high degree of satisfaction, similar to data found in literature when comparing similar techniques of post-bariatric plastic surgery22. Similarly, we observed a higher percentage of satisfaction in the patients who underwent the two-level approach, similar to literature, which revealed that body contouring surgery that addresses several segments of the body generated a higher satisfactory surgical result due to body harmonization when seen in its totality7,8.
The analysis of the results by the external evaluator, 53.84% of the cases presented a surgical result considered great, 38.46% good and 7.69% regular. No results were scored as bad. Therefore, it revealed a rate of 92.30% of the cases classified as good or great, demonstrating a high degree of approval of surgical results.
CONCLUSION
In order to have a good functional and aesthetic result, a pre-established routine and a systematic procedure and sequential steps are important.
Additionally, we emphasize the need for a well-trained and capable surgical team, made up of several members, all following the same surgical technique, so that the process can be optimized with a shortened surgical time, minimizing consequent complications.
Satisfactory results obtained with low complication rates, minimal patient absence from normal life, better aesthetic results, and much lower costs proves the applicability of the routine of Plastic Surgery at Daher Hospital in post-bariatric patients.
COLLABORATIONS
|
JCD |
Analysis and/or data interpretation, final manuscript approval, realization of operations and/or trials. |
|
ACC |
Conception and design study, writing - original draft preparation. |
|
MCC |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
BEP |
Analysis and/or data interpretation, realization of operations and/or trials. |
|
GCS |
Conception and design study, writing - original draft preparation. |
|
LDPB |
Conception and design study, writing - original draft preparation. |
|
RCSD |
Conception and design study, writing - original draft preparation. |
|
LMCD |
Conception and design study, writing - original draft preparation. |
REFERENCES
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766-81. PMID: 24880830 DOI: https://doi.org/10.1016/S0140-6736(14)60460-8
2. Pinheiro ARO, Freitas SFT, Corso ACT. Uma abordagem epidemiológica da obesidade. Rev Nutr. 2004;17(4):523-33. DOI: https://doi.org/10.1590/S1415-52732004000400012
3. Brasil. Ministério da Saúde. VIGITEL Brasil 2013. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2013. Brasília: Ministério da Saúde; 2014. Disponível em: https:// biavati.files.wordpress.com/2014/05/vigitel-2013.pdf
4. Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197-209. PMID: 16198769 DOI: https://doi.org/10.1016/S0140-6736(05)67483-1
5. Chang SH, Stoll CR, Colditz GA. Cost-effectiveness of bariatric surgery: should it be universally available? Maturitas. 2011;69(3):230-8. PMID: 21570782
6. Bradley D, Conte C, Mittendorfer B, Eagon C, Varela JE, Fabbrini E, et al. Effects of gastric bypass and adjustable gastric banding on glucose homeostasis. Journal of Clinical Investigation. 2012:112.
7. Kitzinger HB, Abayev S, Pittermann A, Karle B, Bohdjalian A, Langer FB, et al. After massive weight loss: patients’ expectations of body contouring surgery. Obes Surg. 2012;22(4):544-8. DOI: https://doi.org/10.1007/s11695-011-0551-6
8. Al-Hadithy N, Mennie J, Magos T, Stewart K. Desire for post bariatric body contouring in South East Scotland. J Plast Reconstr Aesthet Surg. 2013;66(1):87-94. DOI: https://doi.org/10.1016/j.bjps.2012.08.041
9. Roxo CDP, Pinheiro O, Almeida D. Abdominoplastia Multifuncional. Rev Bras Cir Plást. 2004;19(3):64-74.
10. Roxo CDP, Roxo ACW, Roxo CW. Coxoplastia oblíqua em pacientes após grandes perdas ponderais. Rev Bras Cir Plást. 2012;27(1):119-23. DOI: https://doi.org/10.1590/S1983-51752012000100020
11. Saldanha OR. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;21(6):518- 26. DOI: https://doi.org/10.1067/maj.2001.121243
12. Daher JC, Benedik A, Faria CADC, Amaral JDG, Rodrigues Neto JN, Cosac OM, et al. Umbilicoplastia: experiência com a técnica do minicírculo de pele. Rev Bras Cir Plást. 2011;26(2):302-5.
13. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41. PMID: 19328174 DOI: https://doi.org/10.1016/S1090-820X(98)70073-1
14. Kelly HA. Excision of the flat abdominal wall lipectomy. Surg Gynec Obstet. 1910;10:229-31.
15. Cintra Junior W. Abdominoplastia circunferencial simples e composta: evolução técnica, experiência de 10 anos e análise das complicações [Tese de doutorado]. São Paulo: Universidade de São Paulo, Faculdade de Medicina; 2014.
16. Somalo M. Dermolipectomia circular del tronco. Semana Med. 1940;47:1435.
17. Baroudi R. Cirurgia do contorno corporal. Rio de Janeiro: Indexa Editora; 2009.
18. Modolin M, Cintra W Jr, Gobbi CI, Ferreira MC. Circumferential abdominoplasty for sequential treatment after morbid obesity. Obes Surg. 2003;13(1):95-100. DOI: https://doi.org/10.1381/096089203321136665
19. Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, et al.; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Cholesterol). National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 30 million participants. Lancet. 2011;377(9765):578-86. DOI: https://doi.org/10.1016/S0140-6736(10)62038-7
20. CDC. [Cited 2011 Mar 25]. Available from: http://www.cdc.gov/PDF/Frequently_Asked_Questions_About_Calculating_Obesity-Related_Risk.pdf
21. Arthurs ZM, Cuadrado D, Sohn V, Wolcott K, Lesperance K, Carter P, et al. Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am J Surg. 2007;193(5):567-70. DOI: https://doi.org/10.1016/j.amjsurg.2007.01.006
22. Cintra Junior W, Modolin M, Gobbi CIC, Gemperli R, Ferreira MC. Abdominoplastia circunferencial em pacientes apó s cirurgia bariátrica: avaliação da qualidade de vida pelo critério adaptativo. Rev Bras Cir Plá st. 2009;24(1):52-6.
23. Manahan MA, Shermak MA. Massive panniculectomy after massive weight loss. Plast Reconstr Surg. 2006;117(7):2191-7.
24. Baroudi R. A seguranç a nas cirurgias estéticas combinadas. Rev Bras Cir Plá st. 2010;25(4):581-2.
1. Hospital Daher Lago Sul, Brasília, DF,
Brazil.
Corresponding author: José Carlos Daher, Quadra 7, SHIS QI 7 conjunto F, Lago Sul, Brasília, DF, Brazil. Zide Code: 71615-660. E-mail: daher@hospitaldaher.com.br
Article received: April 02, 2018.
Article accepted: April 16, 2019.
Conflicts of interest: none.


























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter