

Case Reports - Year 2000 - Volume 15 -
Giant Hemangioma of the Hand in a Child - Case Report
Hemangioma Gigante da Mão em Criança - Relato de Caso
ABSTRACT
The authors discuss a case of hand giant hemangioma in a child, surgically treated with success. The frequency of this type of tumor in children, and the therapeutic options recommended by diffirent authors are discussed.
Keywords: Giant hemangioma; hand; child
RESUMO
Os autores descrevem um caso de hemangioma gigante na palma da mão de uma criança tratada cirurgicamente com bom resultado e discutem a freqüência deste tumor em crianças, assim como as condutas propostas por diferentes escolas.
Palavras-chave: Hemangioma gigante; mão; criança
For many reasons, palmar tumors are a ehalienge for the surgeons. The hand is a highly specialized structure, and represents a relationship tool with both the enviranment and other people. The hand is essential to virtually all human activities. The hand's complex anatomy results from the presence of several functional structures within a small area (tendons, nerves, and blood vessels). In children, care must be taken not to damage these structures during a surgical procedure, since such anatomical structures are difficult to identify, and any damage ean greatly affect the patient's quality of life.
In 1940, Watson and Me Carthy(1) reported that hemangiomas account for 25% of all hand tumors. In 1994, Kransdorf(2) published a study on benign tumors in which hemangiomas represented 13% of hand tumors in people aged from zero to fifteen. In 1996, Mendel and Louis(3) carried out a study on vascular tumors in the upper limbs, showing thar the hemangioma is the fourth more frequent hand vascular tumor.
Other authors, such as Palmierí(4), Glanz(5), Weisman(6) and Milner(7) published studies on the surgical treatment for hand hemangiomas. In 1986, Milner and Sykes(7) published a paper describing the surgical approach of hand diffuse cavernous hemangiomas. The largest hemangioma described in this paper had a diameter of 6 x 7 cm.
In the present study, the authors report the case of a ten-year-old female patient with a palmar giant hemangioma. The surgical approach and postoperative course of the disease are described and the results are compared with those of other authors.
CLINICAL CASE
S.M.O., a 10-year-old female patient, had a soft tissue tumor with the following characteristics: almost circular shape, diameter of 10 cm and height ranging from 4 to 5 cm. The tumor extended throughout the palm of the left hand, invading the second imerdigital space. Her mother reported that the child presented a "tiny spot" at the palm of the left hand at birth (Figs. 1 and 2).
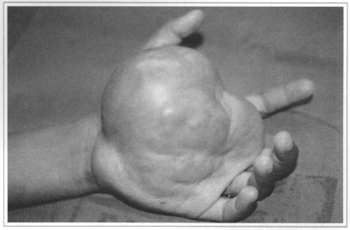
Fig. 1 - Preoperative aspect.
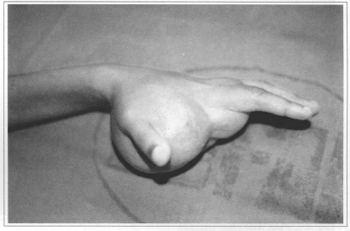
Fig. 2 - Preoperative aspect.
The physical examination showed a flexion disability of metacarpophalangeal joints and a limited flexion of proximal and distal interphalangeal joints, both affecting all fingers, except for the thumb. The X-ray showed dysplasia of the metacarpal head of all fingers, except for the thumb; subluxation of the second finger's metacarpophalangeal joint due to tumor invasion; and dystrophic microcalcifications scattered throughout the tumor. Angiography showed a uniform invasion into the palm of the left hand (Fig. 3).
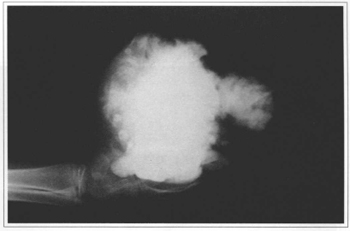
Fig. 3 - Radiological aspect. Profile.
The surgical procedure was carried out under general anesthesia. First, a tourniquet was used to temporarily stop blood flow and the residual blood was aspirated with a syringe. After skin incision on the palm of the hand along the cleavage lines, exposure of surface planes, and identification of hand structures, a careful dissection of the dark brown mass was performed, releasing tendons, nerves, and the ulnar artery was identified (Fig. 4). Tumor resection was completed with success. Hypotrophy of palmar interosseous muscles was observed during surgery. A Penrose drain was placed and the wound was closed with 5/0 mononylon. A compression bandage was applied and the hand was kept raised. A large hematoma appeared one day after surgery. It was drained and hemostasis was reviewed (Fig. 5). The patient complained of severe pain two days after surgery and a local edema was present. On the following day, she presented phlyctenas on the left hand. Passive physical therapy was then started. Eight days after surgery, the edema was greatly decreased and active physical therapy could be started.
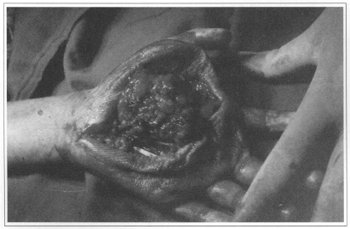
Fig. 4a - Intraoperative period.
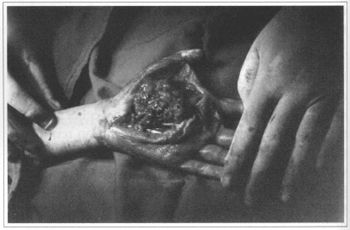
Fig. 4b - Tumor dissection.
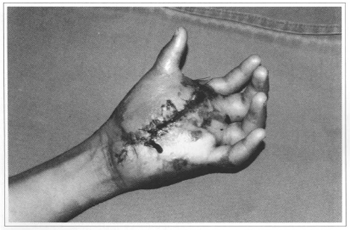
Fig. 5 - One day after surgery.
Ten days after surgery, the patient was discharged presenting a good joint flexion, except for rhe second finger metacarpophalangeal joint, which presented dysplasia of the capsule and ligaments (Fig. 6). The microscopic examination diagnosis is Cavernous Hemangioma of the Hand.
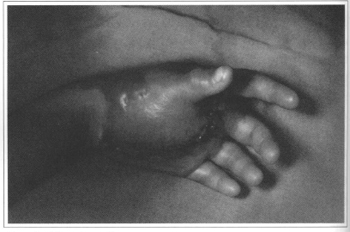
Fig. 6 - Ten days afrer surgery.
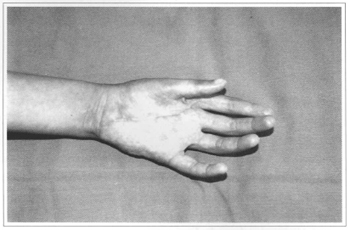
Fig. 7 - Sixty days after surgery.
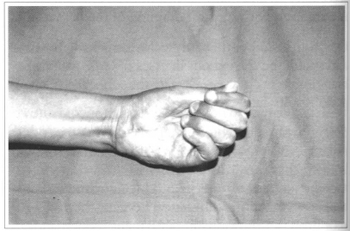
Fig. 8 - Sixty days after surgery.
DISCUSSION
Hemangioma therapy is a hotly disputed issue, since a great percentage of the tumors spontaneously shrink or regress. The therapy is often delayed in the hope that the tumor disappears. In 1888, Duncan(8)was one of the pioneers to report spontaneous regression in more than half of the mixed-type hemangiomas.
Complications, such as ulcers, necrosis, secondary infection, and hemorrhage, can appear when the appropriate therapy is delayed. As for hand hemangiomas, tumor growth may lead to functional sequels, with limb amputation in the more severe cases. In several publications, Curado(9) has reported a 100% spontaneous involution of fragiform-type hemangiomas(4), which is seen in a few cases of cavernous hemangiomas.
In 1959, Weisman(6) determined that the hemangioma involution is not related to the tumor site and size and is independent of whether it is present at birth or not.
Several treatments have been suggested, including cryotherapy, intralesional injection of sclerosing agents and irradiation alone or in combination, with variable results. The use of sclerosing agents in the hand may produce fibrosis while irradiation and cryotherapy are not effective in treating this type of lesions due to their limited effects and because malign transformation is possible. In 1969, Glanz(5) reported that nonsurgical techniques play a small role, if any, in the treatment of cavernous hemangioma. The best results are obtained by surgical excision of the lesion, which is the first-choice therapy.
The cavernous hemangioma of the hand is generally larger than it looks like, once it tends to invade into deep tissue. Difficulties in the management of this type of diffuse vascular malformations have been extensively reported and their surgical resection requires a careful dissection. Serious complications are not uncommon, especially with preoperative embolization recommended by some authors to decrease bleeding during excision. Surgery should be considered in individual cases, specially when the tumor is large or a functional limitation exists due to the high recurrence rate reported by some authors. Weisman and Milner(6) recommend the partial resection to alleviate symptoms, emphasizing the balance between aggressive surgical resection and prevention of functional structures.
In our case, a careful surgical resection was indicated due to the great palmar deformity and left hand functional limitation caused by the progressive tumor growth. The fact that anatomical structures are smaller in a child, and occupy a limited area is noteworthy. All measures required to preserve vital structures were taken with satisfactory esthetical and functional results.
Caroli and Zanasi(10)(1991), among others, reported that surgical treatment is the procedure of choice in cases of large hemangiomas of the hand , emphasizing the importance of a careful dissection and preservation of vital structures, with a low relapse rate.
Daily postoperative follow-up is important to early identify and treat complications, as illustrated by the present case. Three days after surgery, skin suffering secondary to a hematoma was noticed and satisfactorily resolved with surgical draining of the hematoma.
Our conclusion is that surgical treatment is possible and should be carried out in cases of large palmar hemangiomas in children. Despite the surgical challenge, good results can be expected.
Surgeons should avoid reintervention to avoid tissue necrosis, except when there is a strong indication. We believe that surgical treatment is the first-choice therapy in cases of tumors producing marked symptoms and functional limitation because the rapid tumor growth can results in permanent sequels and, in most severe cases, amputation.
REFERENCES
1. WATSON WL, Mc CARTHY WD. Blood and lymph vessel tumors. Surgery, Gynecology and Obstetrics. 1940;71:569-572.
2. KRANSDORF MJ, JELINEK S, MOSER P. Soft-tissue masses: diagnosis using MR imaging. AJR. 1989;153:541-547.
3. MENDEL T, LOUIS D, ARBOR A. Major vascular malformations of the upper extremity: Long-term observation. J. Hand Surg. 1997;22A:302-306.
4. PALMIERI TJ. Subcutaneous hemangiomas of the hand. J. Hand Surg. 1985;10A:135-139.
5. GLANZ S. The surgical treatment of cavernous hemangiomas of the hand British J. of Plast. Surg. 1969;22:293.
6. WEISMAN P. Blood vessel tumors of the hand. Plast Reconstr. Surg. 1959;23:175-186.
7. MILNER RH, SYKES PJ. Diffuse cavernous haemangiomas of the upper limb. J. Hand Surg. 1987;12B:199-202.
8. DUNCAN J. Angioma and other papers. Edinburgh : Oliver & Boyd, 1900. p 13-4. Edited by James Hodson.
9. CURADO JH. Tratamento dos hemangiomas e linfangiomas. In: Mélega, Zanini, Psillakis. Cirurgia Plástica. São Paulo : Medsi, 1992. p. 177-89.
10. CAROLI A, ZANASI S, MARCUZZI M. Gli emangiomi della mano. Chir. Organi Mov. 1991(76);317-25.
I - Member of the Brazilian Society of Orthopedics
II - Member of the Brazilian Society of Plastic Surgery and Assistam Physician at Instituto de Cirurgia Plástica Santa Cruz
III - Member of the Brazilian Society of Plastic Surgery and Resident at Instituto de Cirurgia Plástica Santa Cruz
IV - Member of the Brazilian Society of Plastic Surgery and Resident at Instituto de Cirurgia Plástica Santa Cruz
Address for correspondence:
Jason César A. de Figueiredo, MD
R. Santa Cruz, 398
04122-000 - São Paulo - SP Brazil
Phone/fax: (55 11) 575-9863
Study performed at Instituto de Cirurgia Plástica Santa Cruz in São Paulo, SP, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter