

Original Article - Year 2019 - Volume 34 -
Effectiveness of Pessoa's universal technique for single marking in mastoplasty performed while training plastic surgeons
Avaliação do emprego da técnica universal para mastoplastias marcação única de Pessoa em um serviço de ensino de Cirurgia Plástica
ABSTRACT
Introduction: Reduction mastoplasty is still a challenging procedure for plastic surgeons. The Objective is to show the results of the treatment of different degrees of breast hypertrophy using Pessoa's single marking technique performed while training plastic surgeons.
Methods: A retrospective cohort of 95 patients underwent reduction mastoplasty using Pessoa's technique. The cohort included patients with breast ptosis, hypertrophy, gigantomastia, and/ or breast asymmetry. The procedures were performed by first-, second-, and third-year residents. The exclusion criteria were psychological disorders, morbid obesity, and/or indication for prosthesis implantation without skin and/or areola reduction. The analyzed factors were age, sex, final size, patient's degree of satisfaction, complications, and difficulties experienced by the residents in performing the surgery.
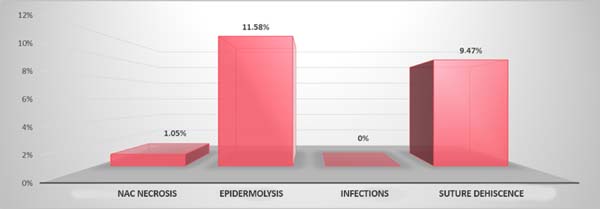
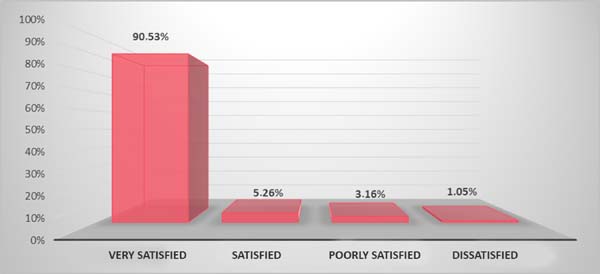
Results: All patients were women aged between 21 and 61 years. Of the patients, 90.53% reported being very satisfied; 5.26%, satisfied; 3.16%, poorly satisfied; and 1.05%, dissatisfied. The complications observed were necrosis of the nipple-areola complex (1.05%), epidermolysis (11.58%), and suture dehiscence (9.47%). The rate of difficulty experienced by the residents varied between 11.1% and 55.6%, depending on the step of the surgical procedure.
Conclusions: A high degree of satisfaction was reported by both the patients and residents. The results confirm the effectiveness of the technique while training residents.
Keywords: Mastoplasty; Plastic surgery; Breast; Body contour; Reconstructive surgical procedures
RESUMO
Introdução: A mamoplastia redutora é ainda um procedimento que desafia o cirurgião
plástico. O objetivo é demonstrar os resultados no tratamento de variados
graus de hipertrofia e ptose mamária utilizando-se a técnica de Marcação
Única, proposta por Pessoa, durante o treinamento de novos cirurgiões
plásticos.
Métodos: Coorte retrospectivo de 95 pacientes submetidas à mamoplastia redutora pela
técnica de Pessoa. Incluídas pacientes com ptose, hipertrofia, gigantomastia
e/ou assimetria das mamas. Os procedimentos foram realizados por residentes
do primeiro, segundo e terceiro ano. Como fatores de exclusão foram usados:
distúrbios psicológicos, obesidade mórbida e/ou pacientes com indicação de
implante de prótese sem redução de pele e/ou aréola. Foram avaliados a
idade, sexo, volume resultante, grau de satisfação, complicações e
dificuldades dos residentes para realização do procedimento cirúrgico.
Resultados: Todas as pacientes do sexo feminino, com idade entre 21 e 61 anos. 90,53% das
pacientes declararam-se muito satisfeitas, 5,26% satisfeitas, 3,16% pouco
satisfeitas e 1,05% insatisfeita. Como complicações, foram observadas
necrose de complexo areolopapilar (1,05%), epidermólise (11,58%) e
deiscência de sutura (9,47%). As dificuldades encontradas pelos residentes,
dependendo da etapa do procedimento cirúrgico, variaram entre 11,1% e
55,6%.
Conclusões: Verificou-se alto grau de satisfação tanto da parte das pacientes quanto dos
residentes envolvidos. Os resultados encontrados confirmam a efetividade da
técnica no treinamento de residentes.
Palavras-chave: Mamoplastia; Cirurgia plástica; Mama; Contorno corporal; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Reduction mastoplasty is a challenging procedure for plastic surgeons, although many techniques explaining how to perform it have been described in the literature1-5. The methods that are usually cited are empiric and mostly based on a surgeon’s intuition. Several techniques can be used to mark the skin, remove breast tissue, and perform a skin incision and resection, presenting their own advantages and disadvantages. Some can be applied only to small breasts or breasts with specific characteristics. However, none of the techniques can be applied in procedures for repairing breast morphological changes induced by different etiological causes.
The first surgical technique for breast reduction was developed by Paulus Aegenita, who in the 7th century, described in detail a procedure used to correct gynecomastia. More-reliable methods were described in the 1920s by Thorek, Aubert, and Passot. Improvements of the techniques were then reported by Schwartzmann and De Biesenberger in the 1930s. The technique described by Dr. Schwartzmann is still used nowadays.
The era of modern mastoplasty started in the 1960s with the works of Strombeck and Pitanguy, who published their technique based on the information reported by Lexer (1912), Kraske (1923), and Arié (1957). The contributions of Skoog (1963), in relation to the lateral dermal pedicle, and Mackissock (1972), concerning the popular procedure of areola reconstruction with bipedicled dermal flaps, are also worth mentioning6.
The surgical technique known as single marking (SM) was developed by Pessoa7 in 1989 at the Service of Plastic Surgery and Reconstructive Microsurgery of Walter Cantídio University Hospital of the Federal University of Ceará. The technique was presented at the competition for the Georges Arié award, and promoted by the Brazilian Society of Plastic Surgery, in 2009, where it received honorable mention.
This technique was developed by taking into consideration breast morphology, known worldwide to be conical, and its anatomical relationship with the chest wall. Therefore, the development of this method was based on the assumption that when operating a breast, the surgeon aims to achieve a cone-shaped breast in conditions in which the patient’s breast has total or partial loss of integrity. The technique is based on anatomical and geometric principles, which could be applied to all types of procedures for maintaining, repairing, or reconstructing the breast. This method can be used to treat all types of breasts (small, medium, large, and giant).
When planning to use this technique, the size of the breast must first be determined. According to the International System of Units, cubic meter is used as the standard volume unit. One cubic meter (1 m³) corresponds to a volume of 1,000 L. Therefore, breasts can be deemed small or large just by observing and calculating the ratio between the space they occupy on the chest divided by the space they occupy on the abdomen.
The Lalardrie and Jouglard classifications8 were also used. According to the authors, breast size could be represented by 5 categories based on the height (base of the breast) and frontal projection of the breast. Thus, breasts are divided as follows: having 1. an ideal volume (250-300 cm3), 2. moderate hypertrophy (400-600 cm3), 3. significant hypertrophy (600-800 cm3), and 4. very significant hypertrophy (800-1000 cm3).
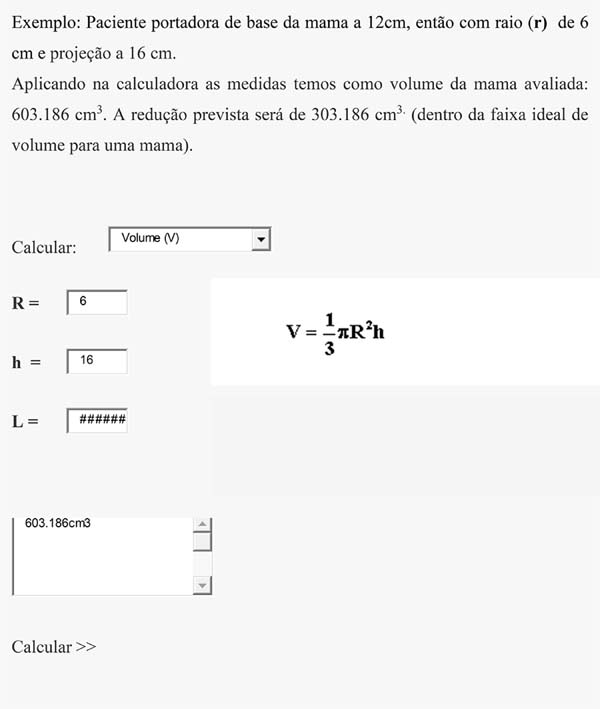
In this article, to be able to use breast volume as the measurement to define breast size, the Web Calculator9 was used preoperatively.
To calculate the breast volume that was surgically removed, Archimedes’ principle (Syracuse, Sicily, 287 BC)10,11 was applied intraoperatively.
The principle states that
a. All bodies immersed in fluid displaces a determined weight of liquid, whose volume is equal to the volume of the submerged body.
b. A body immersed in fluid “loses” a fraction of its weight that is equal to the weight of the fluid, which in turn is equal to the submerged volume of the object.
The principle was not used in the original technique of Pessoa7 but was applied in the present study. Moreover, on the basis of the above-mentioned statement, “any surgeon performing breast surgery aimed at repairing or reconstructing the breast must create, maintain, or reconstruct the cone shape regardless of any change that totally or partially compromises the breast anatomy.”
OBJECTIVE
The objective of this study was to demonstrate the effectiveness of the single marking technique proposed by Pessoa7 and performed while training new plastic surgeons. Herein, we report the results obtained in patients with different degrees of breast hypertrophy and ptosis who underwent the procedure.
METHODS
We conducted a retrospective and descriptive study based on the data collected from the medical records of women diagnosed as having breast ptosis, hypertrophy, gigantomastia, and/or breast asymmetry who underwent reduction mastoplasty.
Ninety-five patients were evaluated by analyzing and comparing the breast before and after surgery. The outcomes of the procedures performed between January 2014 and May 2017 by first-, second-, and third-year residents (R1, R2, and R3, respectively) were assessed.
This study was approved by the research ethics committee of the institution (opinion no. 69467517.5.0000.5045).
Surgical procedures were preceded by anamnesis, physical examination, laboratory tests, cardiac examinations, and screening of breast abnormalities by ultrasonography and mammography, conducted in patients aged >35 years.
The inclusion criteria were as follows:
1. Patients aged >21 years.
2. Patients with breast volumes > 300 cm3.
3. Patients whose main preoperative complaints were physical discomfort, bad posture, back pain, and premenstrual pain.
4. Patients with an outpatient postoperative follow-up of 1 year.
5. Patients who signed the informed consent form.
The exclusion criteria were as follows:
1. Patients with a body mass index (BMI) ≥ 28.
2. Patients with psychological disorders.
3. Patients with indication for prosthesis implantation without skin and/or areola reduction.
To evaluate the results, the opinions of both the surgeons (residents) and the patients were considered.
All the patients were monitored postoperatively, on dates scheduled in the outpatient clinic of the above-mentioned service. All the women were monitored for a period of 1 year, after which we collected the data to conduct this study.
The data analyzed were age, degree of patient satisfaction, appearance of the scars, volume of the resected breast tissue per surgery, type of resulting scar, and early and late complications.
On their visit at 1 year after the procedure, the patients were given a survey questionnaire, with topics listed in Chart 1 and referring to the quality of the treatment result, final volume, breast shape and ptosis, aesthetic quality of the nipple-areola complex (NAC), breast symmetry, scar quality, and degree of satisfaction (very satisfied, satisfied, poorly satisfied, and dissatisfied).
| 1. Degree of satisfaction with breast volume |
| a) Note 0 b) Note 1 c) Note 2 |
| 2. Degree of satisfaction with form and degree of ptosis |
| a) Note 0 b) Note 1 c) Note 2 |
| 3. Degree of satisfaction with CAP quality |
| a) Note 0 b) Note 1 c) Note 2 |
| 4. Degree of satisfaction with symmetry of breasts |
| a) Note 0 b) Note 1 c) Note 2 |
| 5. Degree of satisfaction with scar quality |
| a) Note 0 b) Note 1 c) Note 2 |
To calculate the volume of the cone and define the desired breast size preoperatively, we used the Web Calculator9 along with measurements of the radius of the breast base and its projection.
Figures 1 and 2 show how the measurements were taken. Figure 3 shows an example of the Web Calculator used to determine the volume of the straight cone.


The principle of Archimedes of Syracuse, Sicily, was used to determine the volume of the breast tissue removed intraoperatively, and the method used for this purpose is shown in Figure 4.
This principle was applied using 2 disposable plastic containers. One was filled with saline or distilled water. The resected tissue was placed in the other container, which presented the same capacity and was filled with fluid from the first container. This allowed the calculation of the volume of resected tissue, which was equal to the volume of fluid that remained in the first container.
The following observation criteria were used to establish the qualitative parameters of the results obtained from the mastoplasty procedures:
Ideal breast:
a. Conical shape, between the second and sixth intercostal spaces;
b. Ideal volume: 250-300 cm3;
c. Areolas with a diameter of 4 cm;
d. Distance between the upper limit of the areola and the sternal wishbone: ≤19 to 23 cm;
e. Distance between the midline and the lateral limit of the areola: 9 to 11 cm;
f. Breast symmetry;
g. NAC with everted nipples and preserved sensitivity;
h. Preservation of the ability to breastfeed;
i. Scars well positioned within the folds; scars that remain on the breasts should be barely visible.
In the present study, the responses given by the residents to the anonymous structured questionnaire were analyzed, including variables referring to the single marking technique proposed by Pessoa7, the self-assessment of the technique, and the received training. The responses to the survey were scored in an odd ordinal scale from 1 to 3, with a fourth negative option that did not measure the variable (Chart 2). In addition, the residents’ satisfaction with the final outcomes of the procedure was assessed using the same questionnaire as that given to the patients (Chart 1).
| 1. Demarcation |
| a) Average b) Few c) None |
| 2. Access to the gland and choice of pedicle |
| a) Average b) Few c) None |
| 3. Breast Modeling |
| a) Average b) Few c) None |
| 4. Symmetrization |
| a) Average b) Few c) None |
| 5. Breast Closure - Suture |
| a) Average b) Few c) None |
The variables and graphs were entered into Microsoft Excel.
The statistical analysis was performed using the EPIINFO 6.0 software.
RESULTS
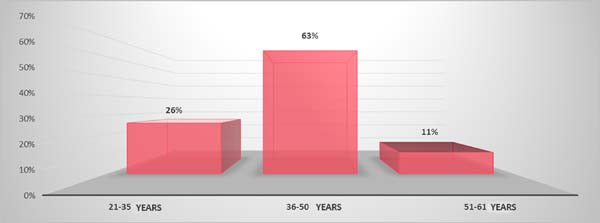
The patients’ ages ranged from 21 and 61 years (Graph 1).
The main postoperative complaints were physical discomfort (100%), bad posture, and back pain (81%).
The inferior and superior pedicle techniques were used in 93 (97.89%) and 2 (2.11%) of the patients, respectively.
The final breast volumes were calculated using the formula of the breast cone as previously described. The results ranged from 315 to 690 cm3.
The types of resulting scars were as follows: T-shaped (98.95%) and L-shaped (1.05%). The mean surgical time was 3 hours.
The observed complications were divided as follows:
a. Early complications: occurring up to 30 days after the procedure, and divided into epidermolysis (11.58%), suture dehiscence (9.47%), necrosis of the NAC (1.05%), and infections (0%; Graph 2).
b. Late complications: occurring during the patient follow-up period and divided into significant asymmetry (1.05%) and ptosis recurrence of Regnault grade ≤ II (5.26%). No other types of late complications were reported.
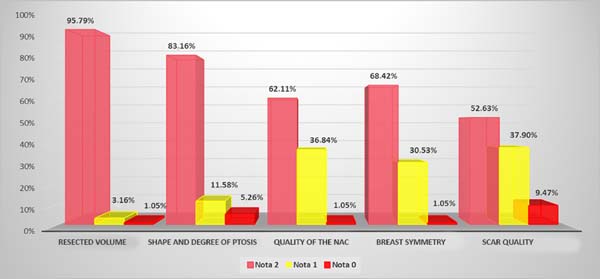
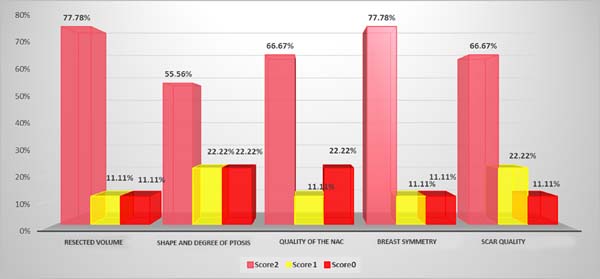
Graph 3 shows the degree of patient satisfaction with the procedure, which was assessed by scoring (2, 1, and 0) the following 5 aspects: resected volume, breast shape and degree of ptosis, quality of the NAC, breast symmetry, and scar quality.
The following results were obtained in relation to the degree of patient satisfaction: 90.53% of the patients were very satisfied; 5.26%, satisfied; 3.16%, poorly satisfied; and 1.05%, dissatisfied (Graph 4).
Among the 9 residents who answered the questionnaires to evaluate the difficulties experienced during the surgical procedure, 3 were R1 (33.3%), 3 were R2 (33.3%), and 3 were R3 (33.3%); 6 were men (66.7%), and 3 (33.3%) were women.
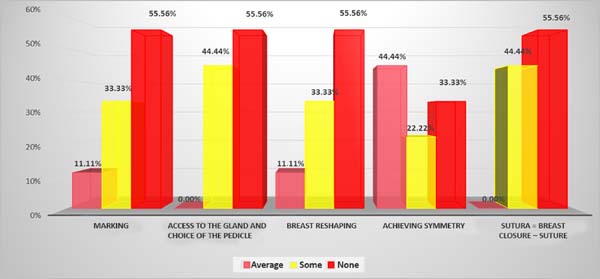
Among the residents, 11.11% reported intermediate difficulties in the surgical marking step (1 R1); 33.33%, some difficulties (2 R1 and 1 R2); and 55.56%, no difficulties (2 R2 and 3 R3).
Regarding the access to the gland and the choice of pedicle, 44.44% reported some difficulty (3 R1 and 1 R2) and 55.56% reported no difficulty (2 R2 and 3 R3).
Regarding breast reshaping, 11.11% of the residents reported intermediate difficulties (1 R1); 33.33%, some difficulty (2 R1 and 1 R2); and 55.56% (2 R2 and 3 R3), no difficulty.
Regarding breast symmetry, 44.44% of the residents reported intermediate difficulty (3 R1 and 1 R2); 22.22%, some difficulty (2 R2); and 33.33%, no difficulty (3 R3).
Regarding breast closure, 44.44% of the residents reported some difficulty (3 R1 and 1 R2); and 55.56% (2 R2 and 3 R3) no difficulty (Graph 5).
The degree of resident satisfaction with the results of the procedure was assessed by scoring the 5 aspects (on a scale of 2, 1, and 0) shown in Graph 6.
Example cases are shown in Figures 5 and 6.
DISCUSSION
Reduction mastoplasty is one of the most common surgical procedures performed by plastic surgeons12. When choosing the type of procedure, one of the surgeon’s major concerns is safe transposition of the NAC and achieving a breast cone that meets the patient’s expectations. Advances in the understanding of vascular anatomy since the 1980s, in particular, allowed plastic surgeons to plan a safe transposition of the NAC on the following 4 pedicles with axial extensions: superior, inferior, mediolateral, and lateral.
Mastering the single marking technique allows the surgeon to safely transpose the NAC within the indication and needs of each patient, which is one of the major advantages of using the method.
The concept of single marking broke the paradigm that no universal technique has been established for breast surgery, as its principles can be applied to all types of breast procedures, provided that the intention is to maintain, repair, or reconstruct the breast cone. From a mathematical point of view, this technique respects the individuality of patients.
The definition of an ideal outcome could be easily modified by establishing, when planning the surgery, whether the resulting cone will be maintained, reduced, or increased with the removal of the skin or breast tissue or with the insertion of silicone implants.
Another important point is the possibility of not making a prior skin removal, which is unnecessary before the planned cone is defined. This technical feature can define the type of resulting scar as circumferential, racket-shaped, L-shaped, T-shaped, or anchor-shaped. Many articles in the literature describe how to create the cone with different scar results.
The possibility of using mathematical concepts allows obtaining completely predictable results, especially when associated with glands and skin reshaping, which is performed in distinct stages. This practice prevents errors such as the removal of excess glands and skin, which cannot be corrected afterward.
An individualized approach is used for each patient.
Unnecessary scars are prevented, and planning a skin pocket can avoid the occurrence of asymmetries.
Another important point to consider is the infiltration of anesthetic and adrenaline solutions to aid in reducing bleeding, which spares the patient from complications, reduces the surgical time without increasing the incidence of bleeding or hematoma, and provides a low-risk postoperative period with lower risk of infection.
The technique does not involve resections below the NAC, which should be located 10 cm above the breast tissue.
In this study, the incidence of NAC necrosis caused by procedures performed to correct gigantomastia (very significant hypertrophy) was up to 85-90%, which is in agreement with the reports in the literature13-15. In the present study, the NAC viability was 98.95%.
A high degree of patient satisfaction (90.53%) was observed, with outcomes rated between satisfactory and excellent, similar to the findings published by Ronconi et al.16, Cho et al.17 and Rohrich et al.18, who used well-established surgical techniques among the national and international communities of plastic surgery.
In the study that described the opinions of the plastic surgery residents regarding the training and self-learning of the surgical technique, the technique was highly favorable, presenting a short learning curve.
Although the residents were highly or moderately satisfied with the outcomes of the procedures performed, they all identified several aspects they wished to improve in relation to breast surgery training/learning. This finding highlights the importance of anonymity in questionnaires to prevent unreliable results.
The above-mentioned observations were not made by the R3 group.
Pessoa’s single marking technique is a recently developed method; therefore, its increasing use by surgeons and improved description will undoubtedly lead to its evolution and better outcomes.
CONCLUSION
In this study, the use of the single marking technique proposed by Pessoa7 was highly effective.
A high degree of satisfaction was reported both by the patients and the residents. The outcomes were rated as good and excellent. The position and shape of the scars were satisfactory, and their sizes were reduced to minimum.
Moreover, the results presented herein confirm that the technique is effective for training residents, proving to be an easy-to-learn, safe, and predictable method.
COLLABORATIONS
|
SGPP |
Analysis and/or data interpretation, data curation, formal analysis, methodology, visualization. |
|
AM |
Analysis and/or data interpretation, conception and design study, data curation, final manuscript approval, methodology, project administration, writing - original draft preparation. |
|
JADL |
Conception and design study, final manuscript approval, project administration, supervision. |
REFERENCES
1. Schartzman E. Die technik der mammaplastik. Der Chirurg. 1930;2:932.
2. Ariê G. Nova técnica em mastoplastia. Rev Latinoam Cir Plast. 1957;3:22-8.
3. Strombeck JO. Reduction mammaplasty. In: Grabb WC, Smith JW, eds. Plastic surgery. Boston: Little, Brown and Co; 1968.
4. Pitanguy I. Hipertrofias mamárias: estudo crítico da técnica pessoal. Rev Bras Cir. 1966;56:263.
5. Skoog T. Plastic surgery: new methods and refinements. Philadelphia: Saunders; 1974.
6. Neligan PC, Grotting JC. Cirurgia Plástica: Técnicas de CirurgiaEstética de Mama. Rio de Janeiro: Elsevier; 2015. p. 153-64.
7. Pessoa SGP, Dias IS, Pessoa LMGP. Mastoplastia com marcação única: uma abordagem pessoal. Rev Bras Cir Plást. 2009;24(4):509-20.
8. Lalardrie JP, Jouglard JP. Plasties Mammaries pour Hypertrophie et Ptose. Paris: Masson; 1973.
9. WebCalc. Área/Volume do Cone Reto. [acesso 2018 Out 2]. Disponível em: http://webcalc.com.br/Matematica/form/cone_reto
10. Guimarães ABAB. O velho princípio de Arquimedes. Cad Bras Ens Fís (Florianópolis). 1999;16(2):170-5.
11. Martins TF, Rodrigues FL, Malafaia PAM, Cruz FAO. Princípio de Arquimedes: do treinamento virtual a execução experimental. Vivências. 2015;11(21):199-205.
12. Cammarota MC, Camara Filho JPP, Daher JC, Benedik Neto A, Faria CADC, Borgatto MS, et al. Aplicação estética e reconstrutora da mamoplastia com pedículo areolado. Rev Bras Cir Plást. 2014;29(2):237-42.
13. Bostwick J. Plastic and Reconstructive Breast Surgery. St Louis: QMP; 1990. DOI: https://doi.org/10.1097/00006534-199104000-00034
14. Hefter W, Elvenes OP, Lindholm P. A retrospective quantitative assessment of breast sensation after lateral pedicle mammaplasty. Br J Plast Surg. 2003;56(7):667-73. DOI: https://doi.org/10.1016/S0007-1226(03)00308-4
15. Graf R, Biggs TM. In search of better shape in mastopexy and reduction mammoplasty. Plast Reconstr Surg. 2002;110(1):309-17. DOI: https://doi.org/10.1097/00006534-200207000-00053
16. Ronconi RC, Vieira FA, Boechat CEJ, Nunes PSMR, Aboudib JHC, Castro CC. Estudo Retrospectivo de 730 Pacientes Submetidas a Mamaplastia Redutora. Rev Bras Cir Plást. 2004;19(2):58-62.
17. Cho BC, Yang JD, Baik BS. Periareolar reduction mammoplasty using an inferior dermal pedicle or a central pedicle. J Plast Reconstr Aesthet Surg. 2008;61(3):275-81. PMID: 18037359 DOI: https://doi.org/10.1016/j.bjps.2007.10.024
18. Rohrich RJ, Gosman AA, Brown SA, Reisch J. Mastopexy preference: a survey of board-certified plastic surgeons. Plast Reconstr Surg. 2006;118(7):1631-8. PMID: 17102738 DOI: https://doi.org/10.1097/01.prs.0000248397.83578.aa
1. Universidade Federal do Ceará, Fortaleza, CE,
Brazil.
2. University of Belgrade, Belgrado,
Sérvia.
Corresponding author: Salustiano Gomes de Pinho Pessoa, Avenida Parnamirim,1001 - Cs 05, Centro, Eusebio, CE, Brazil. Zip Code 61760-000. E-mail: salustianogpessoa@gmail.com Corresponding author: Aleksandra Markovic, Avenida Beira Mar, 4260, Praia de Mucuripe, Fortaleza, CE, Brazil. Zip Code 60165-121. E-mail: 19quepasa19@gmail.com
Article received: July 05, 2018.
Article accepted: April 21, 2019.
Conflicts of interest: none.



















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter