

Case Reports - Year1998 - Volume13 - Issue 2
Malignant Hyperthermia Syndrome after Reduction Mammaplasty - Case Report
Síndrome de Hipertermia Maligna após Mamoplastia Redutora - Relato de Caso
Malignant hyperthermia (MH) is a hypermetabolic condition, which occurrence is rare. It has an incidence of 1:15000 anesthesias in children, and 1:50000 in adults. The disease is more common in men, during the third decade of life. There is no racial preference.
This hypermetabolic condition is characterized by: tachycardia, unstable blood pressure, rigidity of masseters (in 25% of the cases it is not noticed; they are the non rigid forms), hyperthermia (rapid rise in body temperature, up to 1º C, in 5 minutes, reaching 42º, 43º C), tachypnea, aerobic and anaerobic hypermetabolism (lactate and pyruvate), cyanosis, sudoresis or extremely dry skin.
It is believed to be a skeletal muscle disorder, an autosomal dominantly and multifactorially inherited condition, broken out by anesthetic agents (mainly succinylcholine and halothane) and stress.
The main defect of the muscle fiber is the difficulty of the sarcoplasmic reticulum (SPR) in recapturing the calcium, which was released during muscular contraction It is maintained, thus, a contracture condition, with following heat production, oxygen consumption, lactic acid production (as a result of anaerobic metabolism) and finally, muscular necrosis (XAVIER, 1984; MILLER, 1986; SABISTON, 1991; CIVETTA 1992).
The diagnosis has been determined through laboratory and clinical results, that include respiratory and metabolic acidosis (PaCO2 levels higher than 55 mmHg arc significative and of bad prognosis, that is fulminant MH), hypercalcemia, hyperkalemia, myoglobinuria and enzymes increase (mainly lactic dehydrogenase, creatine phosphokinase and aldolase).
The differential diagnosis must be gotten with hyperthyroidism, pheocromocytoma, malignant neuroleptic syndrome and infectious situations.
The treatment consists in interrupting the use of anesthetics, dantrolene, sodium bicarbonate, cooling of gastric, vesical and rectal cavities, urinary debit monitor attendance, steroids, laboratorial attendance of the coagulation factors for detection of disseminated intravascular coagulation.
The mortality rate is 70% right after the establishment of this situation. In cases of survival the late complications are cerebral edema, adult respiratory distress syndrome, acute renal failure (by myoglobinuria), hemolysis and disseminated intravascular coagulation (COLLINS, 1978; XAVIER, 1984; BLITT, 1990).
We will report the occurrence of a case, confirmed soon after the surgery conclusion (reduction mammaplasty). It was treated with success, utilizing dantrolene.
CASE REPORT
SLL, white female, 28 years old, 61 kg, ASA I, was interned for a reduction mammaplasty accomplishment. She was known to have had previous convulsive crisis, at 13 and 18 years old; it was broken out because of stress; several relatives present the same occurrence. Regarding the previous anesthetics, it was noticed peridural for Caesarian operations 6 and 5 years ago, with no intercurrences. Physical exam was considered normal. Pre-operative exams were considered normal. Anesthesia was accomplished, utilizing etomidate, fentanyl citrate, succinylcholine ch1oride and halothane. Mammaplasty was accomplished, using Pitanguy's technique, in 21/2 hours, with approximately 700 ml of bleeding, calculated by bandages weighing. Thirty minutes after the anesthesia was ended the patient presented hyperthermia (axillar temperature 38.8º C) so she was treated with intravenous dipyrone. A few minutes later, she was confused, her pulse rate was 140 and the axillar temperamre was 40º C. The following procedures were taken: cardiac monitor attendance, oxygen catheter, intravenous icy sorus, alcohol bandages on thorax, abdomen and axilla, gastric and vesical washing, utilizing icy sorus, hydrocortisone and cephalosporine. The following exams were accomplished: arterial gasometry, hemoglobin, hematocrit and hemoculture. A few minutes later, the patient remained mentally confused, pulse rate 148, arterial pressure 80 x 60 mmHg, axillar temperature 42º C, dry skin, tachypnea and cyanosis. The following procedures were taken: sodium bicarbonate, vein dissection, central venous pressure control, furosemide, mannitol, oxygenation and cooling procedures were maintained, and another arterial gasometry was taken.
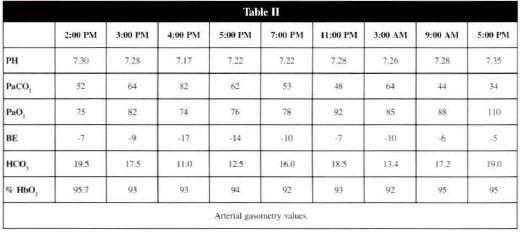
Clinical results in the subsequent 18 hours after this situation is reported in table I. The arterial gasometry values are shown in table II.

Other exams such as hemoglobin (7.3), hemarocrit (22) and creatine kinase (1500 U/ml and l8000 U/ml) were done.
No serious alterations were observed in sodium, potassium, amylase, calcium, coagulogram, reticulocytes counting, glicemia, urea and creatinine exams. During the following 18 hours after that situation, the patient remained always conscious, arterial pressure at about 90 x 50 mmHg, pulse rate always higher than 130, axillar temperature higher than 37.8º C.
During this time she still had dyspnea, radiological data compatible with pulmonary congestion and myalgia.
It was set up a treatment with intravenous dantrolene, 1 mg/kg. A few minutes later, the patient's situation was: arterial pressure 120 x 80 mmHg, pulse rate 86, axillar temperature 36º C, and recovery of the myalgia condition. The patient presented dyspnea and cough, in the 2nd and 3rd days PO. The X-ray examination revealed an interstitial pulmonary infiltrate. At that time, diuretics were administered.
She was discharged from hospital at the 4th postoperatory day presenting better pulmonary (symptomatic and X-rays) situation. Posterior exams indicated enzymatic levels regression. The hemocultures were negative. The patient was asked about similar episodes in the family and she reported that his father had had high fever, after an esophagoplasry surgery.
DISCUSSION
In our opinion, the case presents a situation compatible with MH, due to unexpected hyperthermia occurrence, after using succinylcholine and halothane, acidosis of difficult correction, tachypnea, cyanosis, muscular pain, creatine kinase rise (which is only found our changed in previous muscular diseases, leptospirosis, acute myocardial infarction, MH). There was an evident change for the better, using dantrolene and familiar history.
The ultimate objective of this report is to show the benefits of dantrolene even when administered some hours after the establishment of the case, preventing complications such as acute renal failure, adult respiratory distress syndrome and disseminated intravascular coagulation. Dantrolene is a skeletal muscle relaxant. Its main action consists in retaking calcium through sarcoplasmic reticulum. Its action is specific in MH, causing an entire regression of the situation, in few hours.
REFERENCES
1. XAVIER, L. Síndrome de Hipertermia Maligna. Rev. Bras. Anest. 1984; 34:61-69.
2. MILLER, R.D. Anesthesia. 2. ed. New York. 1986; 3:1971-1994.
3. SABISTON, D.C. Textbook of Surgery. 14. ed.Philadelphia. 1991; p. 301.
4. CIVETTA, J.M. Critical Care. 2. ed. Philadelphia. 1992; 904-6.
5. COLLINS, V.J. Princípios de Anestesiologia. 2. ed. Rio de Janeiro. 1978; 893-5.
6. BLITT, C.D. Monitoring in Anesthesia and Critical Care Medicine. 2. ed. Churchill Livingstone, 1990; 564-5.
I - Associate Member of the SBCP.
II - Titular Member of the SBCP. Plastic Sugery professor of Faculdade de Medicina de Santo Amaro. Medical Assistant of the Plastic Surgery. Department of Hospital do Servidor Público Municipal de São Paulo.
Address for Correspondence:
Paulo Roberto de Souza Jatene, MD
R. Sergipe, 401 - cj. 207/208
01243-001 - São Paulo - SP - Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter