

Original Article - Year 2019 - Volume 34 -
Omphaloplasty based on an isosceles triangle with double fixation in abdominoplasty
Onfaloplastia em triângulo isósceles e com dupla fixação na abdominoplastia
ABSTRACT
Introduction: In conventional abdominoplasty, the creation of a new umbilical scar is challenging. Several surgical techniques and approaches have previously been described and applied, but not always with satisfactory results. The objective is to demonstrate the applicability and satisfaction with omphaloplasty based on an isosceles triangle with double fixation in abdominoplasty.
Methods: The study included 97 female patients aged between 25 and 65 years. All underwent classic abdominal dermolipectomy with moderate abdominal liposuction of the entire anterior abdomen and flanks by the same surgeon and were evaluated at 90, 180, and 360 days postoperatively.
Results: Patients were satisfied with the umbilicus in most cases (92.8%). Some umbilical scars had contracted (3.1%) and others appeared unsightly (4.1%). No necrosis was observed.
Conclusion: This technique was effective and easy to perform, with satisfactory umbilical scar aesthetic outcomes in abdominal dermolipectomy.
Keywords: Liposuction; Abdominoplasty; Abdomen; Umbilicus; Scar
RESUMO
Introdução: Na abdominoplastia convencional, a cicatriz do novo umbigo representa o ponto de maior desafio. Em sua execução, já foram descritas e utilizadas várias técnicas e táticas cirúrgicas, com resultados nem sempre satisfatórios, sob o ponto de vista do paciente e também do médico. O objetivo é demonstrar a aplicabilidade e satisfação com a onfaloplastia em triângulo isósceles e com dupla fixação na abdominoplastia.
Métodos: Foram selecionadas 97 pacientes do sexo feminino, com idades entre 25 e 65 anos. Todas foram submetidas à dermolipectomia abdominal clássica associada à lipoaspiração moderada de todo abdome anterior e flancos e avaliadas com 90, 180 e 360 dias pós-operatórios, pelo mesmo cirurgião.
Resultados: Observou-se um índice de resultados satisfatórios das cicatrizes umbilicais na maioria dos casos (92,8%). Algumas cicatrizes umbilicais apresentaram estenoses (3,1%) e outras, cicatrizes inestéticas (4,1%). Não se observaram necroses.
Conclusão: A utilização desta técnica demonstrou ser eficaz, de fácil execução e com resultados muito satisfatórios na estética da cicatriz umbilical nas dermolipectomias abdominais.
Palavras-chave: Lipoaspiração; Abdominoplastia; Abdome; Umbigo; Cicatriz
INTRODUCTION
Abdominoplasty or abdominal dermolipectomy was described by Kelly1 in 1899 and is among the most common plastic surgery procedures.
Liposuction combined with abdominal dermolipectomy was described by Avelar² in 1998 and has subsequently been accepted as a routine procedure by other authors3-6.
Despite advances in various techniques and adaptations of this procedure, there is still no unanimous agreement on the creation of an umbilical scar, which remains a major challenge in abdominal plastic surgery.
The umbilical scar divides the human body exactly in the middle, according to Marcus Vitruvius7, a Roman architect, and this concept was perfected by Leonardo da Vinci in 1490. The evolution of omphaloplasty began in 1924, when Frist8 performed the first transposition of the umbilicus. Since then, many variations have been used in an attempt to approximate the appearance of the original umbilicus.
In the 1970s, Baroud9 and Regnaut7 used horizontal incisions in the abdominal flap, while in 1978, Avelar10 used a star-shaped incision.
Several techniques have been described: Juri et al.11 proposed the use of a V-shaped incision, Massiha et al.12 added a circular umbilical incision and a triangular incision in the abdominal flap, Malic et al.13 used an inverted U-shaped incision in the flap, and Castillo et al.14 used Y-shaped de-epithelized skin flaps.
Several authors2,7,8,9,13,15 have used various geometric shapes (Mercedes star, lozenge, ellipse, cross, rectangle, shield shape, infinity logo, and y-shape) in an attempt to obtain a more natural result in the creation of the umbilicus, but there is still no consensus on the best technique.
OBJECTIVE
To demonstrate the applicability and satisfaction with omphaloplasty based on an isosceles triangle with double fixation in abdominoplasty.
METHODS
This study included 97 female patients, with a mean age of 45 years (range, 25 to 65 years) who underwent omphaloplasty between January 2014 and December 2015.
The surgeries were performed at the STK-Plastic Surgery Center in Belo Horizonte, MG, by the same surgeon.
All patients received the same pre-, intra-, and postoperative care.
The guidelines of the principles of Helsinki were followed.
Surgical technique
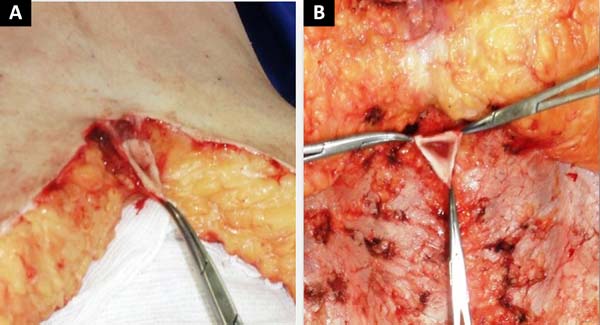
The abdominal flap was freed using an isosceles triangular incision, with an upper base measuring 2 cm and sides measuring 2.5 cm (Figure 1A and B).
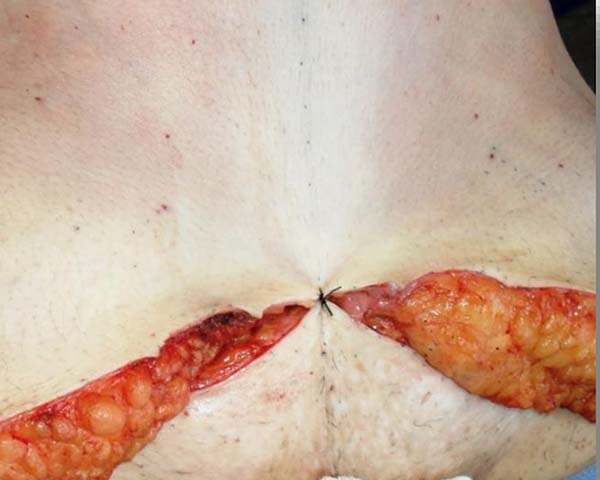
The abdominal flap was provisionally fixed in the suprapubic region (Figure 2).
The demarcation of the new umbilical implantation site began with a linear, 2-cm horizontal incision in the abdominal flap in place of the original projection of the umbilicus in the skin (Figure 3).
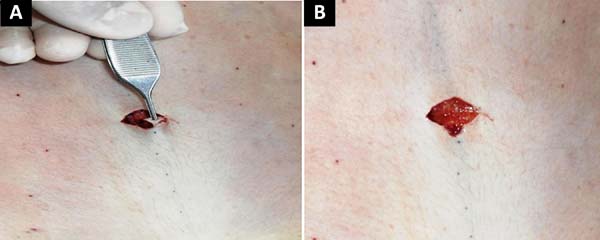
A triangle measuring approximately 0.5 cm was then removed from the middle third of the lower border of this incision (Figure 4 A and B).
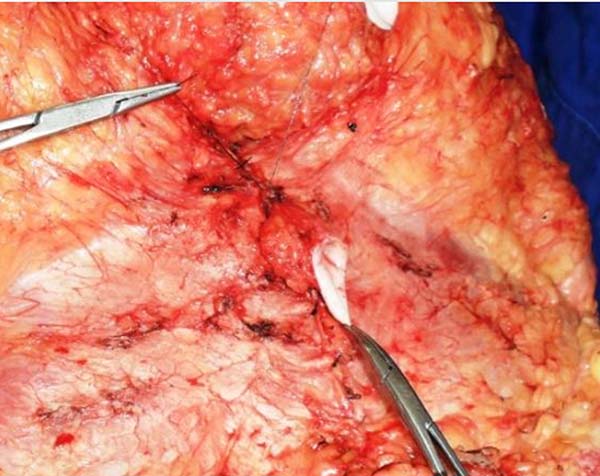
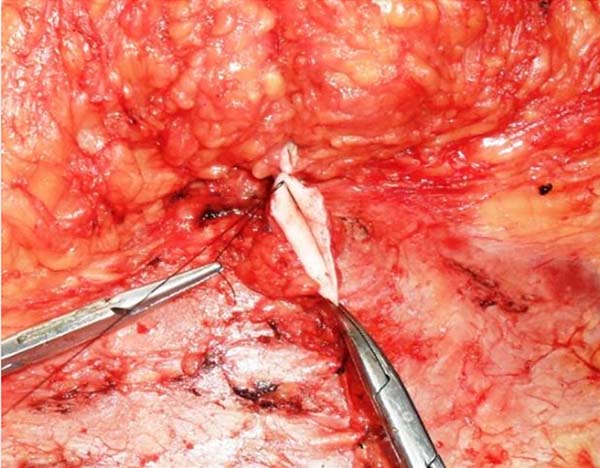
Once the skin incision was made at the new umbilical site, the flap fixation site was released to the suprapubic region. This flap was lifted to expose the detachment area and umbilicus. Fixation was performed with 3-0 monofilament nylon between the medial region of the upper edge of the new umbilical incision and the aponeurosis of the rectus abdominis at the upper base of the umbilical pedicle (Figures 5 and 6).
Next, the upper portion of the new umbilical incision was attached with a transcutaneous U-point to the upper portion of the umbilicus (Figure 7), with the knot buried in the umbilicus.
The umbilicus was transferred through the incision in the abdominal flap (Figure 8).
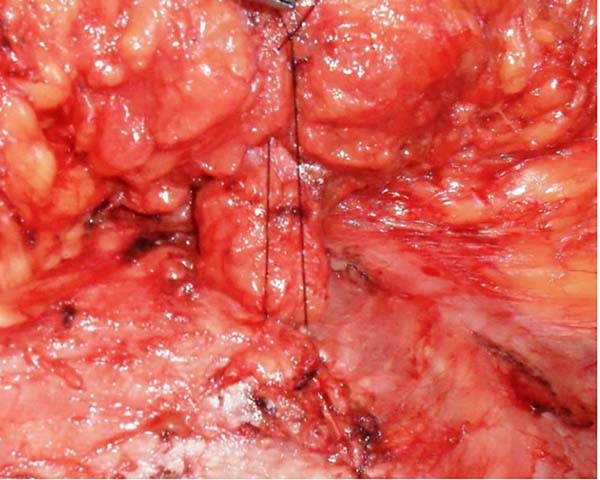
The angles of the umbilical triangle correspond to the angles of the flap incision and are fixed with 4-0 nylon monofilament (Figure 9).
Suturing of the umbilicus at the new site was completed with interrupted U sutures, using 4-0 monofilament nylon with knots buried in the umbilicus (Figure 10).
Finally, the inferior portion of the new umbilical incision was fixed in the abdominal flap to the aponeurosis of the rectus abdominis in the caudal portion of the umbilical pedicle, avoiding displacement of the umbilicus in the postoperative period and minimizing traction on the umbilical scar (Figure 11).
The abdominal flap was then pulled up to the suprapubic line for definitive fixation. Silicone umbilical belts were used in all patients.
RESULTS
The 97 patients were followed for up to 12 months after classic abdominal dermolipectomy with omphaloplasty based on an isosceles triangle with double fixation. A questionnaire was used for self-evaluation (Table 1) at 1 year postoperatively. Patients were asked about the degree of satisfaction with the umbilical abdominoplasty scar and whether they would recommend the surgery to a friend; they were also encouraged to write any comments related to the surgery.
| Very Satisfied | % | Satisfied | % | Slightly Satisfied | % | Yes | % | No | % | |
|---|---|---|---|---|---|---|---|---|---|---|
| How do you rate the abdominal scar? | 83 | 85.5 | 08 | 8.2 | 06 | 6.1 | ||||
| How do you rate the umbilical scar? | 80 | 82.5 | 10 | 10.3 | 07 | 7.2 | ||||
| Would you recommend the surgery to a friend? | 92 | 94.8 | 05 | 5.1 | ||||||
| List any relevant observations |
In all, 85.5% of the patients were very satisfied with the final outcome of the procedure, 8.2% were satisfied, and 6.1% were slightly satisfied. With respect to the umbilical scar, 82.5% were very satisfied, 10.3% were satisfied, and 7.2% were slightly satisfied.
Only 11 patients commented on the size of the abdominoplasty scar and 18 complained of severe postoperative pain.
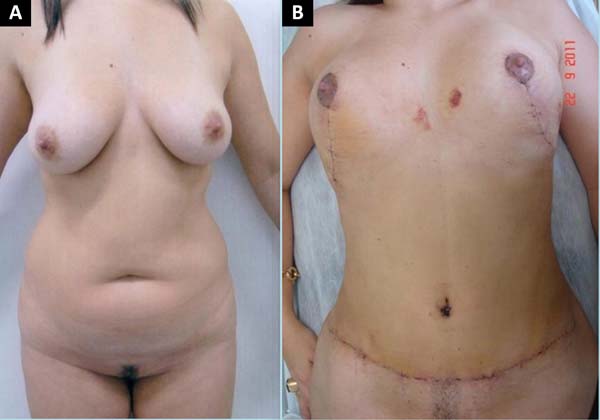
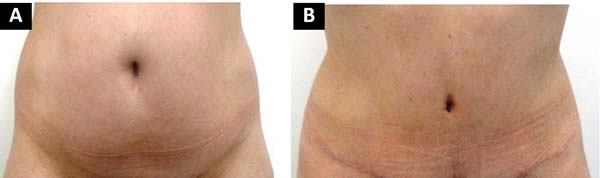
The surgeon assessed these 97 abdominoplasty patients at 90, 180, and 360 days postoperatively. At 1 year, the patients were evaluated for umbilical position on the abdomen, type of scar (atrophic, hypertrophic, and contracted), and scar depth; the overall results were satisfactory, with a low rate of complications (Figures 12, 13, 14, 15).
The complications are listed in Table 2.
| Contraction | Number | Percentage |
|---|---|---|
| Hypertrophy | 03 | 3.09% |
| Atrophy | 02 | 2.06% |
| Necrosis | 02 | 2.06% |
| Necrose | 00 | 0% |
DISCUSSION
The degree of satisfaction with abdominoplasty is usually high because of visible postoperative improvement, compared to the appearance of an abdomen affected by multiparity and fluctuations in body weight.
A poor-quality umbilicus compromises satisfaction with abdominoplasty, and the choice of an appropriate technique is a challenge for the plastic surgeon.
The technique described herein, with abdominal flap fixation to the aponeurosis of the rectus abdominis, superior and inferior to the umbilicus, avoids traction on the umbilical scar, favors the healing process, and promotes a natural appearance, approximating that of an ideal umbilical scar.
The 7 patients who reported poor satisfaction with the umbilical scar underwent a second surgical procedure for correction. This group included 2 patients with an enlarged scar, 2 with a hypertrophic scar, and 3 with scar contraction. Another patient with contraction had an unsatisfactory outcome, but the evaluation was made by the surgeon alone. All other patients reported being satisfied or very satisfied with the umbilical scar.
The 5 patients who would not recommend the surgery to a friend thought that the scar would be smaller, despite being given preoperative information. These 5 were among the 8 who reported only slight satisfaction with the abdominal scar.
Only 11 patients reported expecting a different appearance. Another 18 reported postoperative pain.
CONCLUSION
Omphaloplasty based on an isosceles triangle with double fixation was easy to perform and resulted in a more natural appearance, with overall patient satisfaction.
COLLABORATIONS
|
RC |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
BVBLC |
Analysis and/or interpretation of data; statistical analyses; writing the manuscript or critical review of its contents. |
REFERENCES
1. Kelly HA. Report of gynecological cases (excessive growth of fat). Johns Hopkins Med J. 1899;10:197-201.
2. Avelar JM. Uma nova técnica de abdominoplastia: sistema vascular fechado de retalho subdérmico dobrado sobre si mesmo, combinado com lipoaspiração. Rev Bras Cir. 1999;88/89(1/6):3-20.
3. Fournier PF, Otteni F. Treatment of localized lipodystrophies by aspiration. Chir Esthetic. 1982;59(2):73-8.
4. Klein JA. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol. 1990;16(3):248-63. DOI: https://doi.org/10.1111/j.1524-4725.1990.tb03961.x
5. Carvalho GB, Ribeiro VMN, Barbosa RCC, Coelho EM, Ferreira AC. Lipoaspiração. Res Hosp Geral Fortaleza. 2003;12(2):23-4.
6. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7.
7. Regnault P. The history of abdominal dermolipectomy. Aesthetic Plast Surg. 1978;2(1):113-23. DOI: https://doi.org/10.1007/BF01577945
8. Castro DPR, Saldanha OR, Pinto EBS, Albuquerque FM, Moia SMS. Avaliação estética da cicatriz umbilical em duas técnicas de onfaloplastia. Rev Bras Cir Plást. 2014;29(2):248-52
9. Baroudi R. Umbilicaplasty. Clin Plast Surg. 1975;2(3):431-48.
10. Avelar J. Abdominoplasty-Systematization of a technique without external umbilical scar. Aesthetic Plast Surg. 1978;2(1):141-51. DOI: https://doi.org/10.1007/BF01577947
11. Juri J, Juri C, Raiden G. Reconstruction of the umbilicus in abdominoplasty. Plast Reconstr Surg. 1979;63(4):580-2. PMID: 424470 DOI: https://doi.org/10.1097/00006534-197904000-00032
12. Massiha H, Montegut W, Phillips R. A method of reconstructing a natural-looking umbilicus in abdominoplasty. Ann Plast Surg. 1997;38(3):228-31. DOI: https://doi.org/10.1097/00000637-199703000-00007
13. Malic CC, Spyrou GE, Hough M, Fourie L. Patient satisfaction with two different methods of umbilicoplasty. Plast Reconstr Surg. 2007;119(1):357-61. PMID: 17255693 DOI: https://doi.org/10.1097/01.prs.0000244907.06440.f8
14. Castillo PF, Sepúlveda CA, Prado AC, Troncoso AL, Villamán JJ. Umbilical reinsertion in abdominoplasty: technique using deepithelialized skin flaps. Aesthetic Plast Surg. 2007;31(5):519-20. DOI: https://doi.org/10.1007/s00266-006-0225-2
15. López-Tallaj L, Gervais J. Restauração umbilical na abdominoplastia: uma simples técnica retangular. Rev Bras Cir Plást. 2001;16(3):39-46.x
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil
2. Universidade Estadual de Montes Claros, Montes
Claros, MG, Brazil
3. Faculdade de Medicina de Petrópolis, Faculdade
Arthur Sá Earp Neto, Petrópolis, RJ, Brazil.
Corresponding author: Roney Campos Av João César de Oliveira, nº 1298, sala 605 - Eldorado, Contagem, MG, Brasil Zip Code 32310-000 E-mail: roneycampos66@hotmail.com
Article received: April 6, 2017.
Article accepted: November 27, 2018.
Conflicts of interest: none.

























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter