

Original Article - Year 2019 - Volume 34 -
Zygomatic-palpebral flap: an optional technique for lower eyelid reconstruction
Retalho zigomático-palpebral: uma técnica opcional para a reconstrução da pálpebra inferior
ABSTRACT
Introduction: Lower eyelid reconstruction represents a unique challenge to plastic surgeons, since it involves a facial region of aesthetic and functional importance. The objective is to present an optional technique for the reconstruction of lower eyelid defects using zygomatic-palpebral skin flap. This technique represents an alternative in cases of scleroatrophic skin in older patients, and for young people who do not have an upper eyelid skin redundancy, which prevents, for example, the use of upper eyelid grafts or flaps such as those of Fricke or Tripier.
Methods: The authors describe the flap used in cases of cicatricial ectropion and reconstruction after resection of neoplasms and association with other flaps, such as those of Hughes, or for coverage of cartilage grafts. The flap consisted of a transposition flap made up of skin and underlying subcutaneous tissues, randomized . The technique was based on the use of a local flap with highly similar characteristics to the defect area, which allowed it to mimic functions, while being safe and feasible.
Results: The immediate and late results in terms of aesthetics and function were satisfactory and well accepted by patients and the surgical team, with adequate eyelid occlusion and preserved ocular lubrication.
Conclusion: The advantages of the zygomatic-palpebral flap are its ease of execution, minimal bleeding, low morbidity of the donor area, and the use of local anesthesia. The reconstruction of eyelid defects aims to restore anatomy and function. This can be a challenging task, especially in cases with larger defects that may be present after oncologic procedures both in young and old patients presenting with scleroatrophic skin and minimal tissue laxity.
Keywords: Keywords: Eye; Eyelids; Conjunctiva; Eyelid diseases; Reconstructive surgical procedures; Flaps
RESUMO
Introdução: A reconstrução de pálpebra inferior representa um desafio peculiar ao cirurgião plástico, uma vez que traduz uma região facial de importância estética e funcional. O objetivo é apresentar uma técnica opcional para a reconstrução de defeitos da pálpebra inferior com o retalho cutâneo zigomático-palpebral. Esta técnica mostra uma alternativa nos casos de pele escleroatrófica de pessoas idosas, bem como para pessoas jovens, que não apresentam redundância da pele palpebral superior, impossibilitando por exemplo o uso de enxertos de pálpebra superior ou retalhos como o de Fricke ou Tripier.
Métodos: Os autores mostram a indicação do retalho em casos de ectrópio cicatricial, reconstrução após ressecção de neoplasias, associação com outros retalhos como de Hughes ou para cobertura de enxertos cartilaginosos. É um retalho de transposição composto por pele e subcutâneo, randomizado. A técnica baseia-se no uso de retalho local, de características muito semelhantes à área do defeito, o que permite mimetização, segurança e exequibilidade.
Resultados: Os resultados imediatos e tardios são satisfatórios e bem aceitos pelos pacientes e pela equipe cirúrgica em termos estéticos e funcionais, com oclusão palpebral adequada e lubrificação ocular preservada.
Conclusão: O retalho zigomático-palpebral apresenta como vantagens a simplicidade de execução, sangramento mínimo, baixa morbidade de área doadora e feito sob anestesia local. O objetivo de reconstruir defeitos da pálpebra é restaurar a anatomia e função. Esta pode ser uma tarefa desafiadora, especialmente em defeitos maiores que podem estar presentes nos procedimentos oncológicos em jovens e em idosos com pele escleroatrófica e mínima frouxidão.
Palavras-chave: Olho; Pálpebras; Túnica conjuntiva. Doenças palpebrais; Procedimentos cirúrgicos reconstrutivos; Retalhos
INTRODUCTION
Reconstruction of eyelid defects focuses on two major targets: restoring the anatomy and eyelid function. This can be a challenging task, especially in larger defects, such as those occurring after oncologic procedures in young people with minimal tissue laxity and elderly patients with scleroatrophic skin, and in cases of trauma or burns with significant tissue loss.
Several reconstructive techniques have been developed and the surgical choice usually depends on the affected portion of the eyelid and the extent of the defect. Reconstructive procedures must maintain the function and integrity of the periorbital structures while seeking adequate aesthetic repair. The objectives of eyelid reconstruction should consider the following aspects:
Smooth and soft internal conjunctival mucosa - eye lubrication; A stable eyelid margin with rigid support such as the tarsus in order
to ensure shape and stability;
Eyelid stiffness in the canthal ligaments; Functionally active muscles that allow tonus; Adequate eyelid occlusion to maintain eye protection; Acceptable aesthetic result in terms of facial symmetry.
In this study, the authors presented the use of zygomatic-palpebral flap, a technique initially described by Hermann Eduard Fritze in 1845, which despite its antiquity has proven to be a safe and versatile option with good results for lower eyelid reconstruction.
OBJECTIVE
This study aimed to present an optional technique for the reconstruction of defects of the anterior lamella of the lower eyelid using the zygomatic-palpebral skin flap. This technique is an excellent alternative in cases of scleroatrophic skin in elderly patients, as well as in young people not presenting upper eyelid skin redundancy, which prevents, for example, the use of upper eyelid grafts or flaps such as that of Fricke or Tripier. Moreover, this technique is also indicated for retraction due to burns, trauma or in association with other techniques.
METHODS
The flap was indicated in cases of ectropion, reconstruction after resection of neoplasms, and in association with other flaps, such as those of Hughes, in order to cover cartilage grafts and retractions caused by burns. It consisted in a transposition flap composed of skin and underlying subcutaneous tissues, randomized. This technique is based on the use of local flaps with highly similar characteristics to the defect area, allowing it to mimic functions while being safe and feasible.
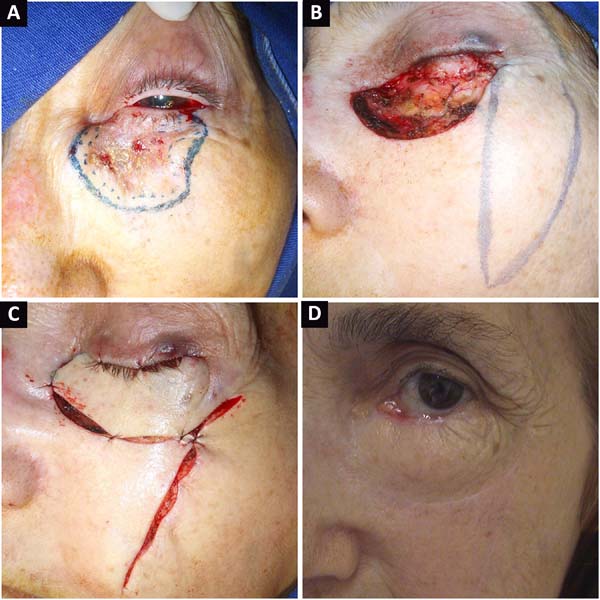
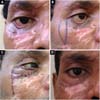
The procedure for creating the flap was the same in all cases. The limits of the receiving area were evaluated (Figure 1A), and based on the extent of the defect, the donor area was delimited in the ipsilateral malar region. Then, the flap was marked in the zygomatic region (Figure 1B) from the lateral corner of the eyelid, descending perpendicularly to 90º in relation to the lower ciliary margin. The skin flap was raised along with a sufficient thick layer of subcutaneous tissue in order to fill the defect entirely (Figures 1C, 1D). Subsequently, the transposition process took place, followed by closure of the donor and receiving areas using deep subdermal stitches (4-0 polydioxanone) and simple separated stiches (6-0 monofilament nylon) superficially (Figure 1E).
RESULTS
The zygomatic-palpebral flap for lower eyelid reconstruction allowed the restoration of height and palpebral vertical length, preventing and correcting ectropion. The immediate results (Figure 1F) and late results in terms of aesthetics, scar quality and function were satisfactory and well accepted by both patients and surgical team, with adequate eyelid occlusion and preserved eye lubrication.
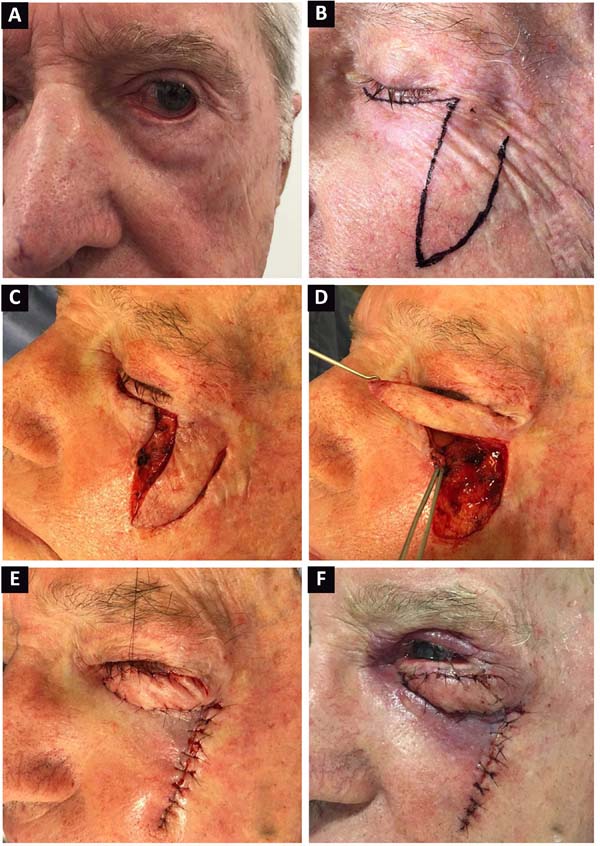
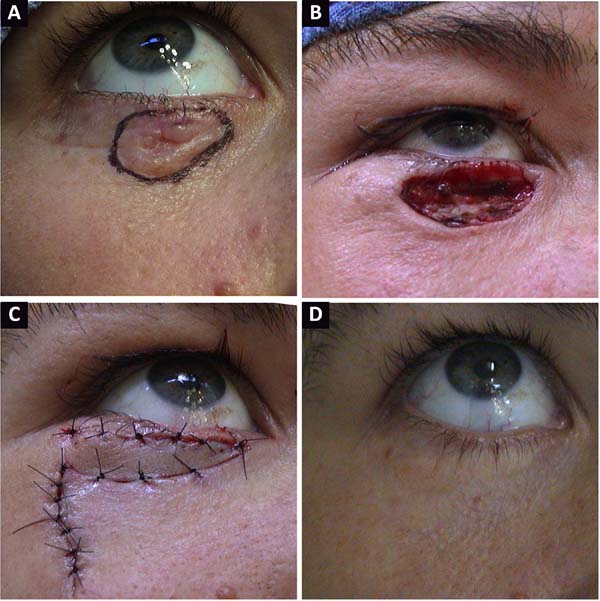
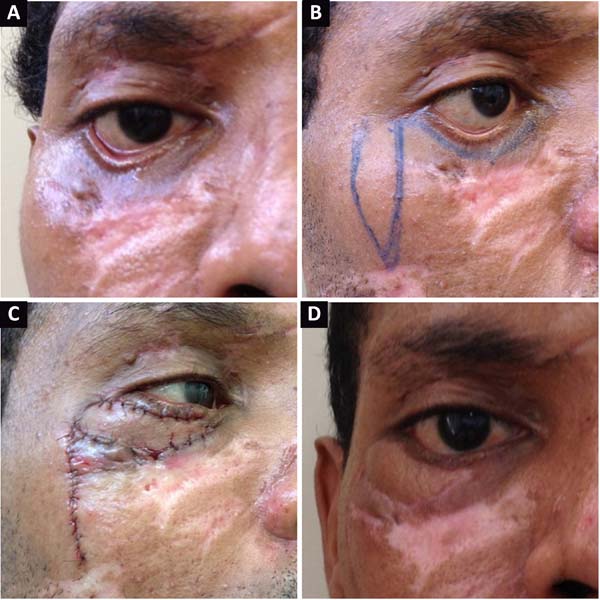
Lymphatic edema of the flap was the greatest complaint in operated cases, but it resolved spontaneously within approximately 6 months. Infection, surgical dehiscence, hematomas, and other complications were not recorded. Figures 2 and 3 present cases of reconstruction of the lower eyelid due to a skin cancer in a young and in an elderly patient, respectively. Moreover, correction of a scar ectropion in a burn victim is presented in Figure 4.
DISCUSSION
The eyelids cover and protect the eyes. Their function is to protect the eyes against excessive light, trauma, or dryness. Moreover, they contain glands that produce mucus, lubricants, and lipids that make up the tear film. Eyelids are divided into three lamellae. The anterior lamella contains skin and muscle, the middle lamella contains the orbital septum, and the posterior lamella contains tarsus, tarsal plates, and the retractor muscles of the eyelid and conjunctiva. The skin of the eyelids is extremely thin, and the skin of the upper eyelid is thinner than that of the lower eyelid, since there is little subcutaneous fat at the base of the eyelid skin.
Eyelid reconstruction techniques involve the restoration of all lamellae, with at least one of these layers having to be well vascularized. Flaps are preferable when compared to grafts due to the like-to-like phenomenon - similarity with the adjacent skin in texture, color, thickness, and elasticity, besides having intrinsic blood supply, maintenance of tactile sensation, the same surgical field, and durability. However, for partial thickness defects, skin grafts may be highly recommended. A satisfactory reconstruction of the lower eyelid should allow juxtaposition of the eyelid to the eyeball in order to prevent the onset of ectropion.
The eyelid reconstruction technique is chosen based on the thickness and extent of the defect. Direct closure techniques can be used in defects of up to 30% in young patients, and up to 45% in elderly patients. In borderline cases, a lateral cantholysis may provide additional relaxation for wound closure.
Local and regional flaps are useful for reconstruction of the lamella. Flaps, as described previously by Tenzel, Hughes, Mustardé, and Cutler, are well known among plastic surgeons and are useful for reconstruction of large defects, as well as cartilage grafts1-6. Tarsus with free margin associated with myocutaneous flap can be used for reconstruction of the posterior lamella.
A literature review showed that the choice of the technique for lower eyelid reconstruction varied according to the skin texture, scars adjacent to the recipient area, patient’s age, probable aesthetic result, size of the defect, and already used alternatives. The zygomatic-palpebral flap technique has some advantages, including the ease of execution, minimal bleeding, low morbidity of the donor area, and the ability to perform it under local anesthesia. Although some authors questioned that the flap design did not consider any of the aesthetic subunits of the face (this being the greatest reservation found in the literature), the scars along the malar region are usually considered as aesthetically acceptable by the patients and surgical teams.
CONCLUSION
Zygomatic-palpebral flap is an alternative technique that can be used in cases of scleroatrophic skin in elderly patients and young patients without sufficient tissue to reconstruct major defects.
COLLABORATIONS
|
AGM |
Analysis and/or data interpretation, conception and design study, data curation, project administration, writing - original draft preparation, writing - review & editing. |
|
MPSN |
Analysis and/or data interpretation, data curation, project administration. |
|
LRCCT |
Data curation, writing - original draft preparation. |
|
MTRC |
Data curation. |
|
CRRC |
Data curation. |
|
VAP |
Data curation. |
|
JPRP |
Data curation. |
REFERENCES
1. Alghoul M, Pacella SJ, McClellan WT, Codner MA. Eyelid reconstruction. Plast Reconstr Surg. 2013;132(2):288e-302e. PMID: 23897357
2. Putterman AM. Deep and superficial eyelid fascia. Plast Reconstr Surg. 2012;129(4):721e-3e.
3. Fezza JP, Massry G. Lower Eyelid Length. Plast Reconstr Surg. 2015;136(2):152e-9e.
4. Jindal K, Sarcia M, Codner MA. Functional considerations in aesthetic eyelid surgery. Plast Reconstr Surg. 2014;134(6):1154-70. DOI: http://dx.doi.org/10.1097/PRS.0000000000000748
5. Orgill DP, Ogawa R. Current methods of burn reconstruction. Plast Reconstr Surg. 2013;131(5):827e-36e. PMID: 23629122
6. Alves JCRR, Liu RP, Silva Filho AF, Pereira NA, Carvalho EES. Reconstrução palpebral com enxerto de cartilagem autóloga de concha de orelha. Rev Bras Cir Plast. 2012;27(2):243-8. DOI: http://dx.doi.org/10.1590/S1983-51752012000200013
1. Universidade Federal do Triângulo Mineiro,
Uberaba, MG, Brazil.
Corresponding author: Aluísio Gonçalves Medeiros Rua José de Alencar, nº 904, apto 203 - Abadia, Uberaba, MG, Brazil Zip Code 38025-120 E-mail: aluisiogm@hotmail.com
Article received: June 20, 2018.
Article accepted: November 11, 2018.
Conflicts of interest: none.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter