

Articles - Year 1998 - Volume 13 -
Gradual Bone Distraction in Craniosynostosis - Preliminary Results in Seven Cases
Tratamento da Síndrome de Apert e da Anomalia de Crouzon por Alongamento Ósseo Gradual
ABSTRACT
Seven patients with craniosynostosis (mean age 8 years, Apert syndrome, n=4, Cronzon's disease, n=3) underwent lengthening of the skull by gradual bone distraction. Three patients (group A) were treated by coronal craniectomy reaching the orbital fissure and gradual bone distraction. The other four patients (group B) underwent monobloc craniofacial disjunction and gradual bone distraction. The patients' progress was monitored clinically as well as by radiographs and photographs. The results showed that craniofacial disjunction followed by gradual bone distraction produced complete correction of exophthalmus and an improvement in the functional and aesthetic aspects of the middle third of the face without the need of bone grafts.
Keywords: craniofacial bone distraction; skull lengthening; craniosynostosis; Apert; face advance; Crouzon.
RESUMO
Foi realizado alongamento gradual de ossos do crânio em pacientes portadores de craniossinostose (quatro Síndromes de Apert e três Anomalias de Crouzon). Três pacientes (grupo A) foram submetidos a craniectomia coronal atingindo a fissura orbital e alongamento ósseo gradual. Outros quatro pacientes (grupo B) foram submetidos a disjunção craniofacial em monobloco (Ortiz - Monasterio, 1978) e alongamento ósseo gradual. Os pacientes foram avaliados por exames clínicos e documentação radiográfica e fotográfica. Os resultados demonstraram que a disjunção craniofacial seguida de alongamento ósseo gradual produziu correção completa da exoftalmia e melhora significativa nos aspectos estéticos e funcionais do terço médio da face) sem o uso de enxertos ósseos.
Palavras-chave: craniossinostose; alongamento ósseo craniofacial; Apert; Crouzon; disjunção craniofacial
The first report of lengthening of long bones of which we are aware was performed in 1905 by Codivilla(l).
Ilizarov(3, 4), has made several studies that make important contributions to this technique by avoiding complications and improving results. He has shown the benefits of doing only a corticotomy to preserve the medullary bone with minimal disruption of the periosteum and endosteum.
The gradual distraction of the mandible was first done in a dog with an extraoral device by Snyder et al. in 1973(12) and they suggested the possibility of applying this method to the human mandible in the treatment of some congenital deformities or for the consequences of trauma.
Michieli and Miotti(9) repeated the experiment in dogs using an intraoral device. Karaharju-Swanto et al. tested in 1990(5) an external fixation device that was applied to the mandibular ramus of sheeps to lengthen the mandible. Karp et al. in 1990(6) used a device in dogs to confirm the feasability of the technique.
Komuro et al. in 1994(7) studied the micromorphological aspects of distraction osteogenesis of the mandible in rabbits and showed that both endochondral and intramembranous ossification occurred and resulted in cortical bone after eight to ten weeks of completion of distraction. Constantino et al in 1994(2) reported segmental mandibular regeneration of a created segmental defect by bifocal distraction osteogenesis in dogs.
In 1992, McCarthy et a1.(8) used the Ilizarov method(3, 4) and published the first results of human mandible distraction with an extraoral device comprising two pins of fixation in each side of the osteotomy in four patients. In 1995, Molina and OrtizMonasterio(lO), presented a study showing good results with one pin of fixation in each side of the osteotomy.
In 1996, Raposo do Amaral(l3) presented results in mandibular distraction at the 11th Congress of the International Confederation for Plastic Reconstructive and Aesthetic Surgery, Yokohama, Japan.
Considering the results acquired in mandibular lengthening, we proposed the gradual distraction technique to correct the craniofacial deformities in patiens with craniosynostosis, Crouzon's disease, and Apert syndrome.
MATERIAL AND METHODS
The skull was distracted by applying an external bone lengthening device to seven patients with craniofacial deformities, four with Apert syndrome and three with Crouzon's disease. We studied the patients in two groups: Group A was made up of three girls aged between 6 and 9 years old, two with Apert syndrome and one with Crouzon's disease (Table I). They underwent coronal craniectomy that reached the orbital fissure (Fig. 1). The anterior portion of the apparatus was put in the lateral inferior orbital and zygomatic bone (malar region), and the posterior portion was put in the temporal bone.


Fig. 1 - Schematic illustration of the coronal craniectomy and lengthening of the posterior portion of the skull.
The distraction started in the operating room and was done for several days at the maximum rate that the patient could accept (mean rate O,8mm/day) (Table II).

Group B. This group underwent monobloc craniofacial disjunction as described by Ortiz-Monasterio(ll) and a newly designed apparams was used. The anterior portion of the apparams was put in the lateral inferior orbital and zygomatic bone (malar region).
The posterior portion was put in the temporal bone (Fig. 2). The distraction started seven days after the operation, at the mean rate of 1.4 mm/day (Table 11).

Fig. 2 - Schematic illustration of the craniofacial disjunction and gradual distraction with advance of the face.
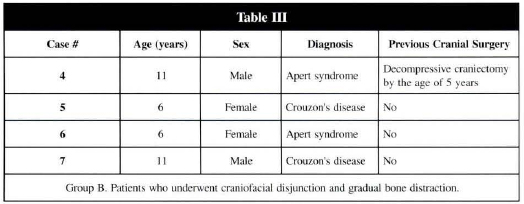
We smdied four patients in this group (Table III).
The device is kept on place during eight weeks after the distraction period in all the seven cases.
To evaluate the procedure, the following craniofacial measurements were made before, during, and after the distraction: exophthalmometry, cephalic perimeter, and biauricular and anteroposterior distance. In the cephalometric radiograph the following measurements were made: sella turcica - the most concave point of the maxilla (SA); sella turcica - nasium (SN); sella turcica - occiput (SO); naso-occiput (NO), craniectomy gap (FT), and the angles: sella turcica - nasium - the most concave point of the maxilla (SNA) and sella turcica - nasium - the most concave point of the mandible (SNB).
RESULTS
The distraction effectively advanced the forehead. The group A patients (Tables IV and V) had more cranial lengthening in the occipital direction (SO 5.8 mm) than in the forehead direction (SN 2.8 mm).


The skull had a "fan like" movement, with a big range craniectomy gap (FT 11.5) (Fig. 3). The exophthalmus had little improvement (mean variation 1.8 mm), but clinical examination showed improvement in conjunctival hyperemia, epiphora, and eye occlusions.

Fig. 3a - Group A patient (Crouzon's desease). Preoperative situation, right profile.

Fig. 3b - Postoperative result.
The intercurrences did not change the final results.
One patient had seroma, pain to distraction occured in two patients, one patient had partial temporary left side facial nerve deficit and left eye muscle partial deficit, that returned to normality after taking off the apparatus.
One patient (case 2) had little changes not only at clinical examination, but also at cephalometric analysis, probablly due to bad location of apparatus, since bilateral partial extrusion of the internal part of the apparatus occured. In one patient, (case I) sella turcica lengthening with range 8 mm was observed (Fig. 4).

Fig. 4a - Group A patient, pre-operative radiograph.

Fig. 4b - Postoperative radiograph: lengthening of the sella turcica.
Patients in group B had great advance of the face and maxilla (SN, SA, and SNA mean variation) and a little movement of the occipital portion of the skull to backward (SO) as shown in Table V. Clinically the patients had increased the antero-posterior distance and cephalic perimeter (Table IV).
Two patients had more midface advance than upper face advance. In one patient cephalic perimeter decrease was observed. Exophthalmus also had correction (mean 11.7 mm) with good improvement in epiphora, conjunctival hyperemia, and eyes occlusions.
The intraoperative intercurrences were: midline palatal fracture in two patients, frontonasal fracture in one patient, and one patient had Le Fort class III fracture.
The postoperative intercurrences were: meningitis (Streptococcus pneumoniae), liquoric fistula, temporary partial deficit left side facial nerve, pulmonary atelectasis in the same patient, and apparatus relocation in two patients. All these patients presented occlusion class III (Angle) and important retrusion of the maxilla preoperatively. After the distraction period occlusion became class II with little over correction. The middle third of the face advanced more than the upper third of the face in one patient.
DISCUSSION
Patients in group A, who underwent decompressive craniectomy reaching orbital fissure and gradual bone distraction, had a "fan like" movement with more lengthening of the posterior portion of the skull. The condition in wich the apparatus was located suggested that the posterior portion of the skull is more sensible to gradual bone distraction.
The movement of the apparatus was always greater than the movement observed in the bone by the cephalometric analysis. This can be explained by the penetration of the apparatus claw into the bone that occurred at the temporal bone, or because the measurements were performed in a different vector than the apparatus disctraction.
In one of the patients the maxilla moved anteriorly.
Despite exophthalmus correction was poor there was an improvement in the lateral view of the superior third of the face, and anterior projection of the frontal bone.
One of the patients presented lengthening of the sella turcica, that suggested the possibility of promoting growth of the skull base in young children.
The group B osteotomies were more difficult to do because we used minimal undermining using a high frontal osteotomy. Endoscopic apparatus can be useful in guiding the osteotomies. Technical difficulties while doing the osteotomies resulted in incomplete palatal midline fractures at Rowe's manoeuvre that can be avoided by using a palatal plate. The Le Fort class III fracture that occurred in one patient was fixed with wire. The immobilisation in such circumstances must be done using miniplates to give more stable bone fixation during the bone distraction.
Except for case 4, the coexisting diseases and complications were basically in the location of the apparatus and were corrected with minimal interventions.
Patients in group B underwent a more rapid distraction of the apparatus than of bone, but the differences were smaller than in group A (table II). This probablly happened because with complete osteotomy the advance of bone is similar to the advance of the apparatus. Case 4 did not behave this way; probably because of his coexisting diseases the distraction began on the 26th postoperative day, after the facial advance that had been produced by the operation itself.
One of the patients developed posterior rotation of the forehead with increased anterior projection of the maxilla. To achieve correction of the forehead another distraction apparatus was put at the sagittal line of the skull. The application of two apparatuses - one on each side - and another one in the midlle line of the skull is useful to control the distraction better, and avoids rotational movements.
All patients had good correction of exophthalmus, and the occlusion that had been class III Angle became class II. We expect that with mandibular growth the occlusion will be better.
Patients from 6 to 11 years old were chosen because we had more cooperation from these patients, not only to carry out the distraction but also to perform the cephalometric radiographs and the clinical measurements.
We believe that this new technique applied in young children can achieve encouraging results.

Fig. 5a - Group B patient (Apert syndrome). Preoperative situation.

Fig. 5b - Postoperative result showing the advancement of the maxilla and correction of the exophthalmia.

Fig. 6a - Group B patient. Preoperative occlusion (Angle's class III).

Fig. 6b . Postoperative aspect showing advancement of the maxilla and Angle's class II occlusion.

Fig. 7a - Group B patient presenting Crouzon's disease.

Fig. 7b - Profile view during the lengthen period. Two lateral and one sagittal device were used in the advancement of the frontal region.
ACKNOWLEDGEMENTS
We thank Antonio Silva Bastos Neto, MD (anaesthesiologist), Gisele Aparecida Schneck and Rosangela Freitas Silvestre (nurses) and João Luis Silva (computer system analyst), from SOBRAPAR.
REFERENCES
1. CODIV1LLA A. On the means of lengthening in the lower limb. The muscles and tissues which arc shortened through deformity. Am. J. Orthop. Surg. 1905; 2:353·369.
2. CONSTANTINO PP, SHYLRET G, FRIEDMAN CD, et al. Segment mandibular regeneration by distraction osteogenesis. Arch. Otolaryngol. Hend Neck Surg.1994; 116:535-545.
3. ILIZAROV GA. The tension-stress effect on the genesis and growth of tissues: I. The influence of stability of fixation and soft-tissue preservation. Clin. Ortbop. 1989; 238:249-282.
4. ILIZAROV GA. The tension-stress effect on the genesis and growth of tissues: II. The influence of the rate and frequency of distraction. Clin. Orthop. 1989; 239:263·286.
5. KARAHARJU-SWANTO T, KARAHARJU EO, RANTA R. Mandibular distraction. An experimental study on sheep. J. Craniomaxillofac. Surg. 1990; 18:280-283.
6. KARP NS, THORME CHM, McCARTHY JG, SISSONS HA. Bone lengthening in the craniofacial skeleton. Ann. Plast. Surg. 1990; 24: 231-237.
7. KOMURO Y, TAKATO T; HARII K, YONEMARA Y. The histologic analysis of distraction osteogeneses of the mandible in rabbits. Plast. Raconstr. Surg. 1994; 94: 152-159.
8. McCARTHY JG, SCHREIBER J, KARP NS, THORME CHM, GRAYSON BH. Lengthening the human mandible by gradual distraction. Plast. Reconstr. Surg. 1992; 89: 1-8.
9. M1CHIELI S, MIOTTI B. Lengthening of mandibular body by gradual surgical - orthodontic distraction. J. Oral Surg. 1990; 24: 231.
10. MOLINA F, ORTIZ-MONASTERIO F. Mandibular elongation and remodeling by distraction: a farewell to major osteotomies. Plast. Reconstr. Surg. 1995; 96:825-840.
11. ORTIZ-MONASTERIO F, FUENTE DEL CAMPO A, CARRILLO A. Advancement of the orbits and the midface in one piece, combined with frontal repositioning, for the correction of Crouzon's deformities. Plast. Reconstr. Surg. 1978; 61 :507-516.
12. SNYDER CC, LEVINE GS, SWANSON HM, et al. Mandibular lengthening by gradual distraction. Preliminary report. Plast. Reconstr. Surg. 1973; 51 :506-508.
13. RAPOSO do AMARAL CM. A new strategy for reshaping the craniofacial skeleton. In: 11th Congress of the International Confederation for Plastic, Reconstructive and Aesthetic Surgery, 1995, Yokohama, Japan.
I - Head of Plastic Surgery, Dept. Surgery, Faculdade de Ciencias Medicas - UNICAMP. President of Sociedade Brasileira de Pesquisa e Assistencia para Reabilitação Craniofacial - SOBRAPAR. Professor of Plastic Surgery, Pontifícia Universidade Católica de Campinas.
II - Chair of Plastic Surgery, Dept. Surgery, Faculdade de Ciências Médicas - UNICAMP
III - Assistant at SOBRAPAR.
IV - Professor at Pontifícia Universidade Católica de Campinas.
V - Plastic Surgeon.
VI - Professor of Plastic Surgery, Dept. Surgery, Faculty of Medical Sciences, State University of Campinas.
Address for Correspondence:
Cassio Menezes Raposo do Amaral, MD
Caixa Postal 6028
Av. Adolfo Lutz, 100
13081-970 - Campinas - SP - Brazil
Phone: (55 19) 289-4465 - Fax: (55 19) 289-5380
e-mails:cassio@raposoamaral.com.br
cassio@sobrapar.org.br
Sociedade Brasileira de Pesquisa e Assistencia para Reabilitação Craniofacial - SOBRAPAR


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter