

Articles - Year 1998 - Volume 13 -
Breast Reconstruction: Geometrical Principles of the Cutaneous Flaps in Double V
Reconstrução Mamária: Princípios Geométricos dos Retalhos Cutâneos em Duplo V
ABSTRACT
The authors describe the Geometric Principles to perform the Mammary Reconstruction utilizing Cutaneous Flaps in Double V, associated with the Implantation of Mammary Prosthesis. This technique has been developed and used in 10 patients since 1996. Easy to be executed, the flaps are characterized by the facility of transposition and rotation, good vascularization viability and by the fact that they assure an adequate shape and positioning of the breast, which volume is assured by the mammary implant. Besides the good aesthetic results and almost unseen scars, by the functional point of view, they achieve a greater mobility to the axillary area, formerly retracted. The technique allows as well the reshaping of the other side breast, nipple and areola complex, in one time surgery, lessening the psycho-emotional traumas to the patients with mammary cancer, victims of physical and psychological mutilations caused by mastectomies.
Keywords: breast reconstruction; cutaneous flaps; surgical geometry; z-plasty; mammary implant.
RESUMO
Os autores descrevem os Princípios Geométricos para realização de Reconstrução Mamária com utilização dos Retalhos Cutâneos em Duplo V, associados à Implantação de Prótese de Mama, técnica desenvolvida e usada em 10 pacientes desde 1996. De fácil execução, os retalhos se caracterizam pela facilidade de transposição e rotação, boa viabilidade circulatória e por garantirem adequada forma e posicionamento da neo mama, cujo volume é garantido pelo implante mamário. Além dos bons resultados estéticos obtidos e cicatrizes dissimuladas, do ponto de vista funcional, os retalhos também oferecem maior mobilidade à região axilar outrora retraída. A técnica permite, ainda, a "adequação' da mama contralateral e a reconstrução do complexo aréolo-mamilar, em um único tempo, permitindo menor número de intervenções cirúrgicas, minimizando, desta forma, os traumas da esfera psico-emocional às pacientes portadoras de neoplasia mamária, vítimas das mutilações físico-psíquicas decorrentes das mastectomias.
Palavras-chave: reconstrução mamária; retalhos cutâneos; geometria cirúrgica; zetaplastia; implantes mamários
The breasts, considered to be the identification of the feminine sexuality, have been, for many years, the main reconstruction points of the Repairing Plastic Surgery which is concerned not only with returning (bringing back) the absent volume but also with alleviating the emotional condition of the woman who faces serious problems due to the sudden amputation she has been submitted to.
The postmastectomy mutilations vary according to the oncological surgery applied (basically: radical and myoconservative mastectomies, and quadrantectomies)(39). The same way, the kind of reconstruction varies according to the structures involved, and, therefore, the different techniques have as their objective the reparation of the mammary cone (isolated or associated to the other thoracic structures)(40).
Such kind of reconstructive surgery presents several problems, specially concerning the scar and the surrounding tissue (points which have been largely approached by the multiple techniques described (adjacent flaps, myocutaneous flaps, free flaps, island flaps and mammary implants)(4,7,24,27,28). Another controvert point among specialists has to do with the moment when the mammary reconstruction will be performed: immediately or delayed(23,40).
However, in the current era, the multidisciplinary team that is responsible for attending the mastectomized patient (specially: mastologist, oncologist, radiologist, plastic surgeon and psychoanalyst) seems to emphasize the importance of the psychical morbidity caused by this illness and its radical treatment, and its influence to the devised prognosis and life quality(23).
In search of a breast reconstruction technique which would cause less surgical traumas and, consequently, less physical-psychic despoiling of the patient, we have restarted the utilization of local cutaneous flaps associated with the mammary implant. The new employed technique has been based on the rigorous geometrical surgical principles of the Aufricht Mastoplasty(3l) and of Pitanguy's Reduction Man1ffiaplasty(32), as well as on occasional utilization of the Z-plasties over the post mastectomy scar during the placement of the mammary implant (Bostwick III)(4); finally, it has also been based on the simplicity of the technique divulged by Holmstrom(21), when he divulged the lateral thoracodorsal flap.
The objective of this work is to present our technique which has been utilized since 1996 in the breast reconstruction cases through the use of Cutaneous Flaps in Double V - according to geometrical principles associated to the Silicone Mammary Prosthesis, with the reconstitution of the nipple-areola complex and adequacy of the contralateral breast in an only surgical time (allowing an anatomical and harmonious contour of the new breast, thoracic wall and axillary region, with less surgical morbidity).
HISTORY
In the existent literature about Breast Reconstruction Surgery (which is wide and large) we can find Czerne(28) who, in 1895 utilized a giant lipoma of the patient herself to reconstruct breast that was amputated due to a benign disease. During several years, until the end of last century, the surgical principle regarding the treatment of breast malignant tumors was merely palliative, with small excisions limited to the tumor while the reconstruction of the breast would be limited to the ablated site.
When Halstead(l7) initiated the treatment of the mammary neoplasias performing the Radical Mastectomy, the patient's prognosis was changed but, in exchange to that, aggressive mutilations happened. Such fact changed the concerns of the specialists responsible for the reconstruction surgery, who started dedicating themselves to the reconstruction of the thoracic wall (which was then a site of extended lesions secondary to the big surgical excisions and, also, to the sequelas caused by the existent side treatments (radiotherapy)).
In the beginning, as an option of reconstruction, skin grafts and adjacent flaps were performed having in view only the cutaneous coating of the affected region, and the aesthetical results were poor. Several adjacent cutaneous flaps were described and several basis concerning the origin of the random cutaneous pedicles were found: superior base (Payr and Tanzini)(24), inferior base (Chardot-Carolus and Wallace-Wilson)(24) and lateral base (Pierer, Robineau, Morel Fatio among others)(24). In the beginning of the 20th century it was possible to perceive some concern with the repairing of the breast shape associated to the closure of the cutaneous tegument with local flaps (Payr, Ombredanne and Kleinshmidt)(24).
Thanks to the advent of the Filles-Filatov-Ginestet(24) cylindrical flaps, in 1916, the breast reconstruction surgery was improved by the utilization of distant cutaneous flaps - already having in view the reconstruction regarding mammary shape and volume which is specially useful in cases of extended cutaneous compromising due to radiodermitis. In 1925, GilLies Donati(24) initiated this kind of technique, followed by several other authors (Cholnoky, Fossati, Barsky, Ginestet)(24).ln 1957, Gilles-Milard(15) described the use of abdominal tubes with favorable results (with, however, high morbidity due to the several surgical times that were demanded). In 1967, Pitanguy(33) utilized tubular flaps of abdominal origin to treat hypomastias; more recently (1973), Orticochea(30) suggested the breast reconstruction With the utilization of distant flaps of the gluteal region using the hand as vector - which also received low acceptance due to the nuisance and multiplicity of surgical times involved.
Still during the transition of the century, some authors preconized the glandular-cutaneous autoplasty by using the opposing breast rotated to a single central position (called cyclopization) with terrible aesthetical results (Verneuil, Legueu, Morestin, Sauer bruch and others)(24). Based on this idea, there come the dermoglandular autoplasties by means of the division of the remaining breast, with better aesthetical results as they had the purpose of creating a new mammary volume on the reconstructed side besides preserving the adequate morphology of the donor breast (Morestin, Mir-Mir, Burian, Neumann, Reinhardt, Dufourmentel and others)(24).ln the 60s and 70s, Brazilian authors (Callia(5), Ely(12) and Pontes(35)) improved the mammary partition technique, obtaining good results for that time. In 1981, De La Plaza(8) suggested a dermoglandular transposition flap utilizing a part of the contralateral breast and thoraco-epigastric tissues.
Other kinds of reconstruction, now having as its objective the volume of the mammary cone(9), were divulged: pure glandular autoplasty (of the contralateral breast; Pierre-Bureau)(24), adipose autoplasty (Morel-Fatio)(24), dermoadipose autoplasty (Marino, Longacre, De Cholnoky and others)(24), muscular (Madeira I And Ii, Sanders)(24) and epiploic (Kiricuta, Zavaleta)(24) autoplasties.
From the second half of this century on, the oncological surgery of the breast starts tending towards less aggressiveness, with the Modified Radical Mastectomy (myoconservative) and the Subcutaneous Mastectomy(16), aLlowing better conditions of closure of the surgical wound. Therefore, the surgeons that are responsible for repairing the amputed breast persisted constantly searching for improved techniques that could allow not only the cutaneous covering but also the improvement of the local aesmetics. Within this period, several kinds of mammary implants have arisen (initially with Pangman and Gonzales-Ulloa)(24).
In the beginning of the 60s, with Cronin-Gerow, the silicone mammary implants (already divulged in Japan by the end of the 40s, by Akiyama)(24) were divulged in augmentation mammaplasties. The utilization of this kind of subcutaneous prosthesis (in the breast reconstruction of me breast surgery) was systematized in 1971, by Snyderman and Guthrie(37). In 1974, Bohmert(2) proposed an upward rotated thoraco-epigastric flap to cover a silicone prosmesis located in the neo-breast site, which is a technique widely developed and divulged by Cronin(6). From 1978 on, Radovan(36) initiated the gradual expansion of the tissues in order to create a space with enough volumetric capacity to introduce a future definitive implant; he has many followers(27, 40).
Between the 50s and the 70s, the utilization of the local dermoadipose flaps widely used in the beginning of the century (Kleinschmidt thoracolateral flap(28)) - still happens in the mammary repairing, associated or not with the use of mammary implants, as, for example: thoraco-abdominal flaps (Baroudi(1)), Boehmert(28)); thoracoscapular flaps (Longacre(26)) and deltopectoral flaps (Bakamjian(28)).
The use of myocutaneous flaps for breast reconstruction has begun with Tanzini(28) (1906) who described the technique of anterior rotation of the great dorsal major muscle and posterior graft. In 1976, Olivari(29) associated the utilization of the great dorsal major flap to the silicone prosthesis, a technique that became popular thanks to Bostwick(3), with great aesthetical advances. Drever(ll), in 1977, was me first to utilize the straight muscle of abdomen in a vertical myocutaneous flap - a surgery that was modified by Hartrampf(18) and Gandolfo(14), in 1982, by dispensing the utilization of prosthesis. In 1984, Ishii(22) used a bipedicled flap of the straight muscle of abdomen in order to guarantee a greater vascularization viability.
Lejour(25) divulged the superior transverse myocutaneous flap of the straight muscle of the abdomen, followed by Vasconez and Psillakis(38), among others.
The local or distant fascio-cutaneous flaps have also their places in the breast reconstructive surgery, as, for example: thoracodorsal fascio-cutaneous flap (Holmstrom(21) - 1983) and brachial facio-cutaneous flap (Pitanguy(34) - 1984).
During the 70s and the 80s, the adjacent muscular tissues were again utilized to provide the lost mammary volume: pectoralis major (Brown(28)); external oblique (Little(28)); serratus (Arnold(28)) and teres major( Goldfrey(28)). In 1990, with Erol and Spira(28), the use of the omentum is resumed, now with its interpositions between the skin and the abdominal subcutaneous previously autonomized.
With the advent of the microsurgery, the free muscular flaps were idealized and brought to the breast reconstruction: gluteus maximus (Fujino(13) - 1976) and tensor fasciae latae (Hill(19)) - 1978). In 1979, Holmström(20)) proposed the utilization of the inferior abdominal tissue as a free flap, with anastomosis of the periumbilical perforans vessels.
On more recent years, new techniques for tumor extirpation have also arisen and the mastologists have the option of more conservative, non-mutilating surgeries, complemented by radiotherapy and chemotherapy: the quadrantectomies(39). This way, the large myocutaneous flaps which had been developed until then became inadequate in cases of minor excisions.
Some authors (Franco, George, Petit)(7) started worrying about the reconstitution of the lesions caused by the quadrantectomies (many times in varied forms and locations) and, with Daher(7), the breast island flaps ("Plug Flaps") arose.
CASUISTRY AND METHOD
In our department, since 1996, we have been indicating, for the breast reconstruction surgeries, the utilization of Cutaneous Flaps in Double V, prepared through geometrical principles associated to silicone mammary implant. With this technique, 10 patients primarily mastectomized due to breast neoplasy, who were submitted to modified radical mastectomies (myoconservative - Patey type) and, therefore, presented preservation of the pectoral muscles and homolateral ganglionic emptying, were operated.
Six patients had had their right breasts amputated and four had had their left breasts amputated.
The quality and quantity of adjacent skin varied according to each patient, as well as the thickness of the subcutaneous cellular tissue which was thinner in two patients. None of them presented serious local sequelas due to radiodermitis.
The characteristics of the postmastectomy scar - regarding quality (normal, hypertrophied, elongated, depressed and irregular), direction (in six patients, the scar was horizontal and, in the others, it was oblique) and length - showed to be variable.
The patients' ages varied from 36 to 65. Three patients were moderate smokers.
All patients' clinical conditions (ASA I) and laboratorial exams were within normality for the perfotming of the surgical proceeding. They were also allowed by the mastologist and the oncologist to submit to breast reconstruction. The waiting time between the mastectomy and the repairing surgery for this group of patients varied from 2 to 3 years due to several reasons.
The kind of anesthesia utilized was the general anesthesia with low flux, which is routinely indicated in our department.
As a routine, the antibiotic therapy was established (3rd generation cephalosporin, in the majority of cases) until the seventh postoperative day and the use of common analgesics was symptomatic. Already during the first week after the surgery the lymphatic drainage procedures were started and the skin sutures were removed between the 10th and the 12th postoperative day, a period during which manual and mild mobilization of the prosthesis was indicated.
SURGICAL TECHNIQUE
For didactic purposes, we have divided the Geometric Principles applied during the demarcation and the surgical steps for the mammary reconstruction utilizing Cutaneous Flaps in Double V associated with the implantation of mammary prosthesis, which is described below.
1. Identification of the preexistent scar (postmastectomy) noticing, specially, its length and direction.
2. Meticulous examination of the contralateral breast by measuring, as reference values, its height and width
3. Demarcation (Fig. 1):
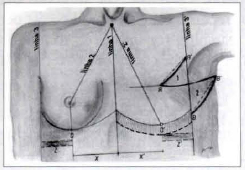
fig. 1 - Diagramatical drawing showing the lines, points, distances and flaps utilized in the surgical demarcation phase of the technique employed in breast reconstruction.
- Identification of the median point in the suprasternal regions and in the xiphoid appendix. From these, the demarcation of the median and central line called LlNE 1 (which goes from the suprasternal region up to the umbilical scar passing by the sternum xiphoid appendix) is carried out.
- following that, LINE 2 is drawn, from the same central point located in the supraesternal region, heading obliquely toward the nipple projection of the healthy breast, until it crosses the respective submammary fold (which was previously demarcated with methylene blue). At this point, it is important to emphasize that such line delineates obliquely in a downward direction until it reaches the healthy areola-nipple plaque, this way dividing the healthy glandula mamaria in two equal halves and determining a central point, called POINT 0;
- The projection of the submammary fold to be reconstructed is carried out, by following, as a basis, the marking made while the patient was still in an orthostatic position, before the surgery starts, when one can compare, more efficiently, the height of the submammary folds.
From this neo submammary fold, its inferior projection is marked (around 2 cm) - an area which, at the right moment, will also be detached from its bed;
- With the help of a caliper, one goes from the central line (LINE 1) towards POINT 0, therefore finding the DISTANCE X (Fig. 2). Such distance is repassed to the side to be reconstructed, when DISTANCE X' (which the end determines the "in mirror" projection of the POINT 0 - which on this side is called POINT 0') is determined. From this point towards the suprasternal mcdian point, the oblique line of the reconstructed side (called LINE 2') is drawn.
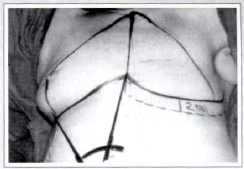
Fig. 2 - Surgical demarcation of DISTANCES X and X'.
- On the healthy side, with the help of a rule, the identification and marking of the anterior axillary line (LINE 3) follows.
Later, the distance between this anterior axillary line and POINT 0 is identified on the submammary fold (still on the healthy side), and DISTANCE Z is found.
- On the neo submammary fold, on the side to be reconstructed, one goes from POINT 0' towards the axillary region repassing "DISTANCE Z" (which, on the reconstructed side, is called DISTANCE Z'). The final point of this new distance determines the point from which the new anterior axillary line (LINE 3'), demarcated with methylene blue as well, will project itself.
- Horizontally directed, two points (POINTS A and B') are demarcated and linked by a straight line by using the axillary projection of the horizontal postmastectomy scar_and the new anterior axillary line (LINE 3'), which cross perpendicularly, as references. DISTANCE Z' corresponds, in cm, to the distance between these two points and LINE 3' (which, in this case, is central)(Fig 3).
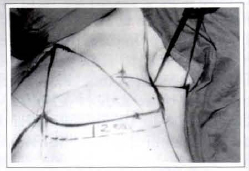
Fig. 3 - Surgical demarcation of DISTANCES Z and Z'.
- On LINE 3' (which is now vertically oriented) one utilizes the same DISTANCE Z' and demarcates points A' and B starting from the central point of its crossing with the axillary projection of the postmastectomy cicatrix.
- Once the points are demarcated, the geometrical preparation of the Z-plasty cutaneous flaps in double V (FLAPS 1 and 2) begins (figure 4). The linking of POINTS A and A', by means of an inferior convexity, slightly curved line, determines FLAP 1 (of superior base, which will be transposed to the axillary region). The linking of POINTS B and B', by means of a more accentuated inferior convexity line, determines FLAP 2 (of inferior base).
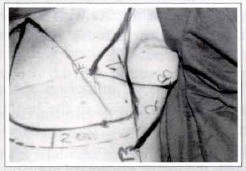
Fig. 4 - Geometrical Preparation of FLAPS 1 and 2.
- At the end of the demarcation phase, we can observe certain peculiarities of the drawn flaps which correspond to a large Z-plasty. FLAP 1 has a superior base and, after its lateral oriented transposition towards the axillary region, it will provide the axile (which was limited due to the local tissular retraction) with greater mobility and elasticity. FLAP 2 has an inferior base and, when it suffers a medial oriented rotation towards the mammary region, it will - by providing larger volumetric capacity to the region - guarantee the confection of the neo breast lateral wall (facilitated by the greater convection of the line that links POINTS BB') what is necessary for the placing of the mammary implant.
4. The surgery proceeds with the local infiltration of anesthetic solution - (containing saline solution, 0,5% lidocaine hydrocloride and 1:400.000 adrenaline) in the incision areas.
5. Following that, there is the cutaneous incision of the lines previously drawn in thee Z (segments AA', AB' and BB') (Fig. 5). The detachment of the cutaneous flaps in the subcutaneous cellular tissue, on the suprafacial plane, is meticulously carried out with the help of a n° 23 knife blade. The random flaps viability can be proved by the presence of blood flow in their edges.
Fig. 5 - Incision of the cutaneous flaps at random.
6. After performing the subcutaneous detachment of FLAPS 1 and 2, with the help of a digital maneuver, the blunt undermining of the mammary implant receptor bed (exactly located below and around of the old post mastectomy scar - Fig. 6) is performed. In this phase of the surgery the area which corresponds to the 2 inferior cm of the new submammary fold (the hachured area) is also detached in order to allow a better accommodation of the prosthesis. With the help of the optic fiber and of the electrocautery a rigorous hemostasis is then performed.

Fig. 6 - Blunt undermining of the future mammary implant "space".
7. The silicone-gel rugous mammary implant is soaked in iodopolvidona solution. In our casuistry 165 cc (1 patient), 190 cc (6 patients), 260 cc (2 patients) and 325 cc (1 patient) implants were performed in supramuscular plane and no kind of tissular tension was observed in the intraoperatory.
8. Immediately after the placing of the prosthesis, the suture is initiated and internal stitches to support the lateral wall (located right below the vertical incision and which future cicatrization will form the new anterior axillary line, located on the same level of LINE 3'), which are responsible for the lateral limit of the reconstructed organ, are performed. For that, 3 or 5 stitches are performed by using strong nylon monofilamentar thread (3-0 or 2-0) between the FLAP 2 base and the muscular fascia; through this, the prosthesis is tied to its new bed and lateral dislocations are prevented from happening.

Fig. 7 - Preparation of the neo breast lateral wall - after rotation and transposition of FLAP 2, extending toward the medial point.
9. Following that, the suture of the flaps is performed in all the Z-plasty extension by planes; subcutaneous, subdermic and cutaneous (inverted simple stitches performed with nylon 4-0 monofilament thread in the two first planes, and Gillie's stitches performed with 5-0 thread in the last plane).
The most peripheric portions of the flaps (around 1.5 to 2 cm from their edges) may be eventually stitched in V-Y preventing tensions in the suture threads.
10. The reconstructed breast may now be observed (in which concerns its position and volume) and compared to the (healthy) contralateral breast (Figs. 8-9). The next surgical time is called "adequacy of the contralateral breast". Such phase is not always necessary (there are only 2 cases in our casuistry) but, when it is performed, there are basically 3 surgical techniques that can be employed:
Fig. 8 - A view right after the rotation and transposition of FLAP 2 towards the medial point (we can notice the neobreast lateral limit, located exactly on the level of the new anterior axillary line).
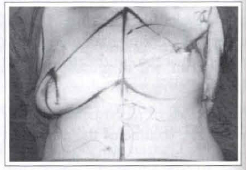
Fig. 9 - Anterior view comparison of the reconstructed breast to the contralateral breast (still not operated).
- reduction mammaplasty (5 cases)
- mastopexy (2 cases)
- augmentation mammaplasty (l case).
11. In our department, the (healthy) contralateral breast is operated through the Single Vertical Scar Technique(10) associated or not to the superficial lipoaspiration of the lateral and medial extensions. The utilization of glandular-adipose flap(9) for the packing of the Superior Pole (Souza Pinto Technique)(9, 10) is also preconized.
12. After the "adequacy of the contralateral breast", the measuring of the healthy areolanipple plaque is performed as well as the posterior transposition of the cardinal points to the reconstructed side, taking care so the center of the neo-areola (which marking is performed with the help of an areola marker) is located over LINE 2' (which is again marked within this surgical time). The correction of LINE 2' is carried out by drawing a perpendicular line leaving from POINT 0' (which is located in the new submammary fold) up to the new nipple position (located in the center of the marked cardinal points).
The height of this new perpendicular line in relation to the nipple shall coincide with the contralateral side (which breast has already passed by the "adequacy phase"). From the projection of the neo nipple, the new oblique line 2' is drawn towards the central point of the sternal furcula.
Then, the cutaneous decortication of the new areolar site is performed followed by the placing of the total skin graft taken from the root of the thigh (inguinal fold) (Fig. 10). The graft is sutured with Gillies stitches while a central apertura must be pelfonned for the placing and suturing of a contralateral nipple graft. Both grafts receive Brown's compressive dressing which is removed on the seventh postoperative day.

Fig. 10 - Decortication of the new nipple-areola plaque area.
13. Aspirating drains must be placed and removed on the day after the surgery. The dressings are performed by putting gauze over the surgical wound and Micropore tape (on the inferior part of the wound) taking care to leave the most lateral half of the mammary flap base (FLAP 2) free, allowing adequate blood irrigation and return (Figs. 11 & 12).

Fig. 11 . Comparison of the reconstructed breast with the contralateral breast, specially in terms of shape, position and volume.

Fig. 12 - Close-up view of the reconstructed breast and its dressing, where it is possible to notice the position of the central scar (located over the new anterior axillary line and which superior and inferior edges were sutured in V-Y, in this case); of the medial scar (located in the upper outer mammary quadrant); and of the lateral scar.
RESULTS
In the current segment of the Breast Reconstruction (3 to 18 months after the surgery) with the described technique, the following results can be observed (Cases 1, 2, 3 & 4):
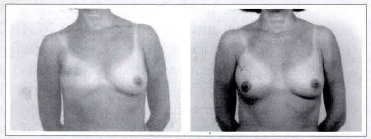
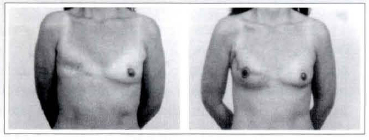
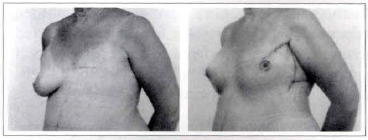
Case la - A 48-year-old patient submitted to a right breast reconstruction through the described technique (a 190 cc mammary implant). Front view: pre and postoperative.
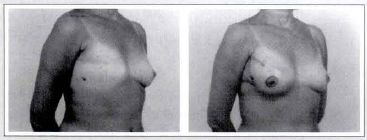
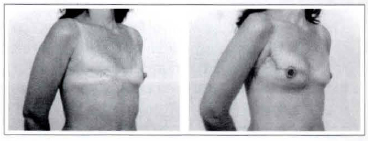
Case 1b - A 48-year-old patient submitted to a right breast reconstruction through the described technique (a 190 cc mammary implant). It is possible to see the position of scars, the shape and the volume of the reconstructed breast). Oblique view: pre- and postoperative.
Case 1c - A 48-year-old patient submitted to a right breast reconstruction through the described technique (a 190 cc mammary implant). It is possible to sec the positioned new axillary line and the greater freedom of movements of the axillary region. Proflle view: pre and postoperative.
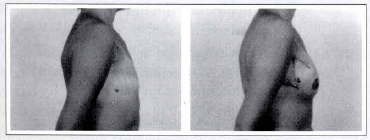
Case 2a: A 65-year-old patient submitted to a right breast reconstruction through the described technique (a 190 cc mammary implant). From view: pre and postoperative.
Case 2b: A 65-year-old patient submitted to a right breast reconstruction through the described technique (a 190 cc mammary implant oblique view: pre and postoperative.
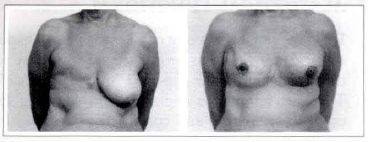
Case 3a: A 36-year-old patient submitted to a right breast reconstruction through the described technique (3 165 cc mammary implant. Front view: pre and postoperative.
Case 3b: A 36-year-old patient submitted to a right breast reconstruction through the described technique (a 165 cc mammary implant). Oblique view: pre- and postoperative.
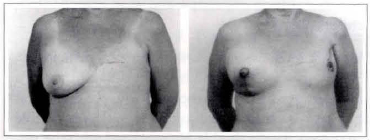
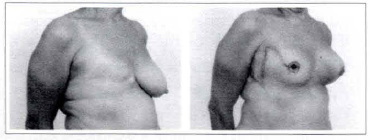
Case 4a: A 65-year-old patient submitted to a left breast reconstruction through the described technique (a 260 cc mammary implant) and reduction mammaplasty of the contralateral side. Front view: pre and postoperative.
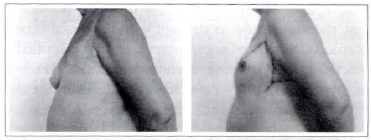
Case 4b: A 65-year-old patient submitted to a left breast reconstruction through the described technique (a 260 cc mammary implant). It is possible to notice the scars and anterior axillary line positions. Profile: pre and postoperative.
Case 4c: A 65-year-old patient submitted to a left breast reconstruction through the described technique (a 260 cc mammary implant). It is possible to notice the position of the scars, the viability of the flaps and the freedom of movements of the axillary region. Oblique view: pre and postoperative.
AESTHETICAL FUNCTIONAL
From the aesthetical point of view, the breast shapes obtained through this procedure are very close to the ideal shape of the expected "mammary cone".
The final scar of the Z-plasties end up being located in strategical and concealed positions (the greater extension of the Z is over the anterior axillary line or too close to it, on the reconstructed side). In the anterior view only a small scar segment (one of the smallest branches of the Z) can be noticed in the external superior quadrant of the breast and, as it is a local flap (same skin quality and thickness of the subcutaneous cellular tissue), no "steps" or other scar drops could be noticed.
The other branch of the Z is located on the lateroposterior thoracical wall.
In three cases we could observe the "breaking" of the old post-mastectomy scar which did not influence the aesthetical results that were obtained. Also, concerning the final results, the previous orientation of this scar (horizontal or oblique) made no difference.
From the functional point of view, we could notice greater mobility and liberation of the axillary region (thanks to rotation and transposition of FLAP 1) which movements were limited before by the own mastectomy procedure and also by local scar retractions. There is also considerable improvement of the "tissular accumulation" (skin and fat) observed in inferior position in relation to the axilla (after the mammary amputation), The quality and positioning of the lateral wall of the reconstructed breast is accomplished thanks to the rotation of FLAP 2, which is facilitated by a more convex direction of the drawn incision line.
CONTRALATERAL BREAST
The "adequacy of the healthy breast" was necessary in the cases of eight patients and was performed, with previous authorization, during the same surgical time of the breast reconstruction. Reduction mammaplasties were performed in 5 cases (up to 340 g of mammary tissue were excised), mastopexies in 2 cases and an augmentation mammaplasty in 1 case. All excised tissue was analyzed by the pathological anatomy and no signs of malignancy were found.
AREOLA-NIPPLE COMPLEX
In our casuistry, all the "areolo-nipple complexes" were reconstructed within the same surgical time: good results were reached in nine cases. In one patient, only, there was low blood supply in the central grafted nipple and its partial loss. Three cases presented slight Iateralization (around 1 to 1.5 cm) which did not affect the final aesthetical quality of the obtained result. Such problem can now be corrected through LINE 2' remarking step, described at the moment of the marking of the new areola nipple plaque.
MAMMARY IMPLANTS
The prosthesis implanted in supra-muscular space presented good mobility and did not dislocate upwards thanks, in nine cases, to the detachment of the 2 centimeters below the new submammary fold.
Only in the first case, in which we did not perform such detachment, the mammary implant was located on a higher position.
With the new mammary wall provided by the rotation of FLAP 2, the lateral restraint of the prosthesis was efficient and, even with the utilization of large volume prosthesis (260 and 325 cc) the performing of the implant was easy and no excessive tensions or tractions on the flaps were observed.
COMPLICATIONS
In two cases a little hematoma was formed and was emptied during the first dressing. Except for the low blood supply in one of the reconstructed nipples and its partial loss, and for the case in which the mammary implant was located in a higher site, there were no other kinds of complications (such as low blood supply and necrosis of the flaps - even in the cases of the two patients With thin cellular tissue or in the cases of the smokers - infections or capsular contractions due to the use of prosthesis until the present moment.
SURGICAL MORBIDITY
It is a simple performance technique, quick (45 minutes on average), secure and non-despoiling.
Seven patients were discharged from the hospital on the same day: so, the technique provides the surgery with an ambulatory character and, this way, favours its psychological aspect.
PSYCHO-EMOTIONAL
Before the reconstruction, all the patients would present (in variable levels) anxiety alternated with depressive states (which is normally expected due to the progress of the pathology itself and also due to the treatments the patients had been submitted to). For 5 of the patients (50%) the fear of having to submit to a new surgical procedure was strong enough to delay the reconstruction indication (from 2 to 3 years on average).
After being submitted to the proposed procedure, all patients experienced great change in their psychoemotional states. According to their commentaries, they considered the surgery and postoperative phases relatively simple and, also, in aesthetical terms, they liked the shape of the new obtained breast.
ECONOMICAL ASPECT
Thanks to the simplicity and quickness of the technique (which influences directly the room surgical expenses) and thunks to the fact that no specialized surgical equipment or training are necessary and to the short necessary permanence in the hospital (less than 24 hours, on average), the surgery has shown to be favourable also at the economical level.
DISCUSSION
Today, the plastic surgeon counts on a great body of surgery methods for the Breast Reconstruction(4, 28, 40); however, choosing among the several methods is still difficult and there is no single technique that may fit all the postmastectomy cases(27). We emphasize some factors that may orientate one's choice for a simpler procedure as the geometric mammary reconstruction with cutaneous flaps in double V associated to breast prosthesis:
PERFORMANCE SIMPLICITY AND SURGICAL MORBIDITY
Nowadays, the muscular flaps(24)(microsurgicall(13, 19, 20, or not) constitute one of the landmarks in the development of the Repairing Plastic Surgery, which main representative is the TRAM(l, 22, 23, 38, 40), followed by the dorsal major musclel(3, 29) and the fasciocutaneous flaps(21).
However, the surgery that deals with the transposition of flaps is not, in any center, a simple surgery: it always involves major surgical morbidity factors(27): clinical-hematological despoiling of the patient; irreversible traumas in the muscle flaps donor areas resulting in large visible scars and ab- sence of the normal function of the compromised muscle (which, in the case of the straight muscle of the abdomen, results in the compromising of the prelum abdominale since the technique is not always feasible due to previous plastic surgeries), more time at the hospital for patient recovering, larger number of postoperative complications (flap necrosis, infections, shape and scar irregularities, among others).
For such reasons, based on old surgical principles(4, 21, 31, 32), in search of the simplicity and efficacy of a less aggressive surgical method(7, 21), we looked at the past for a surgical technique (rotation of double cutaneous flap in double V associated with the implant of a mammary prosthesis) that may be performed in hospital centers fearuring minimal conditions for a small-medium procedure, with no need of sophisticated devices or specific microsurgical training for the plastic surgeon. The results obtained with this technique have shown easiness and quickness of performance and short permanence of the patient in the hospital (which is more econumical and, therefore, more consistent with the social-economical situation of our country). It can be applied practically in all patients submitted to modified radical mastectomies(34)(Patey kind) even when these patients present more oblique, almost vertical scars.
The only contraindication we could observe was the severe cutaneous radiodermitis. Another contraindication (which in this case is relative) would be the patient's refusal to submit to a silicone mammary prosthesis implant.
FUNCTIONAL AND AESTHETICAL ASPECTS
With this technique we have also accomplished adequate shape and volume for the reconstructed mammary cone, associated to the excellent local cutaneous cover (fundamental points for an efficient Mammary Reconstruction(24, 27, 28, 31)).
The neo-breast position and its adequacy to the contralateral organ have been showing a good aesthetical and simetrical value, with the scars located in concealed positions in the lateroposterior face. Except for site bearing the old mastectomy scar (which is kept in an anterior position) one can only notice (from an anterior point of view) a little scar in the upper outer mammary quadrant, proceeding from one of the small branches of the Cutaneous Flaps in Double V Z-plasty. Until this present moment, such scars have been showing to be of good quality, with no retractions, drops, hypertrophies or enlargements (which are advantages brought by the use of local tissue, which has the same skin and subcutaneous quality).
On the contraty, when muscle flaps(22, 24, 28)(microsurgical or not) are utilized, tissular drops (due to the great difference of thickness between the tissues used - specially of the subcutaneous cellular tissue - which makes a second surgical time necessary for fat removing) and scar irregularities (which, through the performed technique, can normally be found in the anterior face of the reconstructed organ) can be noticed.
From a functional point of view, the random cutaneous flaps (confected through this present technique) have been showing good safety and vascularization viability.
Still about the function: by utilizing such flaps, we have been obtaining large liberation and mobility for the axillary region (a region which, most of the times, is retracted, with limited movements, due to the kind of exeresis and cicatrization of the post mastectomy)(39).
The mammary implants, which are utilized by many authors(6, 21, 27), have been showing great capacity when it comes to supplying volume to the amputated organ. In our experience, it has not shown any complication rate.
PHYSICAL-EMOTIONAL ASPECTS
The easiness of the described technique allied to the reconstruction of all the involved clements in one time surgery (which results in a small number of internments and shorter hospital permanence time) lead to a greater acceptance of the reconstruction phase from the part of the patient (who, due to the narural course of her illness, is anxious and depressed)(27, 40). The multidisciplinary(40) caring of this pathology may (after permission from the mastologist - oncologist - radiologist and from the psychoanalyst) lead to the planning of an Immediate Reconstruction(23, 27, 40), always for the patient's psycho-emotional and economical benefit, contributing for the illness cycle of cure through the improvement of the immunological aspectl(4O) (which, nowadays, is known to be widely influenced by emotional aspects).
CONCLUSION
In an age characterized by great technological advancement in ali sectors, we must remember that the oncological cure is not limited to the neoplasia but is also directly related to the life quality it will provide to the patient. Such kind of thought applies fully in the case of mastectomized patients whose psycho-emotional aspect is more and more benefited by the aesthetical aspect allied to the funcional aspect of the wound closure (which is obtained after the reconstruction surgery).
By being entirely conscious of the multidisciplinary aspect related to the Breast Reconstruction Surgery, we have been considering the cutaneous flaps in double Vutilization (by following the described geometrical principles, allied to the mammary prosthesis implant) a simple performance surgical technique, characterized by low morbidity and economical costs, which guarantee to the patient the desired aesthetical and functional results. Besides that, it provides great help to me emotional aspect, favouring the definitive cure of a pathology that has already produced several irreparable sequelas in our society.
REFERENCES
1. BAROUDI R, PINOTII JA, KEPPKE EM. A transverse thoraco-abdominal skin flap for closure after radical mastectomy. Plast. Reconstr. Surg. 1978: 61;547.
2. BOHMERT H. Refinements in technique of the breast reconstruction with thoraco-epigatric and advancement flaps in 150 patients. Transactions of the seventh international congress of IPRS. Rio de Janeiro, 1979. p. 594.
3. BOSTWICK III J, VASCONEZ LO, JURMEWICZ MJ. Breast reconstruction after mastectomy. Plast. Reconstr. Surg. 1978; 61 :682.
4. BOSTWICK III J. Reconstruccion de la mama. In: McCARTHY JG. CIRUGIA PLASTICA TRONCO Y EXTREMlDADES INFERIORES. Buenos Aires: Panamericana Editorial Medica, 1994.
5. CALLIA WEP. Nova tecnica para reconstrução de mama em amastia unilateral. In: IV Congresso Latino Americano de Cirurgia Plastica, Sao Paulo, 1960.
6. CRONIN TD, UPTON J, MECDONAUGH M. Reconstruction of the breast after mastectomy. Plast. Reconstr. Surg. 1977; 59:1.
7. DAHER JC. Retalhos em ilha da mama (PlugFlaps). In: TOURNIEUX AAB. ATUALIZAÇÃO EM CIRURGIA PLASTICA ESTETICA (SBCPER-Regional Sao Paulo), Sao Paulo: Robe editorial, 1994. p.351-362.
8. DE LA PLAZA R. Postmastectomy reconstruction by a contralateral abdominomamary flap.Ann. Plast. Surg., 1981; 6:97.
9. DE SOUZA PINTO EB, ALMEIDA AEF, REYES MFC. Dermoadipose and adenadipose flap in mammoplasty. Aesch. Plnst. Sttrg. 1983; 7:101-108.
10. DE SOUZA PINTO EB, ERAZO PJ, MUNIZ, AC et a1. Breast Reduction: shortening scars with liposuetion. Aesth. Plast. Surg. 1996; 20:481-488.
11. DREVER JM. The epigastric island flap. Plast. Reconstr. Surg. 1977; 59:143.
12. ELY JE Organic mammary augmentation. In: FIRST CONGRESS OF THE ISAPS. Madrid: Sanches Pacheco, 1972. p. 31.
13. FUJINO T, HARASHINA T, ENOMOTO K. Primary breast reconstruction after a standard radical mastectomy by a free flap transfer. Plast. Reconstr. Surg. 1976; 58:372.
14. GANDOUF EA. Breast reconstucion with a lower abdomminal myocutaneous flap. Br. Jr. Plast. Surg. 1982; 25: 452.
15. GILLES H, MILLARD DR. Principles and Art of Plastic Surgery. V. 1. Boston : Little Brown, 1957. p.413.
16. HAAGENSEN CD. Doenças da mama. Sao Paulo : Roca, 1989. p. 889.
17. HALSTEAD WS. The result of operation for the cure of cancer of the breast performed at the John Hopkins Hospital from June, 1889 to January, 1894. Ann. Surg. 1984; 20:497.
18 HARTRAMPF CR, SCHEFLAN M, BLACK PW: Breast reconstruction with a transverse abdominal island flap. Plast. Reconstr. Surg. 1982; 69:216.
19. HTLL HL, NAHAI F, VASCONEZ LO. The tensor fascia lata myocutaneous free flap. Plast. Reconstr. Surg. 1978; 61:517.
20. HOLMSTRÖM H. The free abdominoplasty flap and its use in breast reconstruction. In: TRANSATIONS OF THE SEVENTH INTERNATIONAL CONGRESS OF THE IPRS, Rio de Janeiro, 1984. p.617.
21. HOLMSTRÖM H, LOSSING C. The Lateral Thoracodorsal Flap in Breast Reconstruction. Plast. Reconstr. Surg. 1986; 77(6):933-941.
22. ISHII JR, BOSTWICK III J, RAINE TJ, COLLEMAN JJ, HESTER. TR. Doeble pedicle transversa rectus abdominis myocutaneous flap for unilateral breast and chest wall reconstruction. Plast. Reconstr. Surg. 1985; 76:901.
23. KEPPKE EM, PINOTTI JA, MATTA SR. Reconstruções mamárias imediatas. In: RIBEIRO L. CIRURGIA PLASTICA DA MAMA, Rio de Janeiro: Medsi, 1989. p.75-85.
24. LALARDRIE JP, JOUGLARD JP. Les plasties mammaires d'augmentation et de reconstruction. In: LALARDRIE JP, JOUGLARD JP. CHIRURGIE PLASTIQUE DU SEIN, Paris: Masson et Cie, 1974. p. 183-210.
25. LEJOUR M. Reconstruction of the breast with a contralateral epigastric rectus myocutaneous flap. Chir. Plastic. 1982; 6:181.
26. LONGRACRE JT The ue of local pedicle flaps for reconstruction of the breast after subtotal or total extirpation of the mamary gland. Plast. Reconstr. Surg. 1953; 11:380
27. MAXWELL GP. Breast Reconstruction Following Mastecromy and Surgical Management of the Patient with High-risk Breast Disease. In: SMITH JW, ASTON SJ. PLASTIC SURGERY, Boston: Little Brown, 1991. p. 1203-1247
28. MENDES F, FIGUEIREDO JCA, PEREIRA WB, MÉLEGA JM. Reconstrução mamária: uma revisão e classificação de tecnicas. In: TOURNIEUX, AAB, CURl MM. ATUALIZAÇÃO EM CIRURGIA PLÁSTICA - SBCP, São Paulo: Robe editorial, 1996. p. 341-351.
29. OLIVARI N. The latissimus flap. Br: Jr: Plast. Surg. 1976; 29:126.
30. ORTICOCHEA M. Use of the buttock to reconstruction the breast. Br. J. Plast. Surg. 1973; 26:304.
31. PICK JE Mamas (Mastoplastia). In: PICK JE CIRURGIA REPARADORA, PRINCÍPIOS, PROBLEMAS, METODOS, Barcelona: Salvat, 1955. p.455-478
32. PITANGUY I. Mammaplastia - Estudo de 245 casos consecutivos de Mamaplastia e Apresentação de Tecnica Pessoal. Ver. Bras. Cir. 1961; (out) 201-220.
33. PITANGUY I, FRANCO T. As hipomastias e seu tratamento cirurgico. Hospital (Rio de Janeiro), 1967; 72:1317-1334.
34. PITANGUY I, CALDEIRA AML, ALEXANDRINO A, TREVINO MN, CALIXIO CA. Retalho braquial fasciocutâneo - tecnica de Piranguy para deformidade infraclavicular pos mastectomia. Rev. Bras. Cir. 1984; 74:349.
35. PONTES R. Single stage reconstruction of the missing breast. Br. J. Plast. Surg. 1973; 26:377.
36. RADOVAN C. Breast reconstruction after mastectomy usina the tempory expander. Plast. Reconstr. Surg. 1978; 69:195.
37. SNYDERMAN RK, GUTHRIE RH. Reconstruction of the female breast following radical mastectomy. Plast. Reconstr. Surg. 1971; 47:565.
38. VASCONEZ LO, PSILLAKIS JM, GEBEIK RJ. Reconstruction following mastectomy with a contralateral rectus abdominis myocutaneous island flap. Plast. Reconstr. Surg. 1983; 71:668.
39. VERONESI U et al. Comparison of Halsted Mastectomy with Quadrantectomy, Axillary dissection and Radiatherapy in Darly Breast Cancer: Long Term Results. Eur. J. Cancer Clin. Oncol. 1986; 22(9): 1085-1089.
40. VIEIRA R, KOGUT J. Reconstrução mamária tardia. In: RIBEIRO L. CIRURGIA PLASTICA DA MAMA, Rio de Janeiro: Medsi, 1989. p.87-111.
I - Head of the Plastic Surgery Department of Universidade Santa Cecília. Santos - São Paulo, Brazil.
II - Assistant Surgeon of the Plastic Surgery Department of Universidade Santa Cecília. Santos - São Paulo, Brazil.
III - Assistant Surgeon of the Plastic Surgery Department of Universidade Santa Cecília. Santos - São Paulo, Brazil.
IV - Plastic Surgeon of the Plastic Surgery Department of Universidade Santa Cecilia. Santos - São Paulo, Brazil.
V - Resident of the Plastic Surgery Department of Universidade Santa Cecília. Santos - São Paulo, Brazil.
Address for correspondence:
Centro Cientifico Brasileiro de Cirurgia Plástica
Av. Ana Costa, 120
11060-000 - Santos - SP - Brazil
Phone: (5513) 234-1234 - Fax: (55 13) 233-6028
e-mail: desouza. pinto@bsnet.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter