

Articles - Year 1999 - Volume 14 -
Local Injection of Hyaluronidase in Increasing Skin Flap Survival: An Experimental Study
Injeção Local de Hialuronidase para Aumento da Sobrevivência de Retalhos Cutâneos - Estudo Experimental
ABSTRACT
Previously, clinical observations have suggested that local injection of hyaluronidase (HDL) increase skin flaps survival(23). We have now extended these observations, analyzing the effects of HDL in rabbit skin flaps. Therefore, dorso-lateral, cranially pedicled skin flaps were treated with 1 ml HDL (200 U/ml, treated flaps) and compared, after 7 days of surgery, with flaps injected with 1 ml saline (control 1) or no injected at all (control 2). The efficiency of HDL was confirmed by the percentage of necrosis in the flap area (evaluated by tissue color and capillary filling) which achieved 1.47% ± 2.91) 27.64% ± 25.89 and 30.14% ± 27.96 in the treated groups, control 1 and control 2 flaps respectively. We conclude that HDL is capable of preventing skin flaps necrosis.
Keywords: Hyaluronidase and skin flaps; skin flaps survival; skin flaps.
RESUMO
Observações clínicas realizadas previamente pelo autor senior(23) sugeriram que a injeção local de hialuronidase (HLD) aumenta a sobrevivência de retalhos cutâneos. Neste trabalho experimental, analisamos os efeitos da HLD em retalhos cutâneos de coelhos. Para tanto comparamos, após 7 dias da cirurgia, retalhos dorsolaterais de pedículo craneal, injetados diariamente com 1 ml de HLD (200 U/ml, retalhos tratados, com retalhos injetados diariamente com 1 ml de soro fisiológico (controle 1) e com outros não injetados (controle 2). A eficiência da hialuronidase foi confirmada pela percentagem de necrose nos retalhos (avaliada pela cor e enchimento capilar) que chegou a 1,47% ± 2,91, 27,64% ± 25,89 e 30,14% ± 27,96 nos grupos tratado, controle 1 e controle 2 respectivamente. Concluímos que a HLD é capaz de prevenir necrose em retalhos cutâneos.
Palavras-chave: Hialuronidase e retalhos cutâneos; sobrevivência de retalhos cutâneos; retalhos cutâneos
The survival of large skin flaps is a goal to be reached and many surgical investigators have studied the action of many substances, like vasoactive drugS< 6, 9, 10, 11, 14), antioxidants(8), corticosteroids(22) and enzymes including hyaluronidase(16).
Since 1929 hyaluronidase, the "spreading factor", has its pharmacologic properties thoroughly studied(l2, 21). It has been identified as a mucolytic enzyme, whose main
action is de polymerization and hydrolyzation of hyaluronic acid, a polysaccharide which is an essential component of intercellular ground substance(20).
In the early fifties, hyaluronidase was clinically used for the first time in intravenous high doses to treat patients with cerebral edema(25). Soon afterwards, the enzyme was used in cases of acute myocardial infarct, apparently acting by reducing intramyocardial edema(l8, 19). In 1988 important actions of hyaluronidase upon extracelular matrix macromolecules were shown in an experimental model using the rabbit skin(15). In this work, the intradermal injection of the enzyme degraded dermal proteoglycans and, due to the endoglycosarninidase activity, dissociated collagen bundles, which was followed by resynthesis of the initially degraded proteoglycans. On the other hand, the elastic fibers network was not altered.
Recently, the enzyme was also used yet in hypodermoclysis in patients with advanced cancer(5).
Several srudies using either subcutaneous or intradermal hyaluronidase in areas or around areas of venous extravasation of toxic substances like nafcilin(26), CaCl2(24), hypertonic saline and sodium tetradecyl-sulfate used in sclerotherapy(27, 28), vinca-alcaloids and another cytotoxic drugs(3, 4) demonstrated the effectiveness of hyaluronidase in preventing necrosis.
In the present paper hyaluronidase was injected directly in the skin and subcutaneous tissue of large skin flaps in an attempt to increase the connective tissue permeability, what was supposed to increase the flow of interstitial fluid to the flap proximal end. This was expected to improve the washout of metabolites from the flap extremity to more distant areas with normal vasculature, which might lead to prevention of necrosis of the flap. In the studied model, hyaluronidase proved to be an effective treatment in the prevention of necrosis.
MATERIAL AND METHODS
Eighteen New Zeland female rabbits, weighing between 2500g - 3000g were used. They were maintained under equal conditions. Anesthesia consisted of intramuscular administration of ketamine (25mg/ kg), diazepan (lmg/kg) and atropine (lml), followed by shaving of skin and antisepsis with povidine and alcohol. The experimental model was a latero-dorsal randomized skin flap with a cranial pedicle measuring 12.5 cm x 2.5 cm. Each flap was undermined and replaced in its original site and anchored with a continuous 3.0 monofilament nylon suture (Figs. 1 & 2).

Fig. 1 -The inner surface of an W1dermined flap.

Fig. 2 - The flap surured in its bed.
The study was divided into 2 groups of 9 animals. Group I received two flaps in each animal in the same surgical act. One flap, randomly selected, was injected with the enzyme (HLD 200 U/lml/day - treated flaps) and the contralateral flap injected with saline solution (1 ml/day - control 1 flaps) (Figs. 3 & 4). Approximately 1 ml of the HLD solution, was injected over the two distal thirds of the flap divided in 0.1 ml intradermal injections, and in the same manner with the saline solution in the other side. The injections were carried over during seven days, over periods of 24 hours. In group II (control 2 flaps) each animal had one flap, observed during seven days without any type of treatment.

Fig. 3 - Injection of HLD solution in the two distal thirds of a treated flap.

Fig. 4 - Injection of saline solution in a control-l contralateral flap.
The colour and capillary filling of the flaps were daily observed.
On the seventh postoperative day, the necrotic and surviving area were measured.
STATISTICAL ANALYSIS
The paired Student's t-test was used for the statistical analysis comparing the difference in survival of the flaps between the treated and control 1 flaps. In the case of controll vs control 2 comparison, the non-paired Student's t-test was applied.
Results were expressed as mean ± standard deviation and were considered significant at a 95% confidence level (p < 0.05).
RESULTS
The aim of this work was to evaluate the effects of hyaluronidase on the survival of skin flaps. For this purpose, controlled experiments were carried out in rabbits in which large skin flaps were injected with fixed concentration of the enzyme and checked at variable periods of time for the presence of necrosis.
Different non-paired control conditions were adopted: flaps injected with saline, named cantral l flaps (or Cl), and non-injected flaps, referred to collectively as control 2 flaps (or C2). Both necrosis incidence as well as necrosis extension were undistinguishable between Cl and C2, as presented in Table I and exemplified in (Fig. 5). In experiments in which flaps were treated with HLD (paired with Cl and C2) incidence as well as the extent of necrotic lesions were dramatically decreased as exemplified in Fig. 6 and represented graphically in Fig. 8 (data in Table I).


Fig. 5 - Different ranges of necrosis in the distinct control situations: 5a - C1-flap 25 % necrosed. 5b - C1-flap 75% necrosed. 5c - C2-flap 70.3 % necrosed. 5d - Islands of focal necrosis corresponding to 44.4% of a C2-flap.

Fig. 6 -Different evolution of the treated (T) flaps : 6a - 6% necrosis showed after one week. 6b - 6.6% necrosis.showed after two weeks. 6c - T-flap suffering distal extremity in the 3rd day. 6d - The same flap of 6c showing color change and complete survival in the 7th day. 6e - Dark color in distal extremity of a T-flap, in the 3rd day. 6f - The same flap of 6e, normal aspect in the 7th day.

Fig. 8 - Graphical representation of the necrosis extension, experimentally determined in HLD - treated flaps (T), in saline injected (Cl) and non-injected (C2) controls. Parenthesis present the number of flaps. Necrosis is virtually absent in treated flaps, as judged by the relatively high and comparable levels of necrosis in both control conditions (Cl and C2).
Only two rabbits out of 9 tested presented necrosis of their third ending, in approximately 6% of its length (Fig. 6). In additional cases, color alterations reversed, followed by flap survival and recovery during the first week (Fig. 6). Epidermolysis, commonly taken as a superficial necrosis, was observed once in treated flaps, and followed by a cutaneous recovery after two weeks (Fig. 7).
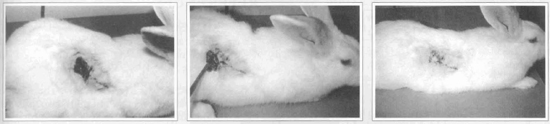
Fig. 7 - Epidermolysis in a treated flap followed by a complete cutaneous recovery: 7a - The epidermal necrosis in its place over the distal third of the flap.7b - The died tissue beeing excised in the 14th day. 7c - The flap with normal skin in its extremity and almost completely cured.
DISCUSSION
Local necrosis is known to represent a common consequence of plastic surgery. Although efforts have concentrated on investigation of possible pharmacological and/or surgical alternatives to circumvent it in different experimental and clinical models, as confirmed in the scientific literature(l, 2, 7, 13, 17), a safe and efficient maneuver able to prevent acute necrosis of large skin-flaps is yet to be developed. Hyaluronidase is an enzyme that reduces or prevents tissue injury presumably by causing the rapid diffusion of extravasated fluids to distant areas(3, 4, 24, 26, 27, 28), thus allowing a better turnover of nutrients. The rapid diffusion of fluids is been attributed to a temporary degradation of tissue cement by hyaluronidase(26), leading to a capillary and intersticial leakage of nutrients and metabolites and increasing the rate of cell nutrition.
Our study analyzed the effects of hyaluronidase on rabbit skin flap after 7 days of surgery. The data showed a significant reduction in the incidence of necrosis in the treated (hyaluronidase) group as compared with the cantral l (saline) group, suggesting that hyaluronidase was effective in improving flap survival. The possibility that the protective effects could be due to saline itself, currently employed as a vehicle to hyaluronidase,was clearly refuted as no significant necrosis prevention was detected in our experimental model and which prevalence (% necrosis, Table I) was comparable to that determined in the non-injected group (C2).
Moreover, the present experimental results substantiate preliminary clinical observations(23) showing that hyaluronidase was effective in improving the survival of larger skin flaps. Although the biochemical and histological basis for hyaluronidase protective effects are yet to be clarified, we believe that the clinical employment of this enzyme in Plastic Surgery must be regarded seriously.
REFERENCES
1. ADAMSON JE, HORTON CE, CRAWFORD IIW, et al. Srudies on the action of dimethyl sulfoxide on the experimental pedical flap. Plast. Reconstr. Surg. 1967; 39:142.
2. ARTURSON C, KHANNA NN. The effects of hyperbaric oxygen, dimethyl sulfoxide, and complamin on the survival of experimental skin flaps. Scand. J. Plast. Reconstr. Surg. 1970; 4:9.
3. BERTELLI G, DINI D, FORNO GB, GOZZA A, SILVESTRO S, VENTURINI M, ROSSO R, PRONZATO P. Hyaluronidase as an antidote to extravasation of vinca-alkaloids: clinical results. J. Cancer Res.Clin. Oncol. 1994; 120:8-505.
4. BERTELLI G. Prevention and management of extravasation of cytotoxic drugs. Drug. Saf. 1995; 12:4-245.
5. BRUERA E, DE STOUTZ ND, FAINSINGER RL, SPACHYNSKI K, SUAREZ ALMAZOR M, HANSON J. Comparison of two different concentrations of hyaluronidase in patients receiving one-our infusions of hypodermoclysis. J. Pain Symptom Manage. 1995; 10:7,505-9.
6. CHEFFE MR, ZABEL A, ZAPATA J, ARAUJO M, CHEFFE LO. The use of buflomedil and pentoxifylline in increasing skin flap survival: a comparative study. Rev. Soc. Bras. Cir. Plast. Est. e Rec. 1996; 11:1,7-12.
7. CHERRY G, GRAVV W. The effect of isoxuprine on muscle and skin flap survival in the pig. Plast. Surg. Forum.1975 ; 2:156.
8. COSTA IR. Increase in survival time of pedicule flaps with manitol (an experimental study). Rev. Soc. Bras. Cir. Plast. Est. e Rec. 1996; 11:135-44.
9. DIAS LC, FOUSTANOS A, CARREIRÃO S, PITANGUI I. Ação farmacológica do cloridrato de buflomedil na vascularização dos transplantes livres de retalhos cutâneos. In XXI CONGRESSO BRASILEIRO DE CIRURGIA PLASTICA. 1984; 18-22.
10. DIAS LC, FOUSTANOS A, CARREIRÃO S, SOUZA FILHO S, PITANGUY I. Influencia do buflomedil na viabilidade de retalhos cutâneos. Rev. Bras. Cir. 1990; 80:2,49-55.
11. DONCATTO LF, POZZAN R, RIBEIRO L, ACCORSI JR. A Ritidoplastia e abdominoplastia em pacientes fumantes: uso de droga vasoativa na prevenção de necrose do retalho. Rev. Bras. Cir. 1990; 80:2,111-115.
12. DURAN-REYNALS F. The effect of extracts of certain organs from normal and immunized animals on the infecting power of vaccine virus. J. Exper. Med. 1929; 50:327.
13. FINSETH F, ADELBERG MG. Prevention of skin flap necrosis by a course of treatment with vasodilator drugs. Plast. Reconstr. Surg. 1978; 61:738.
14. GALLA TJ, BARKER JH, SAETZLER RK et al. Increase in skin flap survival by the vasoactive drug buflomedil. Plast. Reconstr. Surg. 1989; 87:130-138.
15. GODEAU G, ROBERT AM. Action of testicular hyaluronidase on macromolecules of the cutaneous extracellular matrix. Study by computerized image analysis. Pathol. Biol. 1988; 36:6,833-8.
16. GROSSMAN JA, MCGONAGLE BA, DOWDEN RV, DINNER MI. The effect of hyaluronidase and dimethyl sulfoxide (DMSO) on experimental skin flap survival. Ann. Plast. Surg. 1983; 11:3,223-6.
17. KOEHNLCIN JE, LEMPERLE G. Experimental studies on the effect of dimethyl sulfoxide on pedicle flaps. Surgery. 1970; 67:672.
18. MARTINS DE OLIVEIRA J, CARBALLO R, ZIMMERMAN HA. Intravenous injection of hyaluronidase in acute myocardial infarction. Preliminary report of clinical and experimental observations. Amer. Heart J. 1959; 57:712.
19. MARTINS DE OLIVEIRA J, LEVY MN. Effect of hyaluronidase upon the water content of ischemic myocardium. Amer. Heart J. 1960; 60:106.
20. MEYER K. The action of hyaluronidase on hyaluronic accid. Ann. New York Acad. Sc. 1950; 52:1021.
21. McCLEAN D. The influence of testicular extract on dermal permeability and the response to vaccine virus. J. Pathol. & Bact. 1930; 33:1045.
22. NAKATSUKA T, PANG CY, NELIGANP et al. Effect of glucocorticoid treatment on skin capilary blood flow and viability in cutaneous and myocutaneous flaps in the pig. Plast. Reconstr. Surg. 1985; 76:3, 384.
23. PIMENTEL LAS. Injeção local de hialuronidase na prevenção e tratamento de necrose em retalhos cutaneos-nota previa. In XI CONGRESSO IBERO-LATINO-AMERICANO E XXXIII CONG. BRAS. DE CIR. PLAST. 1996; 05-11.
24. RASZKA JR. WV, KUESER TK, SMITH FR, BASS JW The use of hyaluronidase in the treatment of intravenous extravasation injuries. J. Perinatol. 1990; 10:2,146-9.
25 . SA EARP FA. Arq. Brasil. Med. 1954; 14:217.
26. ZENK KE, DUNGY CI, GREENE GR. Nafcillin extravasation injury. Use of hyaluronidase as an antidote. Am. J. Dis. Child. 1981; 135: 12, 1113-4.
27. ZIMMET SE. The prevention of cutaneous necrosis following extravasation of hypertonic saline and sodium tetradecyl sulfate. J. Dermatol. Surg. Oncol. 1993; 19:7,641-6.
28. ZIMMET SE. Hyaluronidase in the prevention of sclerotherapy-induced extravasation necrosis. A dose-response sudy. Dermatal. Surg. 1996; 22:1, 73-6.
I - Member SBCP - Clinica Luiz Pimentel - Niterói - Rio de Janeiro - Brazil.
II - Associate Professor - Instituto de Biofisica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro - Brazil.
Address for correspondence:
Clinica Luiz Pimentel
R. Nilo Peçanha, 59
24210-480 - Niterói - RJ Brazil
Phone: (55 21) 620-6018
Work performed at Instituto de Biofisica Carlos Chagas Filho, UFRJ, Cidade Universitaria, Ilha do Fundão - Rio de Janeiro - RJ - 21940-900, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter