

Case Report - Year 2018 - Volume 33 -
Reinsertion of traumatic avulsion of the superficial and deep flexor tendons of the little finger using the pull-out technique
Reinserção de avulsão traumática dos tendões flexor superficial e profundo do dedo mínimo pela técnica de "Pull Out."
ABSTRACT
Simultaneous closed traumatic avulsion of both the deep flexor tendon and the superficial flexor tendon of the fingers is rare, and only nine cases have been reported in the literature since 1984. Several surgical procedures for repairing flexor tendon lesions have been described, but there is no consensus on the best approach to reinsert the tendon. We report the case of a patient who suffered a traumatic avulsion of the superficial flexor tendon and the deep flexor tendon of the fifth finger, which was surgically treated using the pull-out technique.
Keywords: Wounds and injuries; Tendons; Rupture; Reconstructive surgical procedures; Hands
RESUMO
A lesão fechada simultânea por avulsão do tendão flexor profundo e do tendão flexor superficial dos dedos é rara, tendo sido relatados somente nove casos na literatura desde 1984. Foram descritas diversas técnicas para o reparo cirúrgico da lesão dos tendões flexores, todavia, sem um consenso sobre a melhor forma de reinserção do tendão. Relatamos o caso de um paciente que sofreu avulsão traumática do tendão flexor superficial e do tendão flexor profundo do 5º dedo, que foi tratado cirurgicamente pela técnica de Pull-Out.
Palavras-chave: Ferimentos e lesões; Tendões; Ruptura; Procedimentos cirúrgicos reconstrutivos; Mãos
INTRODUCTION
The flexor tendons are divided into five zones, as proposed by Verdan. Zone I extends from the insertion of the superficial flexor tendon (also known as flexor digitorum superficialis; FDS) to the insertion of the deep flexor tendon (also known as flexor digitorum profundus; FDP), including pulleys C3 and A51. Injuries in zone I only affect the deep flexor tendon of the finger and are relatively common and prevalent in younger populations and athletes. The trauma is usually caused by closed lacerations or avulsions, occurring more frequently in the fourth and fifth fingers of the hand1,2.
Zone II consists of the region between pulley A1 and the beginning of zone I. This zone includes the osteofibrous tunnel and Camper’s chiasm, known as Bunnell’s no man’s land, due to the high risk of complications after tendon injuries, such as adhesions and re-ruptures1.
The objective of this study is to describe the rare case of a patient who suffered a traumatic avulsion of the superficial and deep flexor tendons of the fifth finger, in zones 1 and 2 of Verdan, respectively, and was surgically treated using the pull-out technique described by Bunnell3.
CASE REPORT
A 25-year-old man was admitted to the emergency room as a result of trauma on the fifth finger of his left hand that occurred during a football match on the previous day while trying to hold another player’s shirt. On physical examination, he felt pain in the palmar area and presented edema and inability to flex the proximal and distal interphalangeal joints of the fifth finger, with no alterations of the neurovascular status.
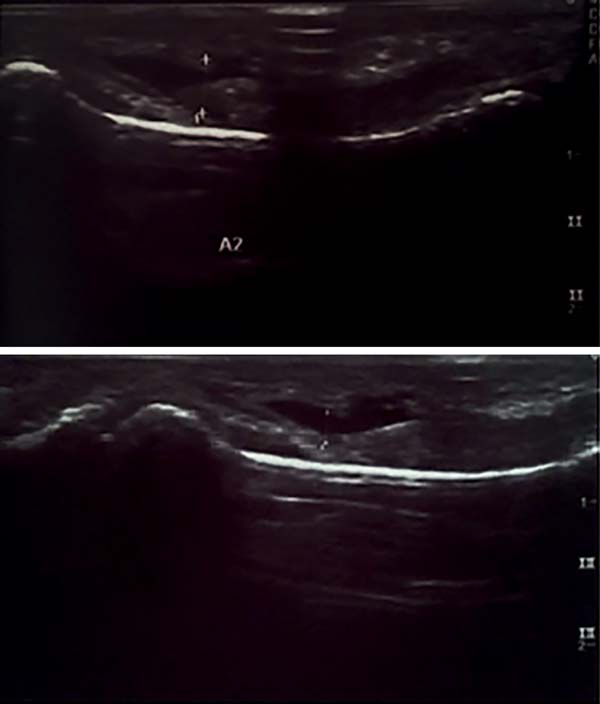
Urgent radiographs were taken, confirming bone integrity. An ultrasound of the finger showed total rupture of the superficial and deep flexor tendons of the fifth finger with tendon retraction (Figure 1).
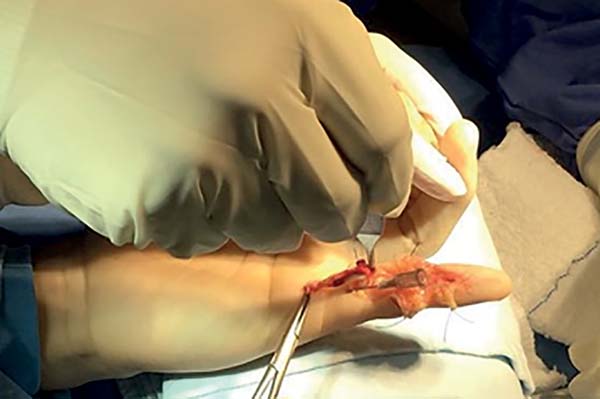
The surgery was performed with the patient under sedation, with brachial plexus nerve block and ischemia of the left upper limb. The palmar area of the fifth finger was accessed through a Brunner’s Z-type incision and complete disinsertion of the superficial and deep flexor tendons was observed (Figure 2). After repairing the tendon stumps with a Krackow suture with Nylon 4-0, bone tunnels were made in the middle and distal phalanges with a 1.0-mm K-wire.
Using a hypodermic needle 40 x 12, the repair wires of the tendon stumps were crossed to the dorsal region of the phalanges, which were fixed to their respective insertion regions using the pull-out technique with the aid of “knobs” made with the base of a 10 mL syringe (Figure 3). Lastly, pulleys A3 and A5 were repaired. A dressing was applied after suturing, followed by immobilization with a dorsal splint with 10º of wrist extension and 90º flexion of the metacarpophalangeal joints (Figure 4).
The protocol described by Duran was followed and dorsal immobilization was maintained for six weeks, with changes every 15 days and progressive extension of the splint. During the 6th week, the immobilization was removed and physical therapy with a hand therapist was started.
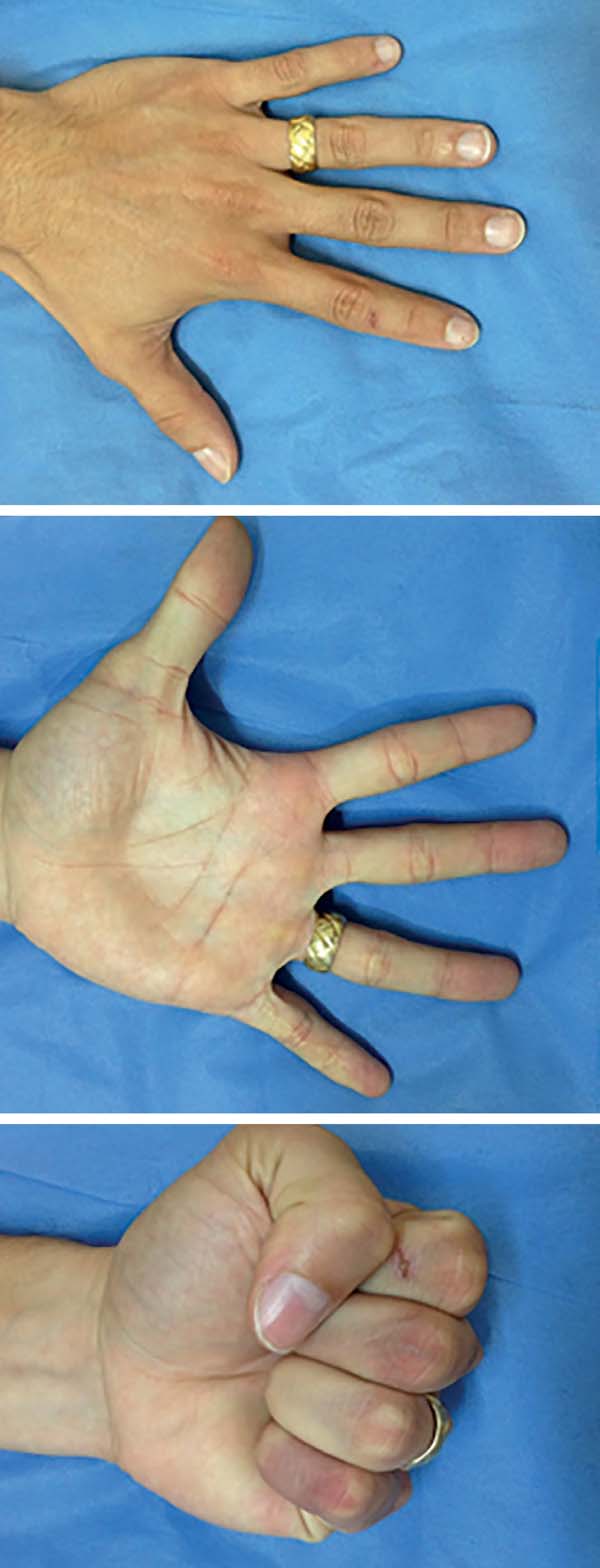
One year postoperatively, the patient was asymptomatic, the scars had improved appearance, and there were no tendon adhesions. The sensitivity remained unchanged and the functional range of motion of the finger joints were as follows: proximal interphalangeal joint (PIPJ) 10-90º, distal interphalangeal joint (DIPJ) 10-85º, metacarpophalangeal joint (MCPJ) 0-90º (Figure 5). This result is considered good by the scale of the American Society for Surgery of the Hand (ADM > 75%) and excellent by the Strickland’s adjusted scale4.
DISCUSSION
Avulsion injuries of the deep flexor tendon at its insertion at the base of the distal phalanx of the fingers is common, especially in athletes and men, with a prevalence for the ring finger that accounts for 75% of these lesions5. Conversely, injuries in the superficial flexor tendon of the fingers are uncommon and mainly affect the ring or middle finger5. A closed lesion of both tendons is rare and only nine cases have been described in the literature since 19846.
Of those cases, all patients were men, with ages ranging from 16 to 49 years (mean of 26.9 years). There were seven cases with one affected finger (ring finger in four cases, middle finger in one case, little finger in two cases), one case with two affected fingers (ring and little fingers) and one case with three affected fingers (index, middle and ring fingers)6. In our case, in agreement with the small epidemiology available in the literature, the patient was male, young (25 years old) and only the little finger was affected.
Regarding the mechanism of trauma, the most common, which occurred in three of the nine patients with injuries in both tendons, was the Jersey finger (term created to denote the closed lesion of the deep flexor tendon at its insertion at the distal phalanx of the finger as it is common among American football and rugby players when trying to hold the opponent’s shirt or jersey)6. The same was reported by our patient who was injured during a football match.
Direct trauma occurred in one case, as did repetitive microtrauma. Traction-hyperextension occurred in two cases. In all cases, except for one, the injury of the FDS occurred in zone 26. In the study by Soro et al.6, the rupture occurred in zone 3. Regarding the FDP, the tendon was affected in zone 2 in two cases and in zone 1 in all other cases.
Radiographs of the affected finger should always be requested to evaluate the presence of fractures in the phalanges. Imaging tests, such as ultrasound and magnetic resonance imaging (MRI), help diagnose where the tendons have been damaged, facilitate the surgical approach, and prevent exploration to locate the ruptured tendon stump1,2,5.
In the present case, the radiographs of the little finger discarded the presence of fractures and the ultrasound helped us to diagnose the simultaneous rupture of the tendons and allowed us to properly plan the surgery. Of the previous reports, only Toussaint et al.7 used preoperative ultrasound as a tool for diagnosis, facilitating the surgical procedure performed.
Several techniques have been described in the literature to repair flexor tendons, but a consensus on the best approach to reinsert the tendon does not exist. Some studies have reported that the pull-out technique is associated with a great number of complications. Kang et al.8 reported a 22% infection rate and abnormal nail growth in 35% of patients.
In fact, a button can hinder personal hygiene, get stuck in clothes, and cause pain and necrosis in the skin via the pressure and injury of the nail bed if it is fixed very proximally at the reinsertion of the FDP. In our case, the patient underwent surgery two days after the injury and the technique was performed according to the description of Bunnell3 in both flexor tendons of the fifth finger, with the patient progressing without complications until the buttons were removed.
Of the cases described with the simultaneous injury, the pull-out reconstruction was performed in five of the six cases operated acutely, but the FDS was resected in two cases. In one acute case, the repair was performed in two stages, with excision of the tendons in the first stage and the use of the graft of the long palmar as graft for reconstruction after nine weeks.
The surgery was performed between 0-4 days for all patients treated acutely. In two cases, the reconstruction was performed sub-acutely, with the surgery taking place 14 and 20 days after the injury. In the first case, the end-to-end repair of the FDP and resection of the FDS were performed. In the other case, the two-stage repair with the long palmar graft was used. In the only case treated chronically, four weeks after the injury, a long palmar graft was used for reconstruction6.
In seven of the nine cases described, the authors stated that their patients returned to work, with good function of the injured fingers, even in late tendon reconstructions, in two stages. In eight cases, the authors cited some stiffness or limited mobility of the distal interphalangeal joint, without significant functional impairment of the finger.
The result was described as good or excellent in five of the cases. In four cases, the authors have the opinion that the result was not good because the injury of the FDP occurred in zone 2 or due to dilaceration in zone 16. Our patient, despite the partial loss of flexion of the DIPJ, evolved with a complete return to his military activities without limitations.
Since various surgical techniques were used in the cases previously described, there is no consensus on the best approach to treat the injury. We believe that the most anatomical reconstruction possible, with the repair of the two damaged tendons, allows a better functional result. In agreement with our opinion, in three of the published cases, the FDS and FDP were reinserted with excellent functional results and minimal loss of movement6.
Evaluating the three cases in which the FDS was resected, our treatment option is confirmed. One evolved with rigidity of the DIPJ and PIPJ; another remained with limited range of motion in all operated finger joints (MCPJ, PIPJ and DIPJ); and the third case, which included two injured fingers, evolved with limited movement and residual flexion in the interphalangeal joints of both fingers (DIPJ 15º, PIPJ 10º in the ring finger and DIPJ 10º and PIPJ 40º in the little finger). Thus, we defend that treatment a few days after the injury, absence of fractures, pull-out technique, and a physiotherapeutic program favored the result, even in zone 2.
The injury of the deep flexor tendon was firstly classified by Leddy and Packer into three types based on the level of retraction of the proximal stump and the presence and size of the avulsed bone fragment9. Subsequently, new subtypes were added to the original classification (types 4, 5A, 5B, and 5C). Recently, Azeem et al.10 created a more comprehensive classification (Chart 1) to facilitate the understanding of the injury pattern, and thus, provide the most appropriate treatment for a better outcome.
| Type I | Isolated avulsion of the FDP tendon without fracture of the distal phalanx |
| Type Ia | Avulsion of the tendon and retraction up to the PIPJ |
| Type Ib | Avulsion of the tendon with a minimum bone fragment that prevents retraction of the tendon up to the palm of the hand |
| Type Ic | Avulsion of the tendon and retraction up to the palm of the hand |
| Types II and III | Avulsion associated with fracture of the distal phalanx |
| Type IIa | Avulsed tendon adhered to a single bone fragment of the distal phalanx, extra-articular |
| Type IIb | Avulsed tendon adhered to a single bone fragment of the distal phalanx, intra-articular |
| Type IIc | Avulsed tendon adhered to a bone fragment of the distal phalanx, intra or extra-articular, with dorsal cortical fracture |
| Type III | Similar to type II, but with secondary retraction of the tendon of the avulsed bone fragment, adhered or not to another bone fragment |
| Type IIIa | Incarcerated tendon on pulley A4 |
| Type IIIb | Retraction of the tendon up to the palm of the hand |
| Type IIIc | Fracture of the distal phalanx with joint involvement |
| Type IIId | Fracture of the distal phalanx with dorsal cortical involvement |
These authors state that their classification is more comprehensive and includes all injury patterns of the flexor tendons. However, the injury described in our case with avulsion of the FDP associated with the FDS is not present in Azeem’s classification10. We believe that the combined injury of the flexor tendons could be included as a new subtype of this classification.
CONCLUSION
Simultaneous avulsion via closed trauma of the superficial and deep flexor tendons of the fingers is rare and only nine cases have been described in the literature. Despite the good results presented previously, different techniques were used by each author; thus, it is not possible to define the best approach to treat the injury. In this case report, the pull-out technique, originally described by Bunnell, associated with a specific protocol, provided adequate fixation of both tendons, with low cost, and an excellent functional result.
COLLABORATIONS
|
HM |
Analysis and/or interpretation of data, data collection, design of the study, project management, research, methodology, performing surgeries and/or experiments, writing - preparation of the original, writing - review and editing. |
|
CG |
Final approval of the manuscript. |
|
IC |
Final approval of the manuscript. |
|
JLD |
Final approval of the manuscript. |
REFERENCES
1. Azar FM, Canale ST, Beaty JH. Campbell's Operative Orthopaedics. 13th ed. Philadelphia: Elsevier/Mosby; 2016.
2. Green DP, Hotchkiss R, Pederson W, eds. Green's Operative Hand Surgery. 7th ed. New York: Churchill Livingstone; 1999. p. 1877, 81.
3. Bunnell S. Primary repair of severed tendons: the use of stainless steel wire. Am J Surg. 1940;47(2):502-16.
4. Libberecht K, Lafaire C, Van Hee R. Evaluation and functional assessment of flexor tendon repair in the hand. Acta Chir Belg. 2006;106(5):560-5.
5. Netscher DT, Badal JJ. Closed flexor tendon ruptures. J Hand Surg Am. 2014;39(11):2315-23.
6. Soro MA, Christen T, Durand S. Unusual Closed Traumatic Avulsion of Both Flexor Tendons in Zones 1 and 3 of the Little Finger. Case Rep Orthop. 2016;2016:6837298. DOI: http://dx.doi.org/10.1155/2016/6837298
7. Toussaint B, Lenoble E, Roche O, Iskandar C, Dossa J, Allieu Y. Subcutaneous avulsion of the flexor digitorum profundus and flexor digitorum superficialis tendons of the ring and little fingers caused by blast injury. Ann Chir Main Memb Super. 1990;9(3):232-5.
8. Kang N, Pratt A, Burr N. Miniplate fixation for avulsion injuries of the flexor digitorum profundus insertion. J Hand Surg Br. 2003;28(4):363-8.
9. Leddy JP. Avulsions of the flexor digitorum profundus. Hand Clin. 1985;1(1):77-83.
10. Azeem MA, Marwan Y, Morshidy AE, Esmaeel A, Zakaria Y. A New Classification Scheme for Closed Avulsion Injuries of the Flexor Digitorum Profundus Tendon. J Hand Surg Asian Pac Vol. 2017;22(1):46-52.
1. Hospital da Força Aérea de Brasília, Brasília,
DF, Brazil.
2. Universidade de Brasília, Brasília, DF,
Brazil.
3. Hospital Naval Marcílio Dias, Ortopedia, Rio de
Janeiro, RJ, Brazil.
4. Instituto Nacional de Traumatologia e
Ortopedia, Rio de Janeiro, RJ, Brazil.
Corresponding author: Henrique Mansur, Área Militar do Aeroporto Internacional de Brasília - Lago Sul - Brasília, DF, Brazil, Zip Code 71607-900. E-mail: henrimansur@globo.com, henrimansur@globo.com
Article received: April 3, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter