

Case Report - Year 2018 - Volume 33 -
Superiorly-based, preauricular tunneled insular flap for reconstruction of auricular defects
Retalho pré-auricular tunelizado insular de base superior para reconstrução de defeitos auriculares
ABSTRACT
The auricular complex is commonly affected by tumors or traumatic events. Several surgical options are available for restoration of ear anatomy. We report the case of a patient who presented with tumor lesions on more than one occasion in the anterior left ear and required surgical intervention to correct the defect generated by excision. As a proposed procedure, we designed and executed a superiorly-based insular flap that was rotated to the scaphoid fossa through a tunnel created in the projection of the triangular fossa; this was performed in a single stage, and the patient was satisfied with the aesthetic and functional results.
Keywords: Ear; Ear neoplasms; Surgical flaps; Reconstructive surgical procedures
RESUMO
O complexo auricular representa sede frequente de lesões, especialmente de origem tumoral ou resultante de eventos traumáticos. Diversas são as opções cirúrgicas para restaurar a integridade anatômica da orelha. Relatamos o caso de um paciente que apresentou lesões tumorais em mais de uma ocasião na face anterior da orelha esquerda e que precisou de intervenção cirúrgica para a correção do defeito gerado pela excisão tumoral. Como procedimento proposto, planejamos e executamos um retalho insular de base superior, que por meio de um túnel criado na projeção da fossa triangular foi rodado para a fossa escafoide, reparando-a em um único tempo cirúrgico, apresentando resultados estético e funcional satisfatórios ao paciente.
Palavras-chave: Orelha; Neoplasias da orelha; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
Restoration of ear anatomical integrity is of fundamental importance after defects are created by resection of cutaneous tumors or resulting from traumatic events1-3, as noted by Sánchez-Sambucety et al.1. These same authors described an option for reconstruction of auricular defects using the transposition of a superiorly-based flap located in the preauricular region, thus maintaining the original characteristics of ear texture and color.
Several surgical techniques can be used for ear reconstruction, including closure by second intention, primary synthesis, partial or total skin grafting, and/or use of local flaps1,3,4.
Auricular repair is complex, especially when the defect reaches the anterior ear because it is more visible. Hence, repair requires techniques that adequately restore structural anatomical integrity. When the tumor is in the scapha, the reconstruction process will depend on the defect size resulting from lesion excision, and whether cartilage and perichondrium are present3.
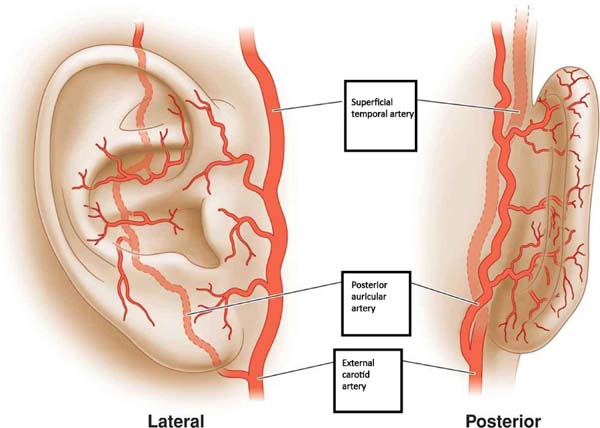
Depending on the affected area, we can employ insular flaps nourished by different arteries. The superficial temporal artery (STA) is of great importance for vascularization of the ear (Figure 1). The STA gives rise to auricular branches that nourish the different parts of the auricular complex3,5. The superior auricular artery branches from the STA, and the superiorly-based flap is especially suitable for repairing non-marginal anterior defects of the scapha, antihelix, and triangular fossa1,5. The remainder of the ear is supplied by the posterior auricular artery5.
In this work, we describe the transposition of a tunneled preauricular insular flap to cover a defect in the scapha using a single-stage surgical procedure with easy technical execution. This procedure can also be used for marginal defects larger than 2.5 cm and can be executed in 2 stages, as described by Di Mascio and Castagnetti4.
CASE REPORT
A 71-year-old patient underwent excision of a cutaneous tumor in the left auricular concha in 2015, followed by cutaneous grafting with good postoperative results. The histopathological report revealed nodular and sclerodermiform carcinoma, with squamous, ulcerated components, and tumor-free surgical margins.
In August 2017, he returned to the Plastic Surgery outpatient clinic complaining of a new lesion in the left ear scapha (Figure 2). We decided on a new surgical approach. The intraoperative frozen section showed that the lesion involved the skin, subcutaneous cellular tissue, and perichondrium, necessitation resection, with a margin of safety extending to lateral and deep limits. To close the defect resulting from the surgical procedure, we chose rotation of a preauricular flap. The lesion was repaired with good aesthetic and functional results.
Surgical technique
The lesion was demarcated with 2% gentian violet, with a safety margin (Figure 3A). Under local anesthesia, the lesion including perichondrium was excised (Figure 3B). The resulting defect was measured on its largest axis. We designed a preauricular flap of dimensions compatible with the defect (Figure 3C).
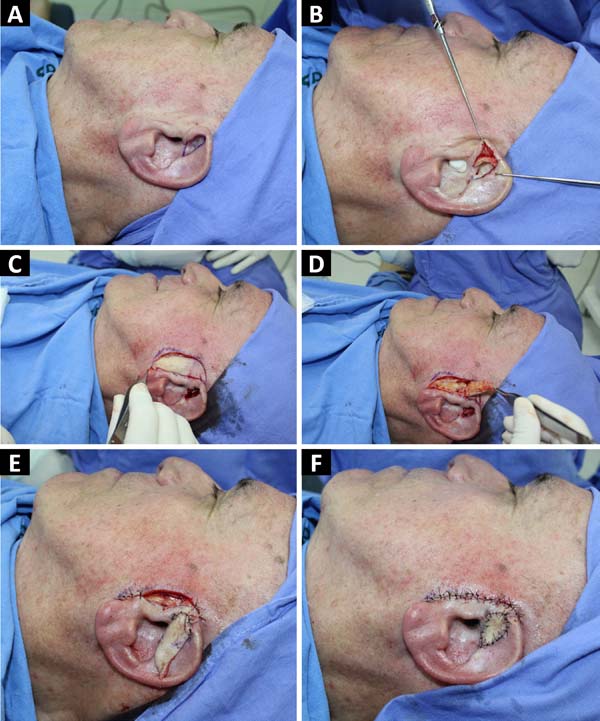
The flap was lifted, and the skin was removed from its base (Figure 3D). An incision was made through the crus of the helix, creating a tunnel for flap passage; the flap was mobilized through the tunnel and adapted to the defect (Figure 3E). The donor and recipient sites were closed using primary synthesis (Figure 3F).
DISCUSSION
The preauricular flap was originally described by Pennisi et al.6 in 1965 for the correction of earlobe defects. With changes in the procedure, the flap was also used for ear defects, but many authors describe this method in 2 stages7.
Lesions resulting from tumors or trauma are common in the auricular complex and require specialized technical expertise for repair. The various options for auricular reconstruction include local flaps, skin grafts, or second intention healing1. It is noteworthy that the use of flaps for auricular reconstruction when excising tumors is the most appropriate technique, since direct closure may cause distortion of the anatomy; grafting in this region is difficult to perform7,8.
When the lesion lies on the scapha, reconstruction will depend on the defect size and whether or not deeper tissues, such as perichondrium and cartilage, are involved8,9. Cartilage exposure requires immediate closure due to the increased risk of infection, necrosis, and chronic chondritis9.
Small defects can be closed with primary synthesis or use of skin grafts. Larger and more complex lesions may require reconstruction with preauricular or postauricular flaps1.
The posterior flap interpolation technique, first described in 1972 by Masson10, is a high-risk procedure, although it is the first choice in concha reconstruction. The tissue tends to present a narrow pedicle and rotating within the ear hinders local circulation.
Several flaps in the mastoid region have been described for ear repair, many of which require 2 surgical stages11,12. In our case, we describe a single-stage flap procedure, with similar auricular skin color and good vascularization; the method can be used to repair defects with or without changes in deeper tissues such as the perichondrium and cartilage. This technique allows a good aesthetic result, in addition to preservation of the auricular pavilion anatomy13.
CONCLUSION
Auricular defects require procedures that restore shape and maintain symmetry. The superiorly-based preauricular flap is easy to perform in experienced hands and provides good skin quality.; it is performed in a single surgical stage, making it ideal for repairing defects in the scapha, antihelix, and triangular fossa.
COLLABORATIONS
|
DAD |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents; special supplement (article submitter). |
|
WS |
Statistical analyses. |
|
PRG |
Analysis and/or interpretation of data. |
|
MFC |
Writing the manuscript or critical review of its contents. |
|
SDB |
Final approval of the manuscript. |
|
FFD |
Completion of surgeries and/or experiments. |
REFERENCES
1. Sánchez-Sambucety P, Alonso-Alonso T, Rodríguez-Prieto MA. Tunnelized preauricular transposition flap for reconstruction of anterior auricular defects. Actas Dermosifiliogr. 2008;99(2):161-2.
2. Armin BB, Ruder RO, Azizadeh B. Partial auricular reconstruction. Semin Plast Surg. 2011;25(4):249-56.
3. Pereira N, Brinca A, Vieira R, Figueiredo A. Tunnelized preauricular transposition flap for reconstruction of auricular defect. J Dermatolog Treat. 2014;25(5):441-3. DOI: 10.3109/09546634.2012.713457
4. Di Mascio D, Castagnetti F. Tubed flap interpolation in reconstruction of helical and ear lobe defects. Dermatol Surg. 2004;30(4 Pt 1):572-8. DOI: 10.1111/j.1524-4725.2004. 30182.x
5. Standring S, ed. Gray's Anatomy: The Anatomical Basis of Medicine and Surgery. 39th ed. London: Churchill-Livingstone; 2005.
6. Pennisi VR, Klabunde EH, Pierce GW. The Preauricular Flap. Plast Reconstr Surg. 1965;35:552-6.
7. Braga AR, Pereira LC, Grave M, Resende JH, Lima DA, De Souza AP, et al. Tunnelised inferiorly based preauricular flap repair of antitragus and concha after basal cell carcinoma excision: case report. J Plast Reconstr Aesthet Surg. 2011;64(3):e73-5. DOI:10.1016/j.bjps.2010.09.005
8. Pereira CCA, Sousa VB, Silva SCMC, Santana ANLL, Carmo MCLC, Macedo PRW. Carcinoma basocelular de localização inusitada na orelha - reconstrução cirúrgica. Surg Cosmet Dermatol. 2016;8(4):362-5. DOI:10.5935/scd1984-8773.201684836
9. Suchin KR, Greenbaum SS. Preauricular tubed pedicle flap repair of a superior antihelical defect. Dermatol Surg. 2004;30(2 Pt 1):239-41.
10. Masson, JK. A simple island flap for reconstruction of concha-helix defects. Br J Plast Surg. 1972;25(4):399-403.
11. Song R, Song Y, Qi K, Jiang H, Pan F. The superior auricular artery and retroauricular arterial islands flaps. Plast Reconstr Surg. 1996;98(4):657-67.
12. Jayarajan R. A versatile flap reconstruction of partial pinna defects - The preauricular flap. JPRAS Open. 2017;13:49-52. DOI: 10.1016/j.jpra.2017.05.007
13. Dessy LA, Figus A, Fioramonti P, Mazzocchi M, Scuderi N. Reconstruction of anterior auricular conchal defect after malignancy excision: revolving-door flap versus full-thickness skin graft. J Plast Reconstr Aesthet Surg. 2010;63(5):746-52. DOI: 10.1016/j.bjps .2009.01.073
1. Hospital Federal de Ipanema, Rio de Janeiro,
RJ, Brazil.
Corresponding author: Délcio Aparecido Durso, Rua Visconde de Pirajá, 135, apto 603 - Ipanema - Rio de Janeiro, RJ, Brazil, Zip Code 22410-001. E-mail: medurso06@yahoo.com.br
Article received: January 3, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter