

Ideas and Innovation - Year 2018 - Volume 33 -
High-definition abdominal liposuction with silicone tubing
Lipoaspiração abdominal de alta definição e tubos de silicone
ABSTRACT
Introduction: Recently, some authors have described high
definition liposuction in the abdominal region, achieved by
the vigorous marking of the grooves of the linea alba, linea
semilunaris, and transverse tendinous intersections within
the rectus abdominis muscle. The aim is to present a pilot
study of high-definition abdominal liposuction technique using
conventional material and silicone tubing in the dressings
.
Methods: Twenty cases were submitted to conventional
liposuction, followed by superficial liposuction under the
linea alba, linea semilunaris, and tendinous intersections,
until a groove was formed at these sites. Flexible silicone
tubing was externally fixed with Micropore tape in the linea
alba, bilateral linea semilunaris, and tendinous intersections,
and removed after 5 days.
Results: A mean increase of 20
minutes was required to perform these steps. The marks of
the silicone tubing were evident at the first follow-up, and
less prominent at the second follow-up. No color change,
ischemia, or significant pain was observed using this
technique. After 3 months, there were no cases of dermatitis,
cutis marmorata, seroma, infection, contour irregularity or
need for additional procedures.
Conclusion: High-definition
abdominal liposuction was performed using conventional
materials and externally fixed temporary silicone tubing.
Keywords: Lipectomy; Lipectomy/trends; Lipectomy/use; Dressings; Compression dressings
RESUMO
Introdução: Recentemente, alguns autores têm descrito a lipoaspiração de alta definição,
na qual, na região abdominal, é alcançada pela marcação vigorosa dos sulcos
das linhas alba, semilunar e interseções tendíneas transversais do músculo
reto abdominal. O objetivo é apresentar estudo piloto de técnica de
lipoaspiração de alta definição abdominal utilizando material convencional e
tubos de silicone nos curativos.
Métodos: Foram descritos 20 casos, submetidos à lipoaspiração convencional e em
seguida lipoaspiração superficial sob as linhas alba, semilunar e
interseções tendíneas, até que se obtivesse a formação de um sulco nestes
locais. Utilizamos tubos de silicone maleáveis nas linhas alba, semilunar
bilateral e interseções tendíneas, fixados externamente com micropore, os
quais foram removidos após 5 dias.
Resultados: Houve um acréscimo médio de 20 minutos para realização destas etapas. As
marcas dos tubos de silicone apresentaram-se muito evidentes no primeiro
retorno, estando mais discretas no segundo retorno. Não foram observadas
alterações de coloração, isquemia ou dor maior pela técnica empregada. Após
3 meses, não houve nenhum caso de dermatite, cútis marmorata, seroma,
infecção, irregularidade de contorno ou necessidade de procedimentos
adicionais.
Conclusão: Foi realizada lipoaspiração de alta definição abdominal, com material
convencional e uso de tubos de silicone temporários fixados
externamente.
Palavras-chave: Lipectomia; Lipectomia/tendências; Lipectomia/utilização; Bandagens; Bandagens compressivas
INTRODUCTION
In 1993, Mentz et al.1 were the first to perform superficial liposuction to define the abdominal musculature, and suggested the use of superficial liposuction in the linea alba, linea semilunaris, and transverse tendinous intersections, without use of foams or other material to better define the abdominal lines.
In 2003, Hoyos & Millard2 introduced the concept of high-definition liposculpture, refining the original concept1 for a 3-dimensional approach, in which not only the abdomen, but also the back, arms, and legs were treated using third-generation ultrasonic liposuction (Vaser).
Reston® foam has been used in liposuction3-5. Despite the benefits, the application only lasts approximately 30 minutes, in addition to being associated with other problems4,6,7 such as allergic dermatitis, blister formation, and postoperative hyperpigmentation.
This pilot study aimed to present a superficial liposuction technique using conventional materials, followed by dressings incorporating soft silicone tubing; the technique is easy for plastic surgeons to learn, and is economically accessible, with satisfactory aesthetic results and low incidence of complications.
OBJECTIVE
To describe a superficial abdominal liposuction technique for the linea alba, linea semilunaris, and transverse tendinous intersections within the rectus abdominis muscle using conventional liposuction material, followed by dressings incorporating soft silicone tubing.
METHODS
This prospective pilot study included 20 patients (19 women and 1 man), who underwent abdominal liposuction under general anesthesia by the same surgeon.
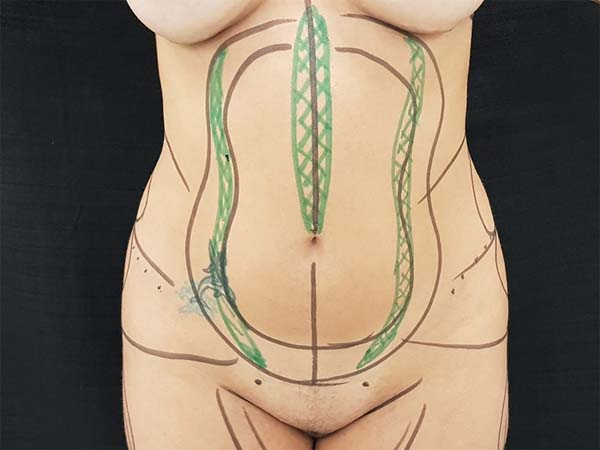
All patients were marked on the abdominal region and other areas planned for liposuction, using a hydrographic pen on the day of surgery. The linea alba, linea semilunaris, and tendinous intersections within the rectus abdominis muscle were identified by abdominal contraction and marked in green (Figure 1).
Two 7-mm incisions were made in the pubic region, inside the swimwear line or in previous scars (Figure 1).
Super-saturation of the abdominal region was performed with saline solution combined with epinephrine at a concentration of 1:500,000 and lidocaine at a concentration of 0.05%.
Liposuction was performed below (deep liposuction) and above (superficial liposuction) Scarpa’s fascia, using 60-mL syringes in the usual manner, with cannulas 4 mm in diameter and 30 and 35 cm in length.
Liposuction was then performed under the linea alba and linea semilunaris, above Scarpa’s fascia and close to the deep dermis (Figure 2), with the same 4-mm cannulas, but with the holes facing the dermis and using the contralateral hand for gripping and vigorous extra fat removal, until the formation of a groove was obtained in these locations, confirmed by the surgeon with a pinch test.
In the male patient, three 3-mm incisions were also made in the supraumbilical linea alba for superficial subdermal liposuction below the tendinous intersections of the rectus abdominis muscle, using 3-mm diameter cannulas, until groove formation was observed.
Next, 20% tincture of benzoin and 7-mm-diameter flexible empty silicone tubing were placed at the contour of the linea semilunaris (Figure 3) and the rectilinear supraumbilical linea alba; the tubing was fixed vertically with Micropore tape over the full length of the treated area (Figure 4).
The hollow silicone tubing was kept occluded for 5 to 6 days and then removed, but shapewear was maintained for 30 days.
All patients underwent manual lymphatic drainage for a period of 30 days, starting at a variable period of 3 to 6 days.
Follow up was performed with clinical and photographic examination at 4-6 days, 3-4 weeks, and 3 months after surgery.
RESULTS
The additional superficial liposuction of the linea alba and linea semilunaris added an average time of 15 minutes to the procedure. Use of dressings with silicone tubing added 5 minutes.
The marks of the silicone tubing were very evident at the first follow-up, and were less prominent at the second follow-up. No color change, ischemia, or significant pain was observed with this technique.
After 3 months, the results were considered good (Figures 5 to 8), with no cases of cutis marmorata, dermatitis, seroma, infection, contour irregularity, or need for additional procedures.
DISCUSSION
In 2012, a randomized, blinded, controlled clinical trial7 compared conventional liposuction with Vaser liposuction, and concluded that there is more retraction and less blood loss with Vaser, but no change in outcome in terms of pain, edema, or adverse effects. This work was limited in its validity8 due to sampling methodology, financial conflicts, and commercial bias. The study also described the occurrence of seromas, burns, and prolonged edema, in addition to a longer learning curve and greater investment for equipment9,10.
The technique advocated in this study differs from those previously described by using silicone tubing, not previously described for use in liposuction dressings. The tubing is hollow and thin (7-mm diameter), and used in pre-planned locations, especially at the linea semilunaris, where the wavy shape helps the skin to adhere directly in the muscular plane; this enhances the appearance of the abdominal musculature, with a more natural final result, besides avoiding possible complications with foams, as previously described3-6.
This technique required little additional surgical time, especially when compared to use of Reston® and ultrasonic or laser liposuction, to achieve greater abdominal refinement.
This method can be added to any conventional liposuction technique, whether performed with syringe, aspirator, or vibro-liposuction, and can be used by any plastic surgeon familiar with liposuction who wants to achieve greater anatomical definition of the abdomen.
Both the medical team and patients reported greater satisfaction with this technique, compared to that without a high-definition approach.
The cases in this pilot study remain in follow-up for long-term evaluation with statistical analysis.
CONCLUSION
This study described the technique of superficial abdominal liposuction at the linea alba, linea semilunaris, and transverse tendinous intersections within the rectus abdominis muscle, using conventional liposuction material, followed by dressing that incorporated silicone tubing and shapewear.
COLLABORATIONS
|
RSG |
Conception and design study; conceptualization; data curation; realization of operations and/or trials; writing - original draft preparation. |
|
CMM |
Conception and design study; investigation |
|
NBR |
Conceptualization. |
|
EBG |
Project administration; supervision. |
|
HFCG |
Project administration; supervision. |
|
LMF |
Project administration; supervision. |
REFERENCES
1. Mentz HA 3rd, Gilliland MD, Patronella CK. Abdominal etching: differential liposuction to detail abdominal musculature. Aesthetic Plast Surg. 1993;17(4):287-90.
2. Hoyos AE, Millard JA. VASER-assisted high-definition liposculpture. Aesth Surg J. 2007;27(6):594-604.
3. Brandy DA. Reston Foam for the Reduction of Ecchymoses Post-Liposuction. Am J Cosm Surg. 1990;7(2):87-91.
4. Fischer G. Liposculpture 4. Fundamentals of good liposculpture technique. J Dermatol Surg Oncol. 1992;18(3):216-9.
5. Schlesinger SL, Kaczynski AJ. Use of Reston foam in liposuction. Aesthetic Plast Surg. 1993;17(1):49-51.
6. Klein J. Miscellaneous complications. In: Klein J, ed. Tumescent technique. St. Louis: Mosby; 2000. p. 46-7.
7. Nagy MW, Vanek PF Jr. A multicenter, prospective, randomized, single-blind, controlled clinical trial comparing VASER-assisted Lipoplasty and suction-assisted Lipoplasty. Plast Reconstr Surg. 2012;129(4):681e-9e.
8. Swanson E. Improved skin contraction after VASER-assisted lipoplasty: is it a change we can believe in? Plast Reconstr Surg. 2012;130(5):754e-6e.
9. Jewell ML, Fodor PB, de Souza Pinto EB, Al Shammari MA. Clinical application of VASER--assisted lipoplasty: a pilot clinical study. Aesthet Surg J. 2002;22(2):131-46.
10. de Souza Pinto EB, Abdala PC, Maciel CM, dos Santos Fde P, de Souza RP. Liposuction and VASER. Clin Plast Surg. 2006;33(1):107-15.
1. Escola Paulista de Medicina, Universidade
Federal de São Paulo, São Paulo, SP, Brazil.
2. Universidade Federal de Santa Catarina,
Florianópolis, SC, Brazil.
3. Hospital Universitário, Florianópolis, SC,
Brazil.
Corresponding author: Rogerio Schützler Gomes, Av. Trompowsky, nº 291 sala 303, Torre 1 - Centro - Florianópolis, SC, Brazil, Zip Code 88015-300. E-mail: plasticarogerio@gmail.com
Article received: October 23, 2018.
Article accepted: November 11, 2018.
Conflicts of interest: none.

















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter