

Original Article - Year 2018 - Volume 33 -
Effect of medial hemisoleus muscle flap on wound healing in the medial and distal thirds of the lower leg
Retalho muscular de hemisóleo medial na reparação de feridas dos terços médio e distal da perna
ABSTRACT
Introduction: The use of many flaps has been described to
repair substance loss in the medial and distal thirds of the
lower leg. The main advantage of the muscle medial hemisoleus
flap is preserving one half of the innervated medial soleus
muscle in situ and keeping the foot's plantar flexion power.
Moreover, the flap has a longer arc of rotation. As recently
described, new vascular concepts and techniques have
increased flap viability. This study aimed to examine the use
and advantages of the medial hemisoleus flap with emphasis
on an indication and complication analysis.
Methods: Over a
10-year period, nine medial hemisoleus flaps were executed
to repair traumatic wounds with tibial exposure in eight
patients. We describe the indications and surgical techniques
in detail.
Results: Complete wound healing was achieved in
all patients. There was a low donor-site complications rate.
One patient suffered from partial necrosis of the extremity
flap. The mean operative time was 2 h.
Conclusions: The
medial hemisoleus flap is useful for repairing substance
loss and provides coverage with intermediary thickened
tissue, high vascularity, minimal donor-site morbidity, foot
plantar flexion power preservation, faster rehabilitation,
accessible surgical techniques, and a shorter operative time.
Keywords: Reconstructive surgical procedures; Lower extremity; Muscle, skeletal; Surgical flaps
RESUMO
Introdução: Muitos retalhos são descritos para reparar as perdas de substância nos terços
médio e distal da perna. A principal vantagem do retalho de músculo
hemisóleo medial é a preservação da inervação da metade do músculo sóleo no
sítio doador, mantendo a força de flexão plantar. Além disso, este retalho
tem um arco de rotação maior quando comparado ao retalho de músculo sóleo
convencional. Novos conceitos vasculares e técnicos, descritos recentemente,
aumentaram a viabilidade deste retalho. O objetivo deste estudo é relatar a
utilização do retalho de hemisóleo medial enfatizando as vantagens,
reafirmando as indicações e analisando as complicações.
Métodos: Em dez anos, um total de nove retalhos de hemisóleo medial foram
confeccionados para a reparação de feridas traumáticas com exposição da
tíbia em oito pacientes. Os critérios de indicação e técnica cirúrgica são
descritos detalhadamente.
Resultados: A cicatrização completa da perda de substância foi alcançada em todos os
pacientes. Observou-se baixo índice de complicações no leito doador e em um
paciente houve necrose parcial da extremidade do retalho. O tempo médio de
realização do procedimento foi de duas horas.
Conclusões: Retalhos de hemisóleo medial são muito úteis na reparação destas perdas de
substância e permitem a cobertura com tecido de espessura intermediária,
rica vascularização, baixo índice de morbidade na área doadora, preservação
da função motora plantar, reabilitação mais rápida no pós-operatório,
técnica cirúrgica acessível e menor tempo operatório.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Extremidade inferior; Músculo esquelético; Retalhos cirúrgicos
INTRODUCTION
The use of cutaneous, fasciocutaneous, muscle, free tissue transfer, and various other flaps have been described to repair the loss of substance in the medium and distal thirds of the leg; several authors consider that the treatment of these defects as a unique challenge1-5. Exposure of the bones, tendons, and osteosynthesis materials associated with the lack of availability of local soft tissue in this area of the body are contributing factors that hinder planning and therapy in such cases2.
Free microsurgical transfer flaps are often the first therapeutic option to promote adequate coverage; their use requires a specific professional multidisciplinary team, specialized infrastructure, and higher cost and must be reserved for traumas that compromise the posterior muscle compartment and vascularization of the leg1-6. However, cutaneous, fasciocutaneous, and even fasciosubcutaneous flaps are technically more accessible, have higher rotational arcs, lower donor-site morbidity rates, and simpler postoperative courses,3,5,7-9 but they must be avoided in situations that require the provision of an increased local blood supply (e.g., fractures with exposed bone)1.
When local muscle flaps are carefully indicated and implemented, they can provide rich vasculature coverage and intermediate thickness6. The main muscles used for medial- and distal-third reconstruction include the flexor digitorum longus, tibialis posterior, flexor hallucis longus, peroneus brevis, peroneus longus, extensor digitorum longus, extensor hallucis longus, reverse tibialis anterior, and soleus4,10,11. Limitations and probable contraindications include patients with severe muscle and vascular-associated traumas and the presence of peripheral vascular disease1,6.
Soleus flaps were first described by Magee et al. in 198012. In 1985, Tobin13 systematized and correlated the morphology of the soleus muscle with the vascular pattern of its pedicles and intramuscular and extramuscular branches, allowing the creation of a large pediculated flap made with the longitudinal half of the hemisoleus flap. This flap can be constructed using the medial or lateral belly of the soleus muscle using direct or reverse blood flow.
Therefore, four flaps are possible: medial hemisoleus pediculated proximally, medial hemisoleus pediculated distally (or reverse), lateral hemisoleus pediculated proximally, and lateral hemisoleus pediculated distally (or reverse)13. The main advantage of these flaps is the preservation of the innervation of the half of the soleus muscle that remains in the donor site, which maintains the plantar flexion force. In addition, the hemisoleus flap has a larger rotational arc than the conventional soleus flap13-15.
In 2005 and 2008, Pu described surgical refinement techniques establishing parameters and increasing reliability for medial hemisoleus flaps6,16. More recently, the association of the technique with angiosome principles (three-dimensional tissue blocks whose irrigation is provided by a branch of a specific deep stem artery)17 described by Taylor & Palmer (1987)17 the design of the flap and the need for careful dissection with the benefit of obtaining a thinner flap with lower donor-site morbidity rates, especially for reverse flow flaps1,9,18.
The medial hemisoleus flap is the most frequently used because of its proximity to the defects that occur more frequently in the three-quarter proximal tibia and because it presents a greater rotation arc than the lateral hemisoleus flap1,6,13.
OBJECTIVE
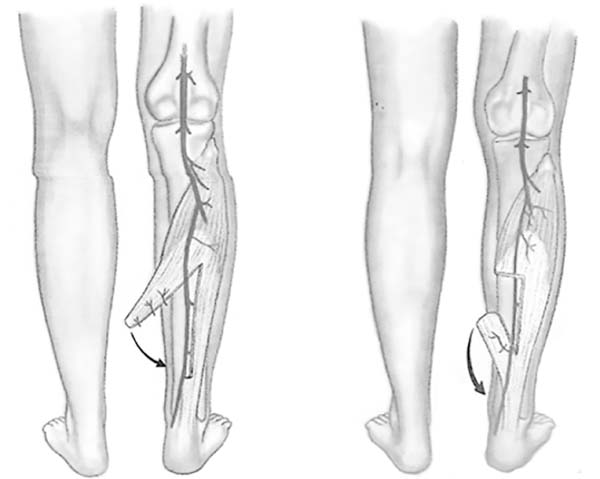
This study aimed to report the use of the medial hemisoleus flap proximal (direct flow) or distal (reverse flow) (Figure 1), emphasize its advantages, confirm its indications, and analyze the complications of this procedure as an alternative in the surgical arsenal to repair substance losses of the medial and distal thirds of the leg.
METHODS
Over a 10-year period, a total of nine medial hemisoleus flaps were created in eight patients (six men, two woman) to repair substance losses of traumatic etiology with tibial exposure. The surgeries were performed at the Ibiapaba Cebams Hospital of Barbacena - MG. The Medical Ethics Committee of Ibiapaba Cebams Hospital analyzed and approved this study (protocol number 001/2018).
The inclusion criteria were as follows:
Presence of a wound with exposed bone or osteosynthesis material in
the medial or distal third of the leg comprising an area < 50
cm².
Stabilization of the fracture when present. Lack of peripheral vascular disease or other conditions that could
compromise the vascular pattern of the soleus muscle, such as
diabetes, smoking, paraplegia, or previous history of vascular
obstruction of the lower limb.
Lack of trauma evidence of compromise of the medial muscle belly of
the soleus.
Treatment of established infectious condition with debridement,
dressings, and systemic antibiotic therapy before the procedure.
The soleus muscle has a characteristic bipeniform morphological pattern (98.8% of cases) in which the medial and lateral belly present independent neurovascular supplies and are longitudinally separated at the medial line. The medial belly originates in the proximal tibia and inserts into the dorsomedial aspect of the calcaneal tendon, while the lateral belly originates in the proximal fibula and inserts into the dorsolateral side of the calcaneal tendon. In the distal half, the medial and lateral bellies of the muscle are separated longitudinally by an intramuscular septum; in the proximal half, these same bellies are fused13.
The vascularization is type II Mathes & Nahai19. There are two proximal dominant pedicles: the tibialis posterior branch that nourishes the medial belly through segmental branches and the fibular branch that nourishes the lateral belly through proximally segmental branches and distally axial segmental branches1,6. A distal perforating branch of the tibialis posterior artery near the medial malleolus also nourishes the distal portion of the medial belly and forms the base of the medial reverse hemisoleus flap6.
The medial and lateral bellies of the soleus muscle are independently innervated.
The medial branch of the medial (superficial) popliteal nerve and the medial branch of the tibialis posterior nerve (motor) innervate the medial belly of the soleus, whereas the lateral belly of the soleus is innervated by the lateral branches of the medial popliteal and posterior tibial nerves13.
Surgical technique
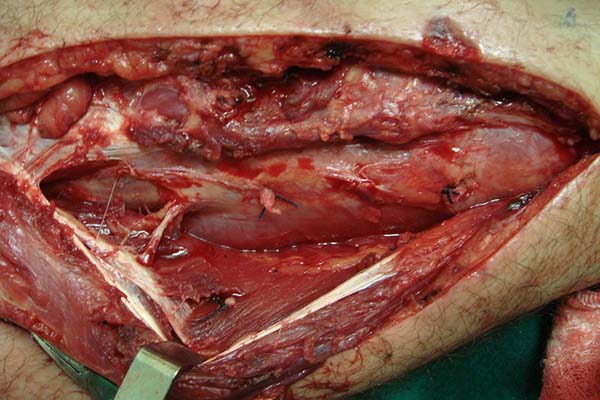
A longitudinal cutaneous incision is made on the medial side of the leg parallel to the medial border of the tibia. The existence of external orthopedic fixators should be considered an inherent part of this surgical procedure, since they are present in most cases (Figure 2). The skin is carefully retracted and allows opening and exposure of the subcutaneous and fascial planes. Whenever possible, superficial nerves (sural, saphenous) and vessels (saphenous vein) should be preserved1. The gastrocnemius muscle is separated from the medial portion of the soleus muscle by blunt dissection20, the deep fascia is opened, and the soleus border is detached from the tibia with the scalpel. The major and secondary vascular pedicles are identified. Careful dissection of the pedicles enables a larger arc of rotation and, consequently, greater flap reach.
In the preparation of the proximal pedicle medial hemisoleus flap, the main pedicle (proximal) is maintained and the secondary pedicles are sectioned (Figure 3). The medial hemisoleus is then disinserted from the calcaneal tendon using a scalpel or other acute cutting instrument featuring lower trauma such as those described by Pu6, and the separation of the medial and lateral bellies of the muscles is guided by the intramuscular septum (Figure 4).
In the preparation of the reverse medial hemisoleus flap, the main pedicle is maintained (distal perforating branch of the posterior tibial artery) and the proximal main pedicle and other secondary pedicles are sectioned. According to the angiosome principle1,8, the flap will be sectioned 2–3 cm proximal to the connected secondary pedicle since the next pedicle must be the distal perforating branch of the posterior distal artery. Separation of the medial and lateral muscle bellies is also performed under intramuscular septum guidance (Figure 5).
The flap is then rotated under a previously made fasciocutaneous tunnel (Figures 6 and 7) and the area of the defect is fixed with a 4.0 absorbable suture. The fasciocutaneous tunnel cannot overcompress the flap. In this case, a transverse fasciotomy can be performed in the tunnel and even the communication of the access area to the flap with the surgical wound.
Once fixed in place, the flap is covered with a thin partial-thickness skin graft (Figure 8). The donor area of the flap does not require a cutaneous graft and receives a primary suture of the deep fascia and the subcutaneous tissue with polyglecaprone 4.0 strands. The skin suture is made using 4.0 nylon thread (Figure 9). Suction drains are used and the non-compressive dressing generally dispenses with immobilization by a gypsum chute due to the presence of the external fasteners.
In the postoperative period, it is important that the patient remains in bed with the operated limb elevated for 4–5 days to reduce edema and venous congestion.
RESULTS
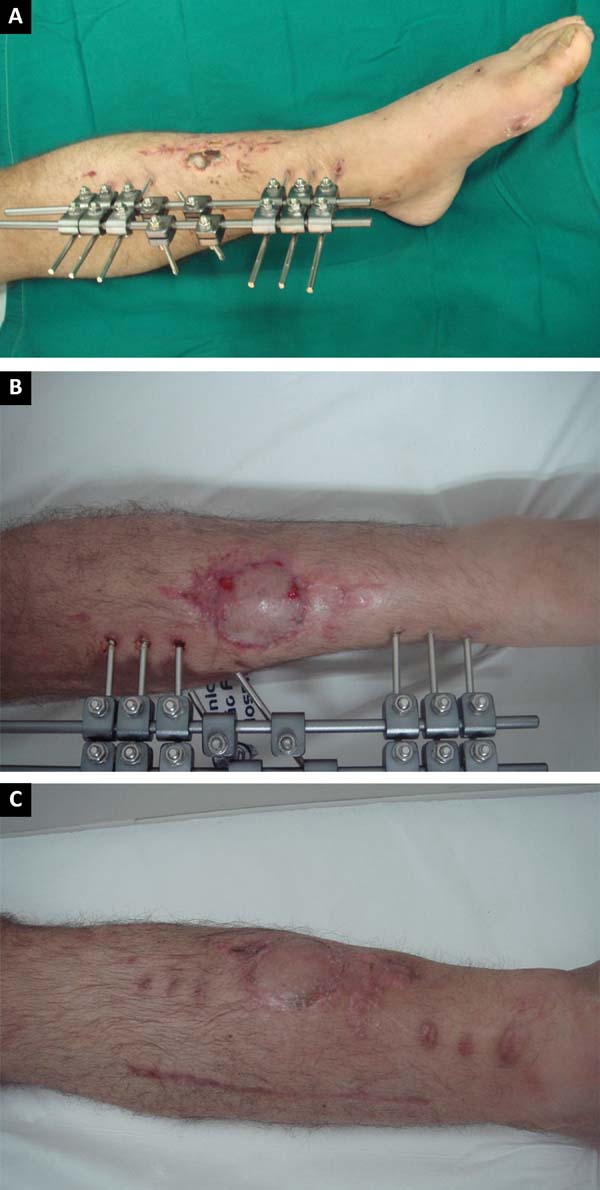
In this series of eight patients (six men [75%] and two women [25%]), nine hemisoleus flaps were made (Table 1). One of the patients (Table 1: APO) had exposed fractures of the bilateral tibiae and underwent bilateral repair with medial hemisoleus flaps at different times. In three patients, a medial reverse hemisoleus flap was used (Figures 10A, B, and C) to repair substance losses in the lower distal third of the leg caused by burns and exposed tibial fractures. The remaining six cases were treated with proximally pediculated hemisoleus flaps (Figures 11, 12, and 13) for repair of wounds with mid-tibial bone exposure caused by automobile accidents and burns. The mean age was 40.5 years (range, 20–68 years). Seven patients (77.7%) underwent surgery after fracture stabilization with external fixators and had palpable and normal pulses.
| Patient | Age(years) | Sex | Injury location | Injury cause | Pretreatment | Medialhemisoleusflap | Flap complication or skin grafting | Fracturecomplications | Follow-uptime |
|---|---|---|---|---|---|---|---|---|---|
| PCO | 20 | Male | Open fracture, medial 1/3 of the left tibia | Automobileaccident | Fasciosubcutaneous reverse calf flap | Proximalpedicle | - | - | 30 months |
| LMF | 27 | Male | Open fracture, medial 1/3 of the left tibia | Automobileaccident | "Cross-leg" and fracture fixation | Proximalpedicle | - | Pseudo-arthrosis | 27 months |
| APO | 30 | Male | Open fracture, medial 1/3 of the right tibia | Automobileaccident | Fracture fixation, thoracotomy, and laparotomy | Proximalpedicle | Donor-site hematoma | - | 22 months |
| APO | 30 | Male | Open fracture, medial 1/3 of the left tibia | Automobileaccident | Hemisoleus medial right flap | Proximalpedicle | - | - | 22 months |
| GMS | 41 | Male | Medial malleolus right exposure | Overheated metal burn | Debridement and dressings | Reverse | - | - | 4 months |
| OMS | 54 | Male | Open fracture, distal 1/3 of the left tibia | Home accident (fall) | Fracture fixation | Reverse | Partial flap loss | - | 18 months |
| MEF | 68 | Female | Open fracture, distal 1/3 of the right tibia | Home accident (fall) | Fracture fixation | Reverse | Partial skin graft loss | Chronicosteomyelitis | 12 months |
| JASB | 32 | Male | Open fracture, medial 1/3 of the left tibia | Automobileaccident | Fracture fixation | Proximalpedicle | Partial skin graft loss | - | 6 months |
| MLRD | 63 | Female | Open fracture, medial 1/3 of the right tibia | Electrical burn | Debridement and dressings | Proximalpedicle | Partial skin graft loss | - | 5 months |
Two patients (22.2%) previously underwent rotation of other flaps with unsatisfactory results. The first one developed complete necrosis of the fasciosubcutaneous reverse flap of the calf caused by the large wound extension and prolonged bone exposure (chronic osteomyelitis). The other patient did not tolerate the immobilization in the postoperative period of a “cross leg.”
One of the patients (11.1%) presented bleeding in the donor area of the flap on the 10th postoperative day caused by disruption of the sectioned distal pedicle that was treated with immediate drainage and there was no compromise of the flap vascularization.
Partial necrosis of the medial reverse hemisoleus flap occurred in one patient (11.1%); the probable causes are related to the presence of local infection, severe venous congestion in the postoperative period, compression by the fasciocutaneous tunnel, and advanced patient age. In this case, the sequential therapy was conservative (debridement, treatment of osteomyelitis and assisted dressings under vacuum) and wound healing was achieved.
Partial-thickness skin grafts were performed at the same surgical time in eight of the nine cases; in three patients (33.3%), there were insignificant losses of skin graft integration without the need for additional surgical procedures (Figure 11B).
The mean surgical time was 2 hours, while the hospital stay after the flap production was 4–28 days (mean, 17.7 days). All patients achieved complete wound healing. In the postoperative follow-up period, three patients required orthopedic surgical treatment with grafts and bone expansion to correct pseudoarthrosis. The minimum postoperative follow-up was 4 months and the mean follow-up time was 16.2 months.
DISCUSSION
Therapeutic options for repairing complex wounds of the medial and distal thirds of the leg cannot yet be considered consensual. Several flaps have been described; however, the muscular flaps, particularly the hemisoleus flap, require intermediate procedures between the fasciocutaneous flaps and transfer free flaps.
All patients in the series underwent medial hemisoleus flap transfer based on the favorable location of the wound, and the main feature of this flap is maintaining plantar flexion at the ankle joint. The soleus muscle is responsible, together with the gastrocnemius muscle, for stabilizing the leg over the foot, that is, for maintaining posture and preventing the body from falling forward when in the upright position21. Preservation of the lateral belly of the soleus at the donor area reduces the use of compensatory mechanisms that arise when the soleus is fully rotated: short step, reduced ability to tilt the body forward, and precocious contralateral calcaneus wound13.
Associated with this precious advantage, hemisoleus flaps are interesting because they promote low morbidity in the donor bed with the need for skin grafts in these areas. This was confirmed in the series of patients in this study, in which all donor areas were closed primarily without epidermolysis or necrosis. Only one patient had late complications (bleeding) in the donor area and no impairment of the final healing result in the flap donor and recipient areas.
The concept that covering wounds with a rich vascular supply is important in cases of bone exposure favoring fracture consolidation is widely advocated by adherents of muscle flaps1,6,11,13,19. However, controversy persists regarding the true beneficial potential of the rich vascularization of muscle flaps in primary fracture consolidation3, which seems to have been suggested in this series in which three patients (37.5%) still required orthopedic surgical complements for fracture healing (Table 1). On the other hand, this rich vascularization is certainly responsible for the high integration rates of the skin graft on the muscle, a fact not observed in the use of fascial and fasciocutaneous flaps2,7,19, where the capacity to supply adequate coverage thickness and well vascularized continues to be questioned.
The mean surgical time did not exceed the 2 hours, a fact that has a direct positive impact on technical execution, treatment cost, and postoperative morbidity rate.
The importance of microsurgical transfer free flaps is based on the potential of promoting coverage in a single procedure with tissue considered healthy and not associated with trauma. It combines the development of vascular techniques, surgical microscopes, delicate instruments, microsurgical threads, and differentiated surgical strategies that, in most cases, are the major limiting factors of this therapy9,14,16. In this context, the hemisoleus flap can be very useful in the treatment of substance losses of the medial and lower leg when the compromised area is <50 cm². Conventional soleus muscle flaps may cover a mean area of 26 cm² according to Hughes et al. 4, who performed numerical studies on cadavers comparing the arcs of rotation of different muscle flaps of the leg.
Pu and Dumanian stated that wounds up to 50 cm² can be safely repaired with medial hemisoleus flaps, reporting a significant gain in extent for this flap1,6.
Detailed knowledge of the morphological and neurovascular anatomy of the soleus muscle is obviously the initial condition for performing this procedure. For this purpose, previous dissections in cadavers can be very enlightening and illustrative22. The technical refinements described by Pu involve the delicacy of the surgical approach to the muscle, dissection of the main pedicles with the purpose of lengthening the rotation arc, use of sharp blades for the medial soleus tendon transversal section that is intimately connected to the gastrocnemius tendon, and suture of the medial tendon of the hemisoleus in the lateral segment of the muscle to minimize functional losses16,20.
By combining this knowledge with the described angiosome principles, especially for reverse flaps, high success rates can be achieved22. The main complications described (postoperative bleeding, partial graft losses, and failure of previously used flaps) were observed at the beginning of the series; therefore, they may be related to technique and indications. The use of the more accurate technique and more rigorous indication criteria, which occurred gradually throughout the series, reduced the complication rates of this flap. Therefore, the learning curve is a considerable factor in the improvement of this surgical technique.
Some complementary steps are also being gradually added in the treatment of these wounds, such as: assisted vacuum closure in the preoperative preparation to reduce injury extent, preoperative angiography in the evaluation of the flap’s vascular potential, postoperative Doppler use, design of the most viable flap design, and description of patch associations for extensive wound closure1,6,13,23. The insertion of these concepts into the therapeutic plan may reduce the postoperative complication rates and increase the technical reliability of this procedure.
CONCLUSIONS
The use of medial hemisoleus proximal (direct flow) or distal (reverse flow) flaps is very useful for repairing substance losses from the medial and distal thirds of the leg and allow wound coverage with intermediate thickness tissues, rich local vascularization, a low donor-area morbidity index, preservation of the plantar motor function, faster postoperative rehabilitation, accessible surgical technique, and shorter operative time.
These flaps may be considered a secondary alternative to transfer free flaps in the reconstruction of these defects or even the first treatment option in cases in which a minor injury or the presence of comorbidities does not justify the complexity of using a transfer free flap.
The association with the angiosome concept and the technical refinements described recently increased hemisoleus flap manufacture safety, reaffirming that the establishment and observation of the indication criteria in preoperative planning is essential to guarantee greater therapeutic success and reduce the postoperative complication rate.
COLLABORATIONS
|
EJC |
Analysis and/or data interpretation, conception and design study, conceptualization, final manuscript approval, realization of operations and/or trials, supervision, writing - review & editing. |
|
MLPN |
Analysis and/or data interpretation, data curation, final manuscript approval, realization of operations and/or trials, software, writing - original draft preparation. |
|
LACF |
Analysis and/or data interpretation, data curation, final manuscript approval, writing - original draft preparation. |
|
DMCJ |
Analysis and/or data interpretation, data curation, final manuscript approval, realization of operations and/or trials, writing - original draft preparation. |
REFERENCES
1. Schierle CF, Rawlani V, Galiano RD, Kim JY, Dumanian GA. Improving outcomes of the distally based hemisoleus flap: principles of angiosomes in flap design. Plast Reconstr Surg. 2009;123(6):1748-54. DOI: 10.1097/PRS.0b013e3181a65a74.
2. Verhelle N, Vranckx J, Van den Hof B, Heymans O. Bone exposure in the leg: is a free muscle flap mandatory? Plast Reconstr Surg. 2005;116(1):170-7.
3. Braga-Silva J, Martins PDE, Roman JA, Gehlen D. Utilização do retalho adipofascial reverso nas perdas de substância cutânea do terço distal da perna e pé. Rev Soc Bras Cir Plást. 2005;20(3):182-6.
4. Hughes LA, Mahoney JL. Anatomic basis of local muscle flaps in the distal third of the leg. Plast Reconstr Surg. 1993;92(6):1144-54.
5. Belém LFMM, Lima JCSA, Ferreira FPMF, Ferreira EM, Penna FV, Alves MB. Retalho sural de fluxo reverso em ilha. Rev Soc Bras Cir Plást. 2007;22(4):195-201.
6. Pu LLQ. Further experience with the medial hemisoleus muscle flap for soft-tissue coverage of a tibial wound in the distal third of the leg. Plast Reconstr Surg. 2008;121(6):2024-8. DOI 10.1097/PRS.0b013e318171240c
7. Canton EJ, Barbosa LS, Ferreira AB, Conde CMY, Respeita EMZ, Gonçalves LB, et al. Reconstrução do terço inferior da perna com retalho fasciocutâneo de pedículo distal. HU Rev. 2002;28:364-6.
8. Martins GB, Moreira AL, Viana FO. Reconstrução de lesões de partes moles do calcanhar com o uso de retalhos fasciocutâneos. Rev Bras Cir Plást. 2009;24(1):104-9.
9. Batista J. Retalho supramaleolar de fluxo reverso: aplicações clínicas. Rev Bras Cir Plást. 2011;26(1):140-6.
10. Cortez M, Borges LG, Lima SCA. Um novo retalho muscular para cobertura do terço inferior da perna e do pé. Rev Bras Ortop. 1993;28(9):687-93.
11. Bacelar TH. Utilização do músculo sóleo para perdas musculocutâneas de terço médio da perna. Rev Bras Cir Plást. 2011;26(2):211-20.
12. Magee WP Jr, Gilbert DA, McInnis WD. Extended muscle and musculocutaneous flaps. Clin Plast Surg. 1980;7(1):57-70.
13. Tobin GR. Hemisoleus and reversed hemisoleus flaps. Plast Reconstr Surg. 1985;76(1):87-96.
14. Souza Filho MVP, Teixeira JCEO, Castro OC. Retalho hemisolear reverso na reconstrução de defeito do terço distal da perna. Rev Bras Cir Plást. 2011;26(4):710-3.
15. Ahmad I, Akhtar S, Rashidi E, Khurram MF. Hemisoleus muscle flap in the reconstruction of exposed bones in the lower limb. J Wound Care. 2013;22(11):635,638-40, 642. DOI: 10.12968/jowc.2013.22.11.635
16. Pu LLQ. The medial hemisoleus muscle flap for soft-tissue coverage of an open wound in the distal leg: P74. Plast Reconstr Surg. 2005;116(Suppl 3):215-6.
17. Costa AC. Retalho ântero-lateral da coxa - estudo anatômico em brasileiros [Tese de doutorado]. São Paulo: Faculdade de Ciências Médicas da Santa Casa de São Paulo; 2006. 150 p.
18. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41.
19. Mathes SJ, Nahai F. Clinical applications for muscle and musculocutaneous flaps. St Louis: Mosby; 1982.
20. Figueiredo JCA, Freitas AG, Arantes HL. Retalhos musculares e musculocutâneos. In: Mélega JM, Bastos JAV, Mélega LM, eds. Cirurgia plástica, fundamentos e arte, princípios gerais. Rio de Janeiro: MEDSi; 2002. p.121-39.
21. Moore KL. O membro inferior. In: Moore KL. Anatomia Orientada para a Clínica. 2a ed. Rio de Janeiro: Guanabara; 1985.
22. Bourdais-Sallot A, Pare A, Herard C, Duclert-Bompaire M, Pucheux J, Terrier LM, et al. Distally Based Medial Hemisoleus Muscle Flap: Anatomic and Angiographic Study of 18 Lower Limbs. Ann Plast Surg. 2017;79(1):73-8. DOI: 10.1097/SAP.0000000000000997
23. Junior JMC, Maciel LCL, Antonini PA, Bandeira TRS. Retalhos músculo-cutâneo para tratamento de deformidades de membros inferiores. Rev Bras Cir Plást. 2008;23(Supl):95.
1. Hospital Ibiapaba Cebams, Barbacena, MG,
Brazil.
2. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
3. Faculdade de Ciências Médicas e da Saúde,
Suprema, Juiz de Fora, MG, Brazil.
4. Faculdade de Medicina de Barbacena, Barbacena,
MG, Brazil.
5. Faculdade de Medicina, Universidade Federal de
Viçosa, Viçosa, MG, Brazil.
Corresponding author: Emiliano José Canton, Rua Padre Anchieta, nº 48, sala 307 - Centro - Barbacena, MG, Brazil, Zip Code 36200-036. E-mail: emiliano.canton@hotmail.com
Article received: May 18, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.


























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter