

Original Article - Year 2018 - Volume 33 -
Complications of immediate breast reconstruction after total mastectomy using conical and non-conical prostheses
Complicações da reconstrução imediata da mama após mastectomia total com uso de prótese cônica e não cônica
ABSTRACT
Introduction: In the biennium 2016-2017, approximately 2,160
new cancer cases were identified by the Brazilian National
Cancer Institute (Instituto Nacional do Câncer; INCA) for the
state of Ceará and 57,960 new cases for every 100,000 women in
Brazil. Breast reconstruction with alloplastic implants presents
early and late surgical complications directly or indirectly
related to the surgical technique used to perform mastectomy
and implantation of the synthetic material. This study aimed
to analyze the complications found in a group of patients
submitted for immediate breast reconstruction using conical
and non-conical prostheses.
Methods: This is a cross-sectional,
retrospective, observational cohort study that analyzed the
medical records of patients who underwent skin-sparing total
mastectomy with immediate breast reconstruction using conical
and non-conical prostheses, performed by the Plastic Surgery
and Reconstructive Microsurgery Service at the HUWC of the
Federal University of Ceará from January 2016 to 2018.
Results:
A total of 13 (54.1%) patients presented with complications. The
conical prostheses showed the highest number of complications,
i.e., 7 (63.6%) patients, whereas only 6 (46.1%) patients with
non-conical prostheses had complications.
Conclusion: Our
study showed a higher frequency of complications with the
use of conical prostheses when compared to non-conical
prostheses, mainly due to the formation of a sore area at
the tip of the conical prosthesis that resulted in extrusion.
Keywords: Mammoplasty; Breast implants; Breast neoplasms; Reconstructive surgical procedures; Breast
RESUMO
Introdução: No biênio 2016-2017 foram estimados pelo Instituto Nacional do Câncer (INCA)
aproximadamente 2.160 casos novos de câncer para o estado do Ceará e 57.960
casos novos para cada 100.000 mulheres no Brasil. A reconstrução mamária com
implante de material aloplástico apresenta complicações cirúrgicas precoces
e tardias que são direta ou indiretamente relacionadas à técnica cirúrgica
utilizada para a realização da mastectomia e a implantação do material
sintético. O presente estudo tem por objetivo analisar as complicações
encontradas em um grupo de pacientes submetidas à reconstrução mamária
imediata com uso de prótese cônica e não cônica.
Métodos: Corresponde a um estudo de coorte transversal, retrospectivo, observacional
com análise de prontuário de pacientes que foram submetidos à mastectomia
total poupadora de pele com reconstrução imediata da mama com o uso de
prótese cônica e não cônica, no período de janeiro de 2016 a janeiro de
2018, realizada pelo Serviço de Cirurgia Plástica e Microcirurgia
Reconstrutiva do HUWC da Universidade Federal do Ceará.
Resultados: As complicações ocorreram em 13 (54,1%). A prótese que apresentou o maior
número de complicações foi a de formato cônico, com complicações em 7
(63,6%) pacientes, enquanto somente 6 (46,1%) pacientes com prótese de
formato não cônica apresentaram complicações.
Conclusão: O nosso estudo mostrou maior frequência de complicações com o uso de próteses
cônicas em relação à não cônica devido principalmente à formação de uma área
de sofrimento na ponta da prótese cônica que resultou em extrusão das
mesmas.
Palavras-chave: Mamoplastia; Implantes de mama; Neoplasias da mama; Procedimentos cirúrgicos reconstrutivos; Mama
INTRODUCTION
Breast cancer is the most common non-cutaneous malignancy among women worldwide, accounting for approximately 28% of new malignant tumor cases each year in Brazil. In the biennium 2016-2017, the Brazilian National Cancer Institute (Instituto Nacional do Câncer; INCA) estimated approximately 2,160 new cases in the state of Ceará and 57,960 new cases of breast cancer for every 100,000 women in Brazil1.
The breasts represent one of the most eloquent symbols of female sexuality, adorning the female body, and any condition that compromises its structure brings serious consequences to the patient’s physical and psychological well-being.
The high incidence of breast cancer and the importance of the breasts for a good quality of life in patients made breast reconstructions after mastectomy an integral part of the cancer treatment plan.
In 1894, William Halsted published in the United States the technique known today as classical radical mastectomy, which relies on total withdrawal of the breast with an adequate margin of safety in the adjacent skin and subcutaneous tissue, in monobloc, by removing the pectoralis major and minor muscles and the adipose tissues in the region, which includes the axillary lymph nodes2. However, this technique greatly compromised breast reconstructions as the skin was not preserved.
Over the years, more conservative techniques have emerged, such as the one advocated by Patey, which preserves the pectoralis major muscle, and the Madden technique, which preserves both the pectoralis muscles.
To progressively perform more conservative mastectomies, the skin-sparing mastectomy was developed, which may or may not preserve the nipple-areola complex (NAC) and emerged as a procedure that improved the reconstructed breasts, using no less complex techniques, but less debilitating for the reconstruction, through implants with alloplastic material. Preservation of the breast skin envelope provides a satisfactory color tone, texture, and contour of the reconstructed breast, either with a tissue expander, alloplastic implant, lipografting, or deepidermized flaps2.
The use of prosthetic implants for breast reconstructions started in the early 1960s with implants filled with silicone gel. Over the years, implant technology and surgical techniques have evolved, resulting in an improved quality of the reconstructed breast3.
Alloplastic implants can be classified according to shape (round, natural, anatomical, and conical), texture (smooth, textured, and coated with polyurethane foam), and projection (high, extra-high, moderate, and low)4. The choice of implant is fundamental to the normal and natural shape, providing more femininity to the thorax.
Breast reconstruction with an alloplastic implant presents early and late surgical complications that are directly or indirectly related to the surgical technique used to perform mastectomy and implantation of a synthetic material.
OBJECTIVE
To analyze the complications found in a group of patients submitted for immediate breast reconstructions using conical and non-conical prostheses performed in our service from January 2016 to 2018.
METHODS
This is a cross-sectional, retrospective, observational cohort study that analyzed the medical records of patients who were submitted for skin-sparing total mastectomies due to breast cancer, with immediate breast reconstruction using an extra-high conical prosthesis coated with polyurethane or a non-conical prosthesis, performed by the Plastic Surgery and Reconstructive Microsurgery Service at the Walter Cantídio University Hospital of the Federal University of Ceará, in Fortaleza, CE.
Patients who had an outpatient follow-up of at least 6 months and whose reconstruction did not require local or distant skin flaps were included. Those who had an outpatient follow-up of <6 months or those who used local or distant flap for breast reconstruction were excluded.
All breast implants were placed in the submuscular position, using the pectoralis major muscle and serratus anterior muscle to create the pocket, followed by muscular suture to connect the edges after placing the prosthesis. To finish the procedure, the subcutaneous region was drained using a vacuum, which was removed after a daily rate of ≤30 mL of the sero-hematic secretion was achieved.
RESULTS
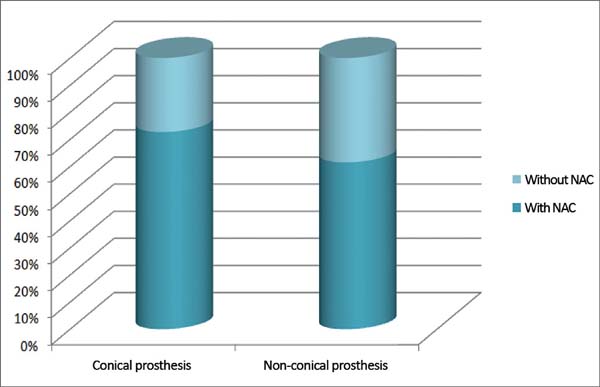
The mean age of the patients was 47.1 years, ranging from 27 to 71 years. Immediate total breast reconstruction using a direct prosthesis after mastectomy due to breast cancer was performed in 24 patients, with 13 (54.2%) reconstructions performed with non-conical prostheses and 11 (45.8%) with conical prostheses. The NAC was preserved in 8 (72.7%) patients with conical prostheses and in 8 (61.5%) with non-conical prostheses; however, the NAC in 3 (27.3%) patients with conical prostheses and in 5 (38.5%) with non-conical prostheses was not preserved (Figure 1).
Regarding the reconstructed side, 12 procedures were performed on the right breast and 12 on the left breast.
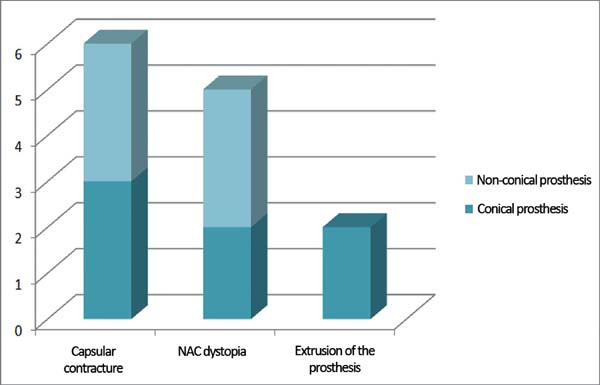
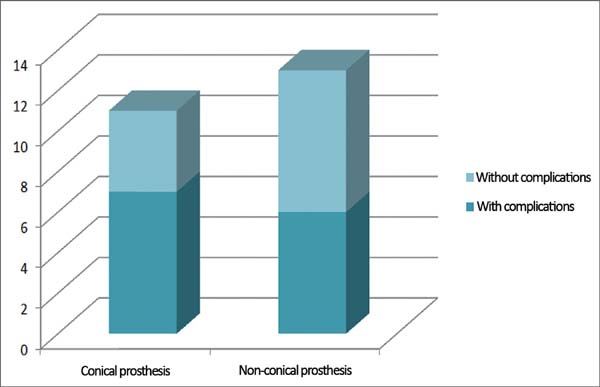
Complications occurred in 13 (54.1%) patients, with capsular contracture that occurred in 6 (25%) patients as the most common (Figure 2). In patients with conical prostheses, 3 experienced capsular contractures, 2 NAC dystopias (Figure 3) and 2 sore flaps with the formation of a hyperemic halo (Figure 4), similar to a pressure ulcer at the tip of the conical prosthesis, which resulted in extrusion (Figure 5) and prosthesis removal. In patients with non-conical prostheses, 3 capsular contractures and 3 NAC dystopias occurred (Figure 6).
No infection or death was found in this group of patients. Regarding the preservation of NAC, 8 (50%) patients with preserved NAC had complications, whereas 5 (62.5%) patients with no preserved NAC had complications.
No difference in the frequency of complications was observed between the right and left breasts, since both presented an incidence of 50% of complications. Conical prostheses presented the highest number of complications, with complications in 7 (63.6%) patients, whereas only 6 (46.1%) patients with non-conical prostheses had complications (Figure 7). In 6 patients submitted for radiotherapy, 2 (33.3%) had capsular contracture as a complication, whereas among the 18 patients who did not undergo radiotherapy, 4 (22.2%) had capsular contracture.
DISCUSSION
In the recent years, breast reconstruction for the treatment of breast cancer has become essential for mastectomized patients due to its proven psychological and physical benefits, because it allows faster return to social life, in addition to an improved immunity, thus contributing to a more favorable prognosis5,6.
Choosing the format of the prosthesis directly influences the shape of the reconstructed breast, providing a better superomedial projection in round prostheses, a better anterior projection in conical prostheses and a more natural appearance in anatomical prostheses for more hypotrophic breasts.
In this study, complications occurred in 54.1% of patients using the alloplastic material, which is higher than most breast reconstruction services, with the incidence ranging from 30% to 43%7,8.
The most common complication identified was capsular contracture, which occurred in 6 (25%) patients, which is similar to that found in the researched literature, ranging from 0.5% to 30%9,10.
The most serious complication identified was prosthetic extrusion that required removal of the prosthesis that occurred in 2 patients who used the conical prosthesis, representing 18.1% of the patients. This incidence was higher than that of a previous study, which ranged from 1.2% to 5.3%, and higher than those using non-conical prostheses, in which no cases of prosthetic extrusion were observed11.
Extrusions occurring in the conical prostheses initially evolved from a sore area (local hyperemic halo) formed in the myocutaneous flap on the tip of these conical prostheses, with characteristics similar to pressure ulcers (Figures 4 and 5).
CONCLUSION
Immediate breast reconstructions with silicone prostheses is an excellent option for selected patients, considering the low complexity of the procedure and short surgical time; however, the disease severity, associated with the surgeon’s experience in performing the mastectomy and the skin flap thickness, may weaken the cutaneous cover of the prosthesis, which promotes extrusion.
Our study showed a higher frequency of complications in immediate breast reconstructions with conical and non-conical prostheses when the NAC was not preserved and when the patient is submitted for radiotherapy, which were observed in patients using conical prostheses. This condition mainly occurs due to the formation of a sore area at the tip of the conical prosthesis that resulted in extrusion.
COLLABORATIONS
|
ROR |
Analysis and/or interpretation of data; statistical analysis; funding applications; data collection; study design; resource management; research; methodology; and writing (preparation of the original manuscript). |
|
SGPP |
Final approval of the manuscript; conceptualization; project management; writing (review and editing); supervision; and observation. |
REFERENCES
1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Estimativa 2016: Incidência de Câncer de Mama no Brasil. Rio de Janeiro: INCA; 2016. [acesso 2018 Mar 12]. Disponível em: http://santacasadermatoazulay.com.br/wp-content/uploads/2017/06/estimativa-2016-v11.pdf
2. Mélega JM. Cirurgia Plástica Fundamentos e Arte: Princípios Gerais. 2a ed. Rio de Janeiro: Guanabara Koogan; 2011.
3. Grabb WC, Smith JW. Cirurgia Plástica. 6a ed. Rio de Janeiro: Guanabara Koogan; 2009.
4. Pitanguy I. Cirurgia Plástica: Uma visão de sua amplitude. 1a ed. São Paulo: Atheneu; 2016.
5. Veiga DF, Veiga-Filho J, Ribeiro LM, Archangelo I Jr, Balbino PF, Caetano LV, et al. Quality-of-life and self-esteem outcomes after oncoplastic breast-conserving surgery. Plast Reconstr Surg. 2010;125(3):811-7.
6. Bellino S, Fenocchio M, Zizza M, Rocca G, Bogetti P, Bogetto F. Quality of life of patients who undergo breast reconstruction after mastectomy: effects of personality characteristics. Plast Reconstr Surg. 2011;127(1):10-7.
7. Almeida Júnior GL, Macedo JLS, Borges SZ, Souza AO, Henriques FAM, Suschino CMH, et al. Reconstrução mamária imediata após cirurgia conservadora do câncer de mama. Rev Soc Bras Cir Plást. 2007;22(1):10-8.
8. Bronz G, Bronz L. Breast reconstruction with skin-expander and silicone prostheses: 15 years' experience. Aesthetic Plast Surg. 2002;26(3):215-8.
9. D'Alessandro GS, Povedano A, Santos LKIL, Santos RA, Góes JCS. Reconstrução mamária imediata com retalho do músculo grande dorsal e retalho de silicone. Rev Bras Cir Plást. 2015;30(2):163-71.
10. Mathes SJ, Hentz VR. Plastic surgery. 2a ed. Philadelphia: Saunders; 2006. p. 26-33.
11. Farah AB, Nahas FX, Mendes JA. Reconstrução mamária em dois estágios com expansores de tecido e implantes de silicone. Rev Bras Cir Plást. 2015;30(2):172-81.
1. Hospital Universitário Walter Cantídio,
Universidade Federal do Ceará, Fortaleza, CE, Brazil.
Corresponding author: Rogério de Oliveira Ribeiro, Rua Odilardo Silva, nº 81 - Laguinho - Macapá - AP - Brazil , Zip Code 68908-182. E-mail: roimed@yahoo.com.br
Article received: August 5, 2018.
Article accepted: October 4, 2018.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter