

Articles - Year 1999 - Volume 14 -
Baldness Surgery: A New Approach and a New Surgical Instrument
Cirurgia da Calvície: Abordagem Pessoal e Novo Instrumental
ABSTRACT
A personal approach to the treatment of baldness through a simple and efficient technique, set on basic principles such as marking of the anterior line, single-hair-graft in the first anterior lines and non traumatic precise technique. A new scalpel cable (idealized by the author) in which a common needle is enclosed. This instrument facilitates a more precise surgical maneuver besides allowing fine and less traumatic procedure.
Keywords: Baldness; single-hair-graft; needles; new instrument.
RESUMO
O autor apresenta a sua abordagem pessoal no tratamento da calvície e os resultados obtidos com uma sistematização simples e eficiente. Enfatiza a necessidade de uma técnica refinada alicerçada em princípios básicos que vão desde a marcação da linha anterior enxertos de um só fio nas primeiras linhas anteriores, passando por técnica atraumática e precisa. Apresenta, detalhadamente, um novo cabo de bisturi (idealizado pelo autor) em que se encaixam agulhas comuns de injeção, estas definitivamente incorporadas ao arsenal do autor para a cirurgia da calvície. O novo instrumental facilita o manuseio preciso do cirurgião além de possibilitar um procedimento mais requintado e muito menos traumático.
Palavras-chave: Calvície; "single-hair-graft"; agulhas; novo instrumental.
Baldness has been a serious problem for men since ancient times. Julius Caesar used a laurel wreath to mask his bald head. Egyptian papyrus older than 5 thousand years had already registered methods for avoiding baldness.In 400 BC Hippocrates noted that eunuchs didn't suffer from gout and generally didn't become bald.
These observations show that men have been worried about this matter for a very long time. Hippocrates observations called so much attention that even today many authors believe that 3 factors (genetic, age and basically endocrino) interact in the development of bald baldness, contributing to Orentreich's(l) studies which show that a dominating sex limited gene is responsible for the noxious action of dihydrotestosterone in certain strategically
placed folliculus pili, in the fronto-parieto occipital region of the scalp, which determines a reduction of hair growth, an anatomical transformation of hair for the bulb's atrophy and finally the loss of the hair as the patient gets older.
Baldness isn't thus only a consequence of the loss of folliculus pili, but a genetic steroid related to time and it manifests as a reduction of hair growth. It's important to notice that Orentreich's(l) findings are related to the common male baldness only.
Nowadays it is widely known that half of the male population in the world is or will be bald in a near future. Nonetheless, the number of baldness surgeries has grown in a geometrical progression due to the good and natural results of new techniques.
Although these techniques present very natural results, some patients will have to wait for biochemical or genetic treatments.
MATERIAL AND METHODS
Baldness surgery is clearly divided into two different stages: before and after Orentreich(l), and with Juri(2), Vallis(3), Chajchir(4), Kaminsky(S), Curi(6) and Uebel(7) contributions, the surgical techniques reached a very good acceptance by both physicians and patients, due to Nordström(8), whose initial idea allowed Curi(6) to develop his known micrograft technique.
We have applied Curi's(6) technique with Uebel's(7) and our own modifications in the treatment of androgenetic baldness, scalp burns sequelae or irreversible acquired alopecia. Patients' age ranged from 20 to 65, of which 48% were between 25 and 35. 92% of the cases were male.
The patient's profile for better results is: highly dense donator area, baldness type 1 to 5 (according to Norwood's(9) classification) and age ranging from 30 to 40 years old.
TECHNIQUE
DONATOR AREA
The patient is placed in ventral decubitus, with a comfortable thoracic position, brow supported by a comfortable foam pillow and free nose. An imaginary line is traced in the occipital region, tangent to the upper pole of both ear's anthelix, which is the upper limit of the incision for the removal of the pilose line. Next, scalp is cut from the upper limit until 1.5 cm below, which determines its height (the length of the cut hair is about 0.5 cm) in order to facilitate its positioning in the receptor area (Fig. 1).
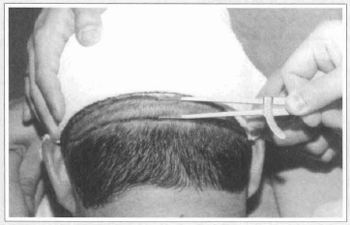
Fig. 1 - Marking of the donator area showing positioning, length and width of the ellipsis and the 0.5 cm hair cut.
In the second surgical step the width of the incision is 1.0 cm and the resulting scar of the first surgical step will be the upper limit. Usually, the length of incision is the distance between both ears. Depending on the circumstances, it can extend untill the temporal region in a classical "boomerang" marking.
Scalp's antisepsis is made with aqueous chlorhexidine. The elliptical line is marked with methylene blue. No more than 10 ml of local 1.5% Xylocaine with adrenaline anesthesia is infiltrated. Classical scalp bevel incisions and careful supragalea dissection. Hemostasia and synthesis with continuous stitching using 4.0 blue Mononylon stitches.
GRAFTS PREPARATION
A rigid plastic board and a resistant autoclave were used. The area was divided in half along its length with a #22 scalpel. Each half was sliced in parallel incisions measuring approximately 2.0 mm (Fig. 2a). Each slice was operated with a #11 scalpel in order to separate the excessive adipose layer right below the bulb's base, but always keeping it immersed in the tissue. Then, micrografts (2 to 3 hairs) and minigrafts (3 to 5 hairs) were prepared obeying the anatomical inclination of the capillary unit, making parallel oblique cuts (Fig. 2b). For the preparation of single-hair-grafts used in the anterior
lines it is necessary to use a magnifying glass. The donator area and all prepared grafts must be holded under small sterile wood sticks such as disposable tongue depressors, frequently humidified with saline solution spray but never immersed in it. Surgical procedure can be facilitated and dynamized by a rigorous control of each graft's quality and the side-by-side disposal of the grafts in the sticks, in a position that makes the surgeon's assistant's movements easier for the introduction of the grafts in the receptor site (Fig. 2c).
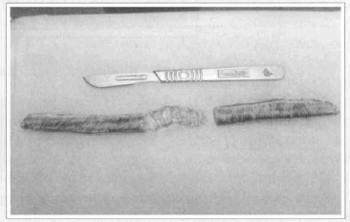
Fig. 2a - Scalp divided in half showing the confection of the slices.
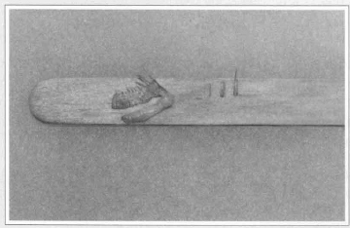
Fig. 2b - Separation of excessive amount of fat from the slice of scalp and examples of "singIe-hair", micro and minigrafts.
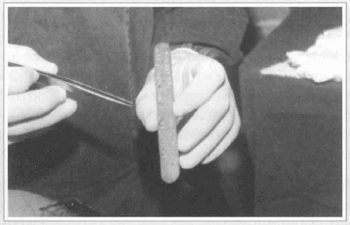
Fig. 2c -Auxiliary ready for grafts implantation. Notice the wood stick, grafts placed in the introduction position, and the straight clamps.
ANTERIOR LINE MARKING
This is the decisive moment for good results. The anterior line shape must be previously discussed with the patient in order to acquire the most natural shape keeping a certain degree of baldness. It's design is characterized by broken lines, as proposed by Basto(lO), allowing an extraordinary natural look besides the correct positioning of the frontal upper limit of the anterior line, theoretically located from 2.0 to 2.5 mm above the upper frontal sulcus (Fig. 3).
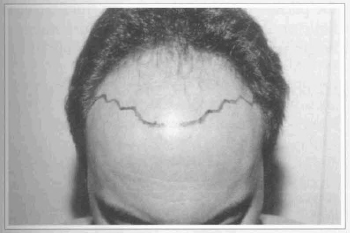
Fig. 3 - Marking of the anterior line with broken traced lines. Aesthetical maintenance of hair shape.
RECEPTOR AREA
The patient must feel comfortable in dorsal decubitus.
Anesthesiologist assisted sedation is important to dissociate the patient from the surgical environment and therefore reduce its stress level and its unfavorable consequences, facilitating further maneuvers. Scalp and face antisepsis is followed by the anterior line marking with methylene blue. The receptor area is divided in 4 to 6 quadrants which are individually operated, bilaterally from the anterior to the posterior portion (Fig. 4). Local anesthesia is infiltrated and turned in each quadrant to be operated. No blocks were performed. A special scalpel cable was figured by the author, which is similar to the shape of a pen in which two kinds of needles can be adapted, 40/12 and 40/16 (Figs. 5a & 5b).

Fig. 4 - Marking of the receptor area in quadrants. In the crown area, marking and disposal of the grafts must be done in a spiral shape.
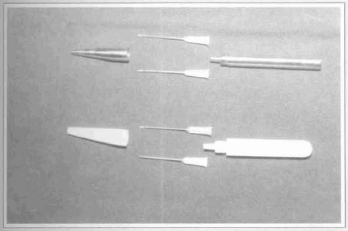
Fig. 5a - New scalpel for baldness surgery. Note the common needles setting and protector cover, similar to a pen.
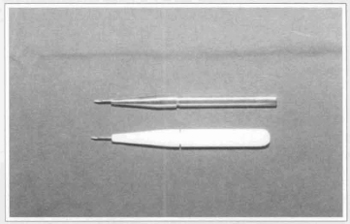
Fig. 5b - Mounted scalpel. It is similar to a pen.
Single hair grafts are used in the first three anterior lines, placed side by side 2 mm far from each other using 40/12 needles. In the second and third lines hair grafts are placed in a "theatre chair" shape, also 2 mm distant (bilaterally and antero-posterior) from each other.
In the next lines only the size of the grafts (micro or mini) and the needle's gauge (40/16) change.
The needle is perpendicularly introduced into the scalp, with the bezel laterally to the left until it disappears in the tissue's depth. Then, the needle is pulled back until the bezel appears. Scalpel's cable is turned 90° to the right in order to open the orifice and to expose the bezel (Fig. 6). The graft must be disposed in such a manner that allows its growth upwards. The needle is carefully removed and the procedure is repeated.
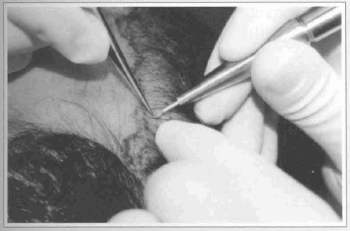
Fig. 6 - Detail of the graft introduction technique. Note the excellent hilt provided by the scalpel cable.
During the placement of the next graft, the previously placed graft is held using the tip of the surgeon's left pointer finger in order to keep the previous one in its new location. Depending on how extensive the bald area is, about 20 needles are replaced in a surgery.
Grafts are hydrated many times during the surgery using an sprayer with saline solution, which also helps keeping them free from hematic scabs (Fig. 7).
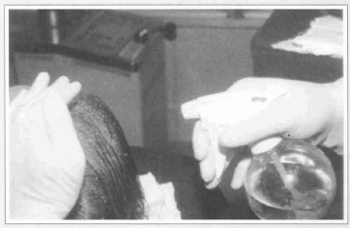
Fig. 7 - Saline solution sprayer used during the surgery.
This strategy in grafts introduction brings many significant improvements to the surgical act, such as:
1. Reduces the orifice's size compared to the ones made with scalpels blade # 11 and therefore it contributes to the disappearance of those undesired skin elevations around the hair, resulting from scar which are very common in the postoperative as patients complain.
2. Significantly reduces transoperative bleeding.
3. Facilitates the placement of the grafts closer to each other, improving the hair density in the operated area.
4. Facilitates the placement of the grafts in areas with pre-existing hair, avoiding the loss of remaining hair.
5. Facilitates the job of the surgeon's assistant in the introduction and guidance of the hair through the needle's bezel.
6. Allows more comfort to the surgeon due to the new scalpel cable designed by the author.
7. Reduces the incidence of postoperative edema.
8. Significandy improves the surgery's final result, mainly in the most anterior lines (Figs. 8e & 8f).
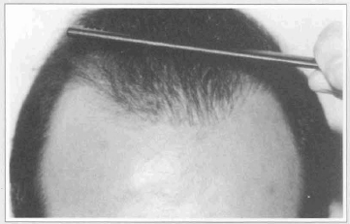
Fig. 8e - In the frontal detail it is possible to notice the natural results of the grafts and the absence of scars around it.
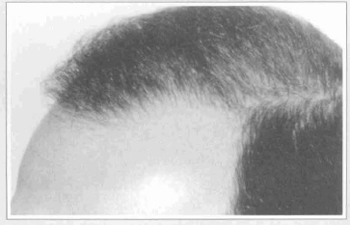
Fig. 8f - Natural results. Left oblique view.
THE PLASTER
Sterile gauzes with vaseline are used on the grafts of the donator area. Then a thick layer of open gauzes are fixed with 15 cm adhesive bands with medium compression. The plaster is removed 48 hours later, and the operated area is liberated for bath using hexachlorophene based liquid soap. Stitches are removed 12 days postoperative. It is recommended not to remove some hematic scabs before 7 days PO. Afterwards the scab's removal is easier and should always be done carefully, preferably with humid hair.
THE NEW SURGICAL INSTRUMENT
Designed by the author and named by the manufacturer "Leão's scalpel" for baldness surgery, this new instnunent, similar to the shape of a pen, works as a cable for the connection of needles of different gauges used in the introduction of the grafts. It is made of a removable extremity that protects the needle, allowing only its 1/3 distal apparent. This provides the surgeon with comfort and steadiness for the movements of perforation and rotation as described by the author. Replacement of the needles is done the same way as the refill of a pen. The instrument is made of two different materials stainless steel or Teflon - it is light, comfortable and perfectly fits the surgeon's hand, facilitating the previously described surgical maneuvers (Figs. 5a & 5b).
COMMENTS & CONCLUSION
Based on our personal experience and preoperative interviews with patients, we concluded that the bald patient's profile according to age is the following: between 20 and 30 years old the patient wishes not only to correct the baldness, but also to have a high capillary density. They are demanding and frequendy return for the second and third surgical steps necessary to meet this objective (Figs. 8a - 8f). Men between 35 and 45 look forward to loosing the "baldheaded" stigma, which can be obtained in a single surgical step (Figs. 9a & 9b). Half of these cases return for a second surgery in order to improve their capillary density. For those patients between 50 and 65, having hair again decreases their sensation of "loss". Being able to use a comb again is a sort of conquest, what makes a second surgical step very infrequent in these cases (Figs. lOa - lOd).
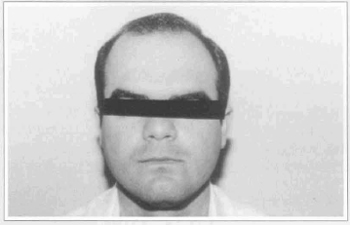
Fig. 8a - 28 years old patient anterior preoperative view. Notice the very thin hair.

Fig. 8b - 8 months postoperative view after the second surgical step.
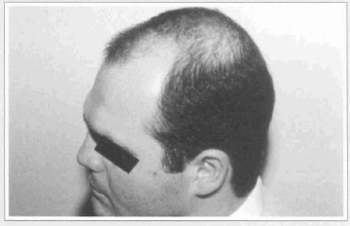
Fig. 8c - Preoperative left oblique view.
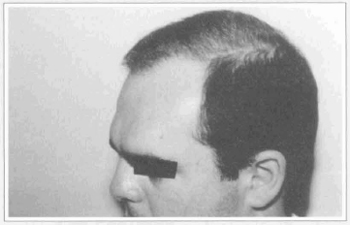
Fig. 8d - 8 months postoperative view after the second surgical step.
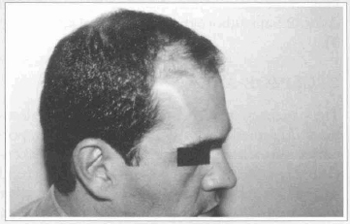
Fig. 9a - 39 years old patient in left oblique view. Thick hair type.
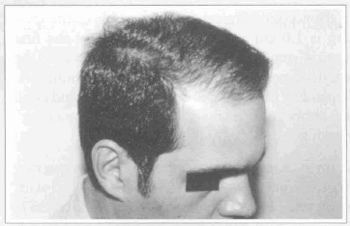
Fig. 9b - 8 months postoperative, after the first surgical step.
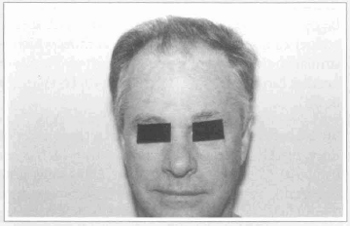
Fig. lOa - Preoperative anterior front view of a 62 years old patient with very thin and gray hair.
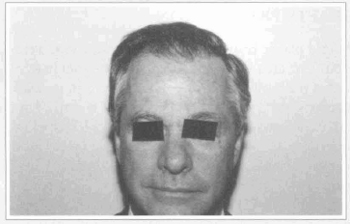
Fig. lOb - 8 months postoperative, after the first surgical step.
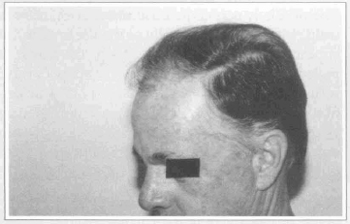
Fig. lOc - Preoperative right oblique view.
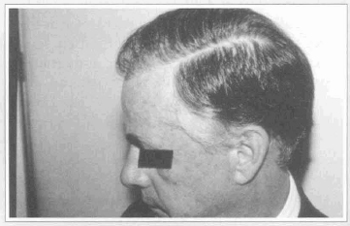
Fig. 10d - 8 months postoperative., after the first surgical step.
The surgeon must be very frank about the need for a second, third or even a fourth surgical step in order to let the patient correctly figure out what his chances are for achieving the best result possible.
When androgenetic alopecia is treated, patience should replace immediatism. It is important both for the surgeon (regarding the surgical approach, the time for achieving the desired result and the interval between surgical steps) and the patient, because the final results will be visible at least 8 months postoperative.
This new approach for the treatment of alopecia, due to the introduction of new instruments and the adoption of less traumatic techniques, brings more refined and natural results, besides an efficient and less aggressive dynamic in pre and postoperative, that can be observed in a better recovery of the patient.
REFERENCES
1. ORENTREICH N. Hair transplantation long term results and new advances. Arch. Otolayng. 1970; 92:576-82.
2. JURI J. Use of Parieto occiptal flaps in the Surgical Treatment of Baldness. Plast. Reconstr. Surg. 1975; 55:456.
3. VALLIS CP. Hair transplantation for male pattern baldness. Surg. Clin. N. Am. 1971; 51:519.
4. CHAJCHIR A & BENZAQUEN I. Tratamiento Quirúrgico de la Calvicie. Consideraciones para la e1ección de pacientes. Prensa Méd. Argentina. 1973; 60(27):962.
5. KAMINSKY A. & SEGERS MA. Autoinjertos cutaneos en la tratamiento de las alopecias. Consideraciones sobre su técnica. Rev. Arg. Dermat. 1965; 57: 133.
6. CURI M. Tratamento da calvície masculina com mini-enxertos. Revista da Soc. Bras. Cir. Plastica. 1990; v. 23 n. 5, 68.
7. UEBEL C. Micrografts and minigrafts : A new approach for Baldness surgery. Ann. Plastic Surg. 1991; 27:476-487.
8. NORDSTRON REA. "Micrografts"for the improvement of the front hairline after hair transplantation. Aesthetic. Plast. Surg. 1981; 5:9.
9. NORWOOD OT, SHIELL RC. Hair transplant surgery, ed. 2, Springfield, ILL, 1984, Charles C. Thomas.
10. BASTO F, LEMOS P. Abordagem pessoal da linha pilosa anterior. Nova contribuição a microenxertia capilar. Atualização em Cirurgia Plastica. Editores: Tournieux e Curi. Robe Editorial, São Paulo. 1996; 113-124.
I - Membra Titular da Sociedade Brasileira de Cirurgia Plastica.
Address for correspondence:
Carlos Eduardo Guimarães Leão, MD
R. do Mosteiro, 105/202
30380-780 - Belo Horizonte - MG Brazil
Phone: (55 31) 337-1041 and (55 31) 9981-5954
e-mail: leao@digiopen.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter