

Case Report - Year 2018 - Volume 33 -
Umbilical endometriosis: a case report and literature review
Endometriose umbilical: relato de caso e revisão de literatura
ABSTRACT
Endometriosis is characterized by the presence of endometrial tissue outside the uterine cavity. The pathophysiology of this condition is poorly understood. However, several hypotheses have been proposed, including the spread of endometrial cells via hematogenous or lymphatic routes. The clinical presentation is variable but includes a palpable nodule, cyclic bleeding, and changes in the color of the skin in the affected region. Diagnosis is established by clinical examination combined with imaging and lesion biopsy. The treatment of choice is surgical, with excision of the lesion and tissue reconstruction. We report the case of a 35-year-old female patient with umbilical endometriosis and the need for removal of the lesion with umbilical reconstruction. The presentation of this condition determines the diagnostic and management approach. Therefore, the exclusion of other benign or malignant disorders is essential.
Keywords: Endometriosis; Plastic surgery; Reconstructive surgical procedures; Umbilicus; Rare diseases
RESUMO
A endometriose é caracterizada pela presença de tecido endometrial fora da cavidade uterina. Seu mecanismo fisiopatológico é pouco esclarecido, mas várias hipóteses são descritas - dentre elas a disseminação de células endometriais por via hematogênica ou linfática. A apresentação clínica é bastante variável, mas podem estar presentes massa palpável, sangramentos cíclicos ou alterações de coloração da pele na região afetada. O diagnóstico é estabelecido a partir do exame clínico, associado a exames de imagem e biópsia da lesão. O tratamento de escolha é o cirúrgico com excisão da lesão e reconstrução da anatomia local. Apresentamos um relato de caso de uma paciente de 35 anos, com endometriose umbilical, com necessidade de excisão da lesão e confecção de novo umbigo. A evolução da afecção descrita é estritamente relacionada ao manejo diagnóstico e propedêutico instituído; sendo assim, a exclusão de diagnósticos diferenciais, benignos ou malignos, é de suma importância.
Palavras-chave: Endometriose; Cirurgia plástica; Procedimentos cirúrgicos reconstrutivos; Umbigo; Doenças raras
INTRODUCTION
Endometriosis is characterized by the presence of endometrial tissue outside the uterine cavity1. This condition affects approximately 12% of women of reproductive age2, and the primary sites of involvement are the ovaries, sacrum, broad ligaments of the uterus, uterosacral ligaments, fallopian tubes, sigmoid colon, appendix, and round ligaments of the uterus1. Umbilical endometriosis represents 0.5% to 1% of all cases2. Malignant complications are rare, corresponding to 1% of all cases3.
In this study, we describe a patient with umbilical endometriosis, and review the diagnosis and treatment.
CASE REPORT
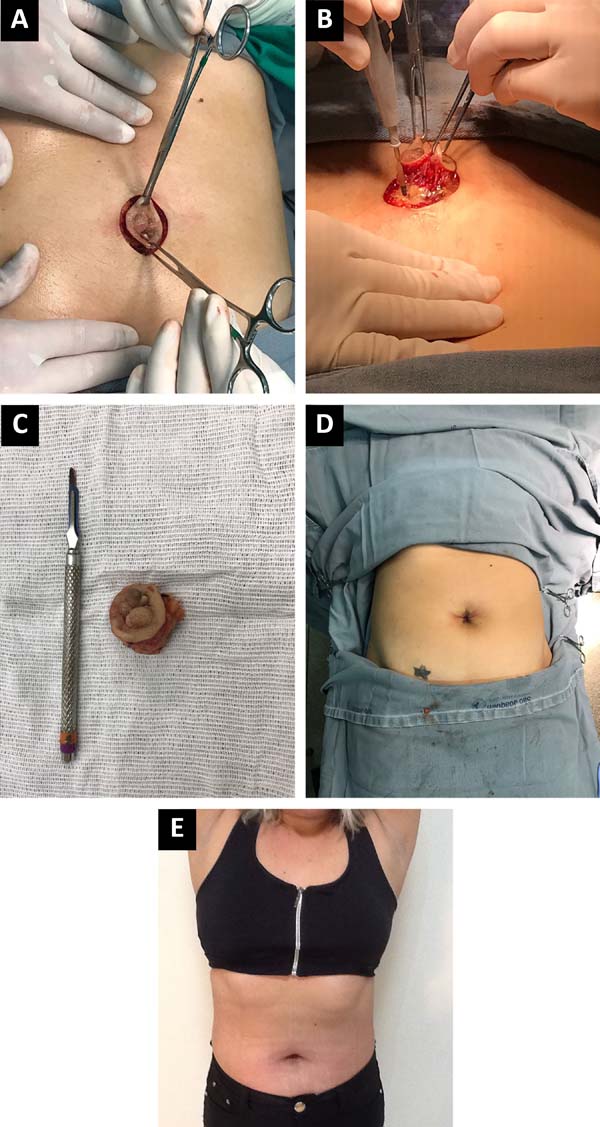
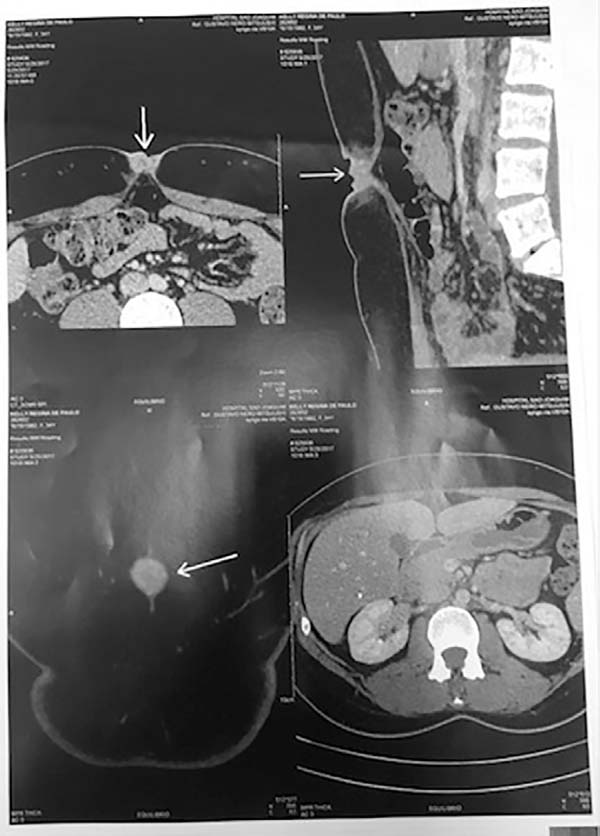
A 35-year-old woman was referred to the Plastic Surgery Department of the São Joaquim Hospital of Franca, Franca, São Paulo state, Brazil, with umbilical vegetative lesions that appeared 6 months prior. Physical examination indicated the presence of a primary lesion that was painful to palpation and surrounded by 2 smaller lesions, all of which were associated with bleeding and pain during the menstrual period (Figure 1). Computed tomography of the abdomen showed an umbilical nodule compatible with probable umbilical endometriosis (Figure 2).
The biopsy of the primary lesion revealed the presence of skin associated with stromal fragments and endometrial glands with no signs of malignancy. Umbilical endometriosis was confirmed by analysis of clinical data, tomography scans, and biopsy, and excision of the lesion with a safe margin was proposed (Figures 3a, b, and c). The biopsies were subjected to histopathological examination. The final appearance after umbilical reconstruction is shown in Figures 3d and 3e.
DISCUSSION
Cutaneous endometriosis is rare and is related to previous surgical procedures in most cases. This condition is classified as primary when it occurs spontaneously, as in the current case. The most common cutaneous manifestation is umbilical, occurring in 34% of cases1,4,5.
Several hypotheses have been proposed to explain the pathophysiology of primary umbilical endometriosis. The most accepted hypothesis in women with concomitant pelvic endometriosis is embolization of endometrial tissue via hematogenous or lymphatic routes. However, metaplasia of Müllerian duct remnants is more likely in patients with cutaneous endometriosis and may be due to inflammatory, hormonal, or traumatic causes2,4.
These lesions may present with specific symptoms, including a palpable erythematous or violaceous nodule of a brownish color with increased volume, and cyclical bleeding and pain during the menstrual period. These lesions may be asymptomatic, in which case the diagnosis is more difficult2,4. In the current case, the patient presented signs and symptoms consistent with previous reports, including a brown and violaceous nodule associated with pain and bleeding during the menstrual period.
The diagnosis is established by a compatible clinical picture and complementary examinations. Ultrasound can be performed and reveals a cystic appearance. Computed tomography and magnetic resonance imaging are better for delimiting the lesion and making a differential diagnosis1,2.
Although several methods for diagnosis are available, biopsy is the most reliable and useful. This histopathological examination reveals the presence of endometrial tissue, with endometrial glands lined by pseudostratified columnar epithelium, which may present active secretion or free erythrocytes. Immunohistochemistry can be used to assess the presence of estrogen and progesterone receptors, which further confirms the diagnosis2,4.
Differential diagnosis should be made for benign and malignant lesions, including hernias, entrapment of ilioinguinal or iliohypogastric nerves, umbilical polyp, melanocytic nevus, suture granuloma, hemangioma, omphalitis, melanoma, adenocarcinoma, squamous cell carcinoma, and basal cell carcinoma1,2,5.
The treatment of choice is surgical, with complete excision of the lesion and umbilical reconstruction if necessary. The nodule should be removed with safe margins to prevent lesion recurrence. After the procedure, clinical treatment with oral contraceptives or other hormonal agents may be implemented to prevent recurrence1,2,4.
The evolution is benign in most cases. However, in a few cases, carcinomatous transformation may occur, requiring frequent assessment4.
CONCLUSION
The described approach has an excellent prognosis and low risk of malignancy. This favorable evolution depends on adequate management of the patient. Moreover, accurate differential diagnosis (for benign or malignant lesions) is essential to determine appropriate treatment.
COLLABORATIONS
|
CBM |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
AMG |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
ACV |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
ARM |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
BAA |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
ADBM |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
ABFB |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
AAR |
Analysis and/or interpretation of data; final approval of the manuscript; writing the manuscript or critical review of its contents. |
|
GNM |
Analysis and/or interpretation of data; final approval of the manuscript; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
REFERENCES
1. Federação Brasileira das Associações de Ginecologia e Obstetrícia (FEBRASGO). Manual de endometriose. São Paulo: FEBRASGO; 2015.
2. Jaime TJ, Jaime TJ, Ormiga P, Leal F, Nogueira OM, Rodrigues N. Endometriose umbilical: relato de um caso e seus achados dermatoscópicos. An Bras Dermatol. 2013;88(1):121-4. DOI: http://dx.doi.org/10.1590/S0365-05962013000100019
3. Pramanik SR, Mondal S, Paul S, Joycerani D. Primary umbilical endometriosis: A rarity. J Hum Reprod Sci. 2014;7(4):269-71. DOI: http://dx.doi.org/10.4103/0974-1208.147495
4. Fancellu A, Pinna A, Manca A, Capobianco G, Porcu A. Primary umbilical endometriosis. Case report and discussion on management options. Int J Surg Case Rep. 2013;4(12):1145-8. DOI: http://dx.doi.org/10.1016/j.ijscr.2013.11.001
5. Garcia AMC, Silveira PS Jr, Garcia BGBC, Assis MG. Endometriose cutânea umbilical: Relato de caso e revisão da literatura. ACM Arq Catarin Med. 2009;38(Supl. 1):254-6.
1. Acadêmica em Medicina, Universidade de Franca,
Franca, SP, Brazil.
2. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
3. Associação Médica Brasileira, São Paulo, SP,
Brazil.
Corresponding author: Carla Batista Moisés, Rua João da Silva Ranhel, 1850, Apt. 304, Bloco 1 - Nucleo Agricola Alpha - Franca, SP, Brazil. Zip Code 14403-175. E-mail: carlabmoises@live.com
Article received: November 23, 2017.
Article accepted: June 22, 2018.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter