

Case Report - Year 2018 - Volume 33 -
Reverse sural flap of the fasciosubcutaneous pedicle: a case report
Retalho sural reverso de pedículo fasciossubcutâneo: relato de caso
ABSTRACT
Introduction: Loss of substance in the lower third of the leg usually requires complex surgical procedures for tissue reconstruction. Among the existing options for tissue reconstruction, reverse sural flap of the fasciosubcutaneous pedicle or reverse adipofascial flap, described in the literature as a viable option, has been little studied compared with other techniques. The objectives of this study were to present the results of surgical treatment of a complex injury due to Achilles tendon rupture using the reverse sural flap of the fasciosubcutaneous pedicle concomitantly with total skin grafting and to discuss the advantages of the procedure as well as other surgical alternatives. Case report: A.D., a 28-year-old male patient, presented with a complex injury in the lower third of the leg because of a poor outcome of surgical repair of Achilles tendon rupture that had occurred during an automobile accident more than 30 days previously. The patient underwent injury reconstruction with the reverse sural flap of the fasciosubcutaneous pedicle. The postoperative result was favorable, without complications. Conclusion: The surgical technique described here is satisfactory for treating lesions in the lower third of the leg due to Achilles tendon rupture.
Keywords: Surgical flaps; Leg trauma; Reconstructive surgical procedures; Operative surgical procedures; Ankle trauma
RESUMO
Introdução: As perdas de substância no terço inferior da perna costumam exigir elaboradas
estratégias cirúrgicas para sua reconstrução. Dentre as opções existentes, o
uso do retalho sural reverso de pedículo fasciossubcutâneo ou adipofascial
reverso, citado na literatura como interessante alternativa, é pouco
relatado, se comparado às outras técnicas mais utilizadas. O objetivo deste
estudo é apresentar o resultado do tratamento de uma lesão exposta do tendão
de Aquiles, realizado com retalho sural reverso de pedículo
fasciossubcutâneo, associado à enxertia de pele total no mesmo tempo
cirúrgico, discutindo as alternativas técnicas e as vantagens do
procedimento.
Relato de caso: A.D., 28 anos, portador de lesão complexa em terço distal da perna,
decorrente de evolução desfavorável de procedimento ortopédico de
reconstrução do tendão de Aquiles rompido em acidente automobilístico,
ocorrido há mais de 30 dias, foi submetido à reconstrução da ferida por meio
do retalho sural reverso de pedículo fasciossubcutâneo. A evolução
pós-operatória foi favorável, não havendo complicações ou
intercorrências.
Conclusão: A técnica relatada apresentou uma boa opção com resultado satisfatório para a
cobertura de lesão de terço inferior da perna com exposição do tendão de
Aquiles.
Palavras-chave: Retalhos cirúrgicos; Traumatismos da perna; Procedimentos cirúrgicos reconstrutivos; Procedimentos cirúrgicos operatórios; Traumatismos do tornozelo
INTRODUCTION
Loss of substance in the lower third of the leg, especially Achilles tendon ruptures, which are common after orthopedic surgeries and are challenging for plastic surgeons because of the high rate of complications and occurrences,1-3 usually requires complex surgical procedures for tissue reconstruction2-4.
Several options are available for treating these injuries, and the simplest method is always preferred1,5. The chosen reconstruction strategy should consider the following factors: injury (location, size), donor area, patient (clinical history), and surgery (surgeon’s experience, hospital structure)1.
Among the options available for surgical repair, the use of the reverse sural flap of the fasciosubcutaneous pedicle3,6,7 or adipofascial reverse flap has been reported in the literature as a viable option since more than 20 years7,8; however, this approach has been little studied compared with other techniques. The main advantages of using the proposed technique are the simple and fast execution; sufficient and reliable vascularization; and low morbidity of the donor site, which has an excellent rotation arc9, making this strategy useful in several cases.
The objectives of this study were to present the results of surgical treatment of a complex injury, involving exposure of the Achilles tendon, in the lower third of the leg using the reverse sural flap of the fasciosubcutaneous pedicle concomitantly with total skin grafting and to discuss the advantages of the procedure as well as other surgical alternatives.
CASE REPORT
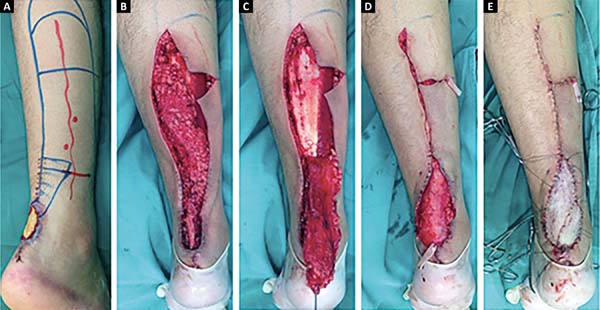
A.D., a 28-year-old male Caucasian patient without comorbidities, presented with a necrotic injury (6.0 × 4.0 cm2) with Achilles tendon exposure in the lower third of his right leg after surgical repair of Achilles tendon rupture that had occurred during an automobile accident. On day 30 after surgery, the patient was referred to our plastic surgery service and underwent surgical debridement (Figure 1).
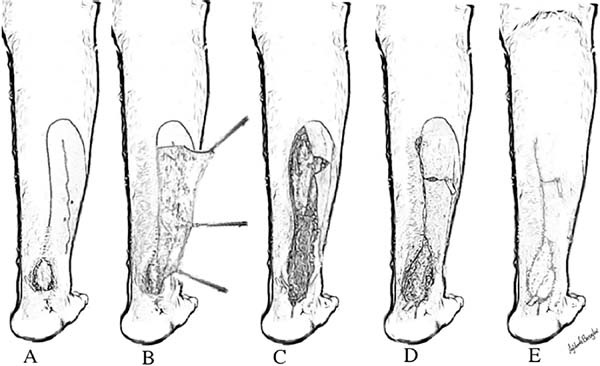
The complex injury was treated 15 days after debridement. With the patient in the prone position and under spinal anesthesia, the operative site in the calf region of the right lower limb was demarcated. The necrotic injury in the lower third of the leg was repaired using the reverse sural flap of the fasciosubcutaneous pedicle, which was fixed without tension, concomitantly with total skin grafting. The skin graft was removed from the ipsilateral popliteal region during flap preparation (Figures 2 and 3).
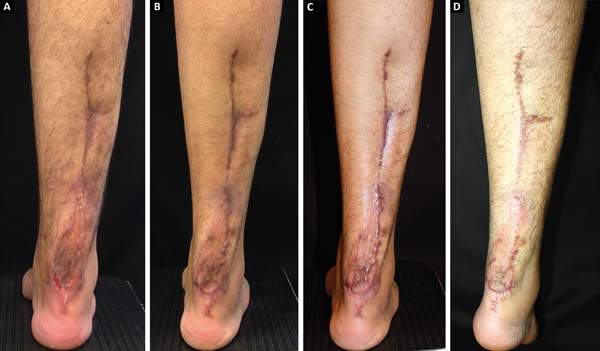
The surgical procedure lasted 90 min and was uneventful. The patient was discharged eight hours after the procedure, without plaster immobilization and required only occlusive dressings. The patient had no relevant motor and sensory deficits or pain and was instructed to avoid walking with a full load for one week. The postoperative period was uneventful, and only occlusive dressings were required. The lesion gradually healed (Figure 4).
DISCUSSION
The need for more effective, easier, and reliable surgical procedures, especially for treating injuries in the distal third of the leg, has been reported by several studies over the years1,7.
Considering the increase in patients’ demands for better surgical outcomes, assessment of the quality of the achieved result has been gaining prominence in the literature and has stimulated more discussions among plastic surgeons and patients2-4.
The reverse sural flap of the fasciosubcutaneous pedicle and the reverse adipofascial flap receive blood supply from the cutaneous perforating branches of the fibular and posterior tibial arteries1. These flaps preserve the sensory innervation of the saphenous, superficial fibular, and sural nerves because only a thin region of the subcutaneous tissue is left under the dermis to avoid injury to the subdermal plexus of the donor region, whereas most of the subcutaneous tissue that is easily dissected in a surgical plane guarantees the viability of the flap, facilitating easy rotation on its axis without the need to release the pedicle to repair the margins in a second surgical procedure, as is the case with the fasciocutaneous flap2, maintaining low morbidity and satisfactory results without functional sequelae1,6,8.
The reverse sural flap of the neurocutaneous pedicle, initially described by Masquelet et al. (1994), is one of the most common options2 for treating injuries such as those reported in this case. However, this surgical approach is criticized because of the loss of cutaneous sensitivity and unsightly scarring of the donor area2.
Perforating flaps have also been gaining prominence in recent years. This technique was first described by Donski & Fogdestam (1983)5 but has disadvantages, including the considerable variability in the diameter and position of the perforating vessels.
The use of microsurgical reconstructions, such as the free myocutaneous flap of the latissimus dorsi, among other options that have emerged in the past few years as surgical alternatives for treating injuries in critical areas,2,3 is usually reserved for larger injuries and requires good hospital infrastructure and highly trained staff.
Some options commonly used for treating complex injuries of the lower limbs have been described in a literature review published in the Brazilian Journal of Plastic Surgery in January 201710. However, the flap used in the present study was not mentioned in that review.
Considering data from previous studies and this study, the use of the reverse sural flap of the fasciosubcutaneous pedicle or reverse adipofascial flap has a good prognosis. The use of these flaps was effective and safe, had excellent esthetic and functional results, and did not cause relapses during the evaluation period. Therefore, these flaps deserve more attention from plastic surgeons because of their high clinical potential, especially compared with other techniques used routinely.
CONCLUSION
The use of the reverse sural flap of the fasciosubcutaneous pedicle concomitantly with total skin grafting was found to be a good option with a satisfactory result for the surgical treatment of a complex injury due to Achilles tendon rupture in the lower third of the leg.
COLLABORATIONS
|
DNS |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
MR |
Final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments. |
|
AABMR |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents. |
|
ICP |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
REFERENCES
1. Braga-Silva J, Martins PDE, Román JA, Gehlen D. Utilização do Retalho Adipofascial Reverso nas Perdas de Substância Cutânea do Terço Distal da Perna e Pé. Rev Bras Cir Plást. 2005;20(3):182-6.
2. Garcia AMC. Retalho sural reverso para reconstrução distal da perna, tornozelo, calcanhar e do pé. Rev Bras Cir Plást. 2009;24(1):96-103.
3. Weber ES, Franciosi LFN, Mueller SF, Dalponte M, Heurich NR, Gonçalves SCS. Retalho sural para reconstrução do pé. ACM Arq Catarin Med. 2007;36(Supl. 1):1-4.
4. Belém LFMM, Lima JCSA, Ferreira FPM, Ferreira EM, Penna FV, Alves MB. Retalho sural de fluxo reverso em ilha. Rev Soc Bras Cir Plást. 2007;22(4):195-201.
5. Donski PK, Fogdestam I. Distally based fasciocutaneous flap from the sural region. A preliminary report. Scand J Plast Reconstr Surg. 1983;17(3):191-6. PMID: 6673085
6. Vendramin FS. Retalho sural de fluxo reverso: 10 anos de experiência clínica e modificações. Rev Bras Cir Plást. 2012;27(2):309-15. DOI: http://dx.doi.org/10.1590/S1983-51752012000200023
7. Gumener R, Zbrodowski A, Montandon D. The reversed fasciosubcutaneous flap in the leg. Plast Reconstr Surg. 1991;88(6):1034-41. DOI: http://dx.doi.org/10.1097/00006534-199112000-00013
8. Franco T, Couto P, Gonçalves LFF, Franco D, Silva CC. Tratamento das exposições ósseas e tendinosas no terço distal da perna e no pé utilizando retalho fasciossubcutâneo reverso de panturrilha. Rev Bras Ortop. 1996;31(3):247-52.
9. Kneser U, Bach AD, Polykandriotis E, Kopp J, Horch RE. Delayed reverse sural flap for staged reconstruction of the foot and lower leg. Plast Reconstr Surg. 2005;116(7):1910-7. DOI: http://dx.doi.org/10.1097/01.prs.0000189204.71906.c2
10. Anlicoara R, Barbosa FAMA, Sá JZ, Braga ACCR, Sá GT. Reconstrução de feridas complexas de membros inferiores com retalhos fasciocutâneos reversos. Rev Bras Cir Plást. 2017;32(1):116-22.
1. Universidade Federal de Mato Grosso do Sul,
Campo Grande, MS, Brazil.
2. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
Corresponding author: Daniel Nunes e Silva, Av. Alto Porã, nº 51 - Chácara Cachoeira, Campo Grande, MS, Brazil. Zip Code 79040-045. E-mail: dermatoeplastica@gmail.com
Article received: February 4, 2018.
Article accepted: June 22, 2018.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter