

Original Article - Year 2018 - Volume 33 -
Epidemiological analysis over 2 years at the Burn Unit of the Urgency Hospital Governor Otávio Lage de Siqueira, Goiânia, Brazil
Análise epidemiológica de 2 anos na Unidade de Queimados do Hospital de Urgências Governador Otávio Lage de Siqueira, Goiânia, Brasil
ABSTRACT
Introduction: Burns are a type of injury that is among the
leading causes of mortality. The use of epidemiology helps in
providing subsidies for evaluation and organization of treatment
and prevention, aiming at the improvement of public health. The
objective is to describe the epidemiological profile of the patients
treated at the Queimados Nelson Picollo unit of the Governador
Otávio Lages de Siqueira Emergency Hospital (HUGOL).
Method: This study analyzed the epidemiological profile of
patients, aged more than 12 years, treated by plastic surgery
at the burn treatment unit, Nelson Picollo, from July 2015 to
June 2017. The patients who were not admitted to the burn
unit were excluded from the study. Data were collected from
the MVSoul R. program.
Results: A total of 375 patients visited
the hospital; of these, 50% of the patients needed intensive care
unit treatments. The mean duration of hospital stay was 23.08
days. The majority of the patients were males, with a mean age
of 39.17 years, and the main etiological agents were inflammable
liquids, mainly alcohol and gasoline. The mean burned body
surface area was 24.67%. A total of 1490 surgical interventions
were performed, with an average of 3.97 surgeries per patient.
Forty patients died; of these, 29 had airway burns. The total
number of patients with airway burns was 73.
Conclusion:
This study provides a profile of burns and hospitalizations
in the HUGOL burns unit, which corresponds with those
from other centers specialized for this type of treatment.
Keywords: Burns; Burn units; Transplants; Surgical flaps; Epidemiology
RESUMO
Introdução: Queimadura é um tipo de lesão que está entre as principais causas de
mortalidade. A utilização da epidemiologia ajuda no fornecimento de
subsídios para avaliação e organização de tratamento e prevenção, visando à
melhora da saúde pública. O objetivo é descrever o perfil epidemiológico dos
pacientes atendidos no Hospital de Urgências Governador Otávio Lages de
Siqueira (HUGOL) na unidade de Queimados Nelson Picollo.
Método: Este estudo analisou o perfil epidemiológico dos pacientes atendidos pela
equipe de cirurgia plástica da unidade de tratamento de queimados Nelson
Picollo, no período de julho 2015 até junho 2017, com idade superior a 12
anos. Critérios de exclusão: pacientes que não foram internados na unidade
de queimados. Os dados foram colhidos do programa MVSoul R.
Resultados: O total de atendimentos foi de 375 pacientes, dos quais 50% necessitaram de
tratamentos unidade de terapia intensiva. O tempo médio de internação foi de
23,08 dias. A maioria do sexo masculino, com média de idade de 39,17 anos,
com agente etiológico principal as chamas por álcool + gasolina. A média de
superfície corporal queimada foi de 24,67%. Foram realizados 1490
intervenções cirúrgicas, média de 3,97 cirurgias por paciente. O total de
óbitos foi de 40 pacientes, dos quais 29 apresentaram queimadura de via
aérea. O total de pacientes com queimadura de via aérea foi de 73 casos.
Conclusão: Este estudo demonstrou um perfil de queimaduras e internações na unidade de
Queimados do HUGOL compatível com outros centros especializados neste tipo
de tratamento.
Palavras-chave: Queimaduras; Unidades de queimados; Transplantes; Retalhos cirúrgicos; Epidemiologia
INTRODUCTION
Burns constitute injury of the organic tissue caused by external agent. Burns may result from trauma caused by heat, chemicals, electricity, friction, or radiation, leading to partial or total destruction of the skin and adjacent tissues1. The severity and prognosis of burns are directly related to the burned body surface area and the depth of the burn, while the factors that indirectly influence the prognosis are the anatomical location of the burn, the age of the patient, the etiological agent, and preexisting diseases and associated lesions. These factors are important indicators of the need for hospitalization for the treatment of burns2,3.
According to the World Health Organization, burns are the fourth most common type of trauma in the world, after interpersonal violence, falls, and traffic accidents4. The number of people with burns is large, and burns constitute a serious public health problem. It is estimated that six million victims per year seek medical care for some degree of burns worldwide; however, it is difficult to determine the specific distribution of cases for each country due to the scarcity of epidemiological data and national reporting systems.
In some countries, the available data allow us to estimate the annual incidence of burns, for example, the incidence is around 500,000 in the United States of America; 10,000-15,000 hospital admissions per year have been reported in Germany; and 700,000 to 800,000 new cases are reported in India. According to the Brazilian Society of Burns (SBQ), it is estimated that there are approximately 1,000,000 burn injuries per year in Brazil. Of these, about 100,000 require hospital care and 2,500 evolve to death due to burns or the associated complications5.
Burn Treatment Units (BTUs) first appeared in the United States and England in the 1950s to improve and strengthen the specific treatment of burn victims and to improve the epidemiological indices of these treatments. Currently, the US has 137 BTUs located across the country. In Brazil, there are 57 registered BTUs throughout the national territory, as reported by the Brazilian Society of Burns (SBQ).
These units are reference centers for hospitalization and treatment of patients with severe complex second and third degree burns and important comorbidities. They function as multiprofessional treatment centers, with serval professionals that provide care to these patients. In addition to clinical care, these units should function as centers for knowledge-building, training professionals, and disseminating burn data6-8.
The epidemiological pattern of burns varies widely in different parts of the world9. They represent a public health problem in several developing countries, and the lack of public education campaigns is one of the main factors associated with a high incidence of accidental burns10.
Epidemiology is considered the basic science for preventive medicine and a source of information for the formulation of public health policies. Currently, patients who are victims of burns should be evaluated and monitored periodically by interdisciplinary professionals in specialized centers, who have the physical plant, facilities, and adequate equipment to perform the treatment11.
OBJECTIVE
The study involved the evaluation and analysis of the epidemiological profile of patients hospitalized for treatment at the Burn Unit of the Governor Otávio Lage de Siqueira (HUGOL) Emergency Hospital in Goiânia, GO.
METHODS
Data from the electronic medical records of 376 patients who were treated for burns at the HUGOL Emergency Hospital in Goiânia, GO, between July 2015 and June 2017 was collected and analyzed.
Inclusion criteria
Patients, who visited the Emergency and outpatient clinic at HUGOL but were not hospitalized for treatment, patients who were admitted to the Pediatrics unit, either in the ICU or a clinical or surgical ward due to some kind of burns were excluded.
Statistical analysis
During the analysis of the variables of this study, we considered as inclusion criteria: age, gender, etiological agent, burned body surface area, burn depth, body regions affected by burn, debridements, grafts, flaps, infections, evolution to death, burns of inhaled routes, time of hospitalization in intensive care unit of burns and time of hospitalization.
The data was plotted in excel table and analyzed by the SPSS 24 program.
RESULTS
A total of 375 patients were admitted from July 2015 to June 2017; of these, 50% of the patients needed treatment and follow-up in an intensive care unit (Table 1). The average hospitalization duration for these patients in the ICU was 14.73 days.
| Yes | 188 |
| No | 187 |
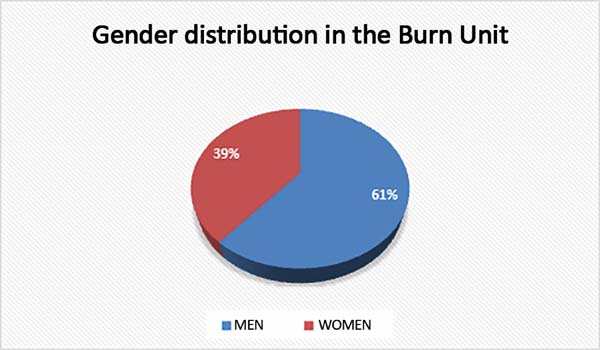
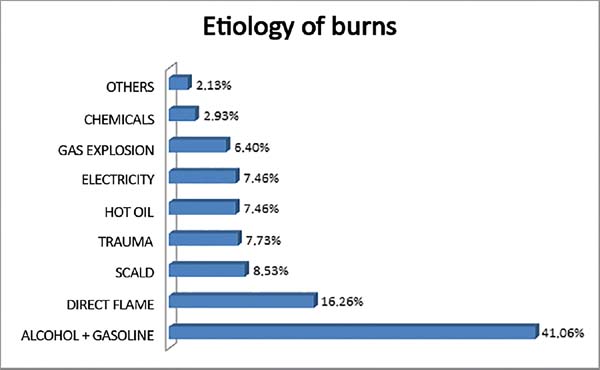
The overall mean duration of hospitalization in the burns unit was 23.08 days. The patients were mostly males (61%) (Figure 1). The mean age of the patients was 39.17 years. The main etiological agent in the patients admitted to the service was alcohol in combination with gasoline (41.06%), followed by direct flame (16.26%), scalding (8.53%), trauma (7.73%), hot oil or (7.46% for each), gas explosion (6.4%), and chemicals (2.93%) (Figure 2).
In cases of chemical burns, sulfuric acid was the major etiological agent, accounting for 37% of the cases (Table 2). The mean SCQ was 24.67%. The 2nd degree burns were the most prevalent type, reported in 51% of the cases, followed by a combination of 2nd and 3rd degree burns, in 47%, while 3rd degree burns were reported in only 2% of the cases (Table 3).
| Cicatricure® | 1 |
| Caustic soda | 4 |
| Sulfuric acid | 2 |
| Acid detergent | 2 |
| Tar | 1 |
| Fig leaf | 1 |
| Total | 11 |
| Second degree | 189 |
| Second + third degree | 178 |
| Third degree | 8 |
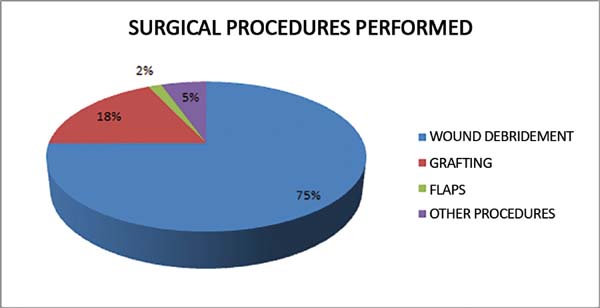
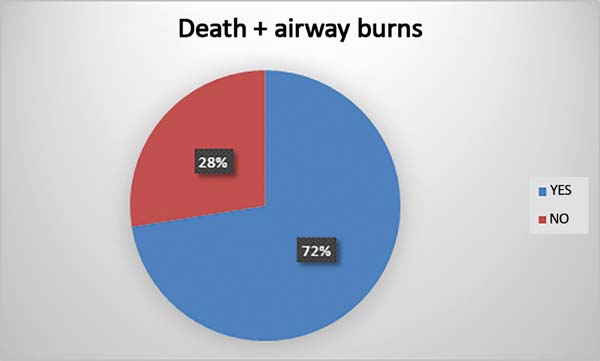
A total of 1490 surgical procedures were performed, with an average of 3.97 surgeries per patient. Of these, 268 were grafting; 24, flap placement; 1117, debridement; and 81, other procedures, among them tracheostomies (Figure 3). Forty patients died; of them, 29 presented airway burns (72.5%; Figure 4). The total number of patients with airway burns was 73.
DISCUSSION
Burns are a serious public health problem in Brazil. Knowledge of epidemiological data is of great importance in supporting programs for the prevention and treatment of burns, and for defining a parallel between national and international experiences. The data obtained in this study were, in general, compatible with those reported in other national and international studies.
In the period studied, we observed a prevalence of accidents in males (61%), corresponding to the national and international epidemiological profile12-16.
The burning agent was the open flame (57.32%), particularly on contact with flammable liquids, mainly alcohol and gasoline (41.06%), followed by heated liquids (15.99%), similar to that data reported by Macedo and Rosa16 and data from other countries13. The use of flammable liquids to light a fire is very common in Brazil, and the use of alcohol in the gel form is an effective method for reducing the incidence of burns by this agent.
The electrical and chemical burns were the least frequent (7.46% and 2.93%, respectively) with a lower burned body surface area, but a greater burn depth; these data correspond with data from the literature review16-20.
The mean burned body surface area was 24.67%, leading to an average hospital stay of 23.08 days. This duration of hospitalization was similar to that described by Macedo and Rosa16 and also to the international statistics21-23. The severity of the patients, such as the depth and area of the burns, and the presence of airway lesion were related.
The mortality rate in this study was 10.66%, higher than that observed by Macedo and Rosa16 and in other Brazilian studies11; being compatible with an increase in the mean age of the patients studied, the depth and area of burns, and the presence of airway injury.
Traditionally, the burned body surface, the severity of the lesion, and the age of the patient were important determinants of the mortality rate in patients with burns. With the advancements in studies on this health impairment, other factors, such as inhalation injury, pre-admission shock, sepsis and thrombocytopenia, became important.
The highest mortality rates are among the older patients, especially those aged more than 60 years. We observed this in our study, since the mean age of the patients in our study was 39.17 years, which is about 30% higher than the average age reported by Gimenes et al.13 from Sorocaba, SP; the mean age of the patients is usually less than 30 years in national and international studies. This may be because patients under 12 years of age, who are usually victims of a hot liquid (scalding) accident, acquire more superficial lesions, with lower mortality rates in this age group.
Another factor that explains this high mortality rate is the high prevalence of inhalation burns, often not mentioned in other studies due to the difficulty in documenting such burns. We observed a higher mortality rate in patients with evidence of airway burns. Of the 40 deaths, 29 had airway burns (72.5%) (Figure 4). The total number of patients with airway burns was 73, that is, 39.72% of the patients suffered burns in various areas and died, which is consistent with the world literature.
Burns remain the worst injury that can suddenly happen to individuals, marking them for the rest of their life. Burns are responsible for significant morbidity and high mortality rates worldwide, despite advances in the available treatments24.
The study provided a profile of burn injuries and hospitalizations in the Burns unit of HUGOL; this profile corresponds with those from other specialized centers for this type of treatment.
This study contributes to the evidence that epidemiological studies are indispensable tools for acquiring knowledge about the population to be treated, thus, enabling the development of strategies for the prevention of burns and for the progressive decrease of its prevalence. The study also proposes the importance of continuously educating the population to prevent avoidable accidents.
The negligent use of inflammable products also accounts for a large number of these accidents; the incidence of such accidents may decrease if effective social awareness measures are implemented.
COLLABORATIONS
|
FCFA |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
BCOC |
Analysis and/or interpretation of data; conception and design of the study; writing the manuscript or critical review of its contents. |
|
JFM |
Statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
|
WJVJ |
Statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
|
GMDR |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; writing the manuscript or critical review of its contents. |
REFERENCES
1. Mendes CA, Sá DM, Padovese SM, Cruvinel SS. Estudo epidemiológico de queimaduras atendidas nas Unidades de Atendimento Integrado de Uberlândia-MG entre 2000 a 2005. Rev Bras Queimaduras. 2009;8(1):18-22.
2. Serra MCVF, Gomes DR, Crisóstomo MR, Serra AS. Cálculo da área queimada e indicadores para internação hospitalar. In: Maciel E, Serra MC, eds. Tratado de queimaduras. São Paulo: Atheneu; 2004. p. 43-9.
3. Leão CEG, Andrade ES, Fabrini DS, Oliveira RA, Machado GLB, Gontijo LC. Epidemiologia das queimaduras no estado de Minas Gerais. Rev Bras Cir Plást. 2011;26(4):573-7.
4. World Health Organization (WHO). The Global Burden of Disease: 2004 Update. Geneva: World Health Organization; 2008 [citado 2018 Maio 23]. Disponível em: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
5. Gomes DR, Serra MC, Guimarães LM. Condutas na Internação. In: Gomes DR, Serra MC, Guimarães LM, Macieira Júnior L, eds. Condutas atuais em queimaduras. Rio de Janeiro: Revinter; 2001.
6. Al-Mousawi AM, Mecott-Rivera GA, Jeschke MG, Herndon DN. Burn teams and burn centers: the importance of a comprehensive team approach to burn care. Clin Plast Surg. 2009;36(4):547-54. DOI: http://dx.doi.org/10.1016/j.cps.2009.05.015 DOI: http://dx.doi.org/10.1016/j.cps.2009.05.015
7. http://www.ameriburn.org/BCRDPublic.pdf http://dx.doi.org/10.1353/abr.2014.0064
8. Sociedade Brasileira de Queimaduras (SBQ). Queimaduras [Internet]. Goiânia [acesso 2013 Jun 16]. Disponível em: http://sbqueimaduras.org.br/queimaduras-conceito-e-causas
9. Cruz BF, Cordovil PBL, Batista KNM. Perfil epidemiológico de pacientes que sofreram queimaduras no Brasil: revisão de literatura. Rev Bras Queimaduras. 2012;11(4):246-50.
10. Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004;329(7463):447-9. PMID: 15321905 DOI: http://dx.doi.org/10.1136/bmj.329.7463.447
11. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. Rev Bras Queimaduras. 2010;9(3):82-8.
12. Souza AA, Mattar CA, Almeida PCC, Faiwichow L, Fernandes FS, Neto ECA, et al. Perfil epidemiológico dos pacientes internados na Unidade de Queimaduras do Hospital do Servidor Público Estadual de São Paulo. Rev Bras Queimaduras. 2009;8(3):87-90.
13. Gimenes GA, Alferes FCBA, Dorsa PP, Barros ACP, Gonella HA. Estudo epidemiológico de pacientes internados no Centro de Tratamento de Queimados do Conjunto Hospitalar de Sorocaba. Rev Bras Queimaduras. 2009;8(1):14-7.
14. Asuquo ME, Ekpo R, Ngim O, Agbor C. A prospective study of burn trauma in adults at the university of calabar teaching hospital, calabar (South eastern Nigeria). Eplasty. 2008;8:e36.
15. Montes SF, Barbosa MH, Sousa Neto AL. Aspectos clínicos e epidemiológicos de pacientes queimados internados em um Hospital de Ensino. Rev Esc Enferm USP. 2011;45(2):369-73. DOI: http://dx.doi.org/10.1590/S0080-62342011000200010
16. Macedo JLS, Rosa SC. Estudo epidemiológico dos pacientes internados na Unidade de Queimados: Hospital Regional da Asa Norte, Brasília, 1992-1997. Brasília Med 2000;37(3/4):87-92.
17. Adesunkanmi K, Oyelami OA. The pattern and outcome of burn injuries at Wesley Guild Hospital, Ilesha, Nigeria: a review of 156 cases. J Trop Med Hyg. 1994;97(2):108-12.
18. Costa DM, Lemos ATO, Lamounier JA, Cruvinel MGC, Pereira MVC. Estudo retrospectivo de queimaduras na infância e adolescência. Rev Méd Minas Gerais 1994;4(2):102-4.
19. Haberal M, Uçar N, Bilgin N. Epidemiological servey of burns trated in Ankara, Turkey and desirable burn-prevention strategies. Burns. 1995;21(8):601-6. DOI: http://dx.doi.org/10.1016/0305-4179(95)00044-C
20. Milo Y, Robinpour M, Glicksman A, Tamir G, Burvin R, Hauben DJ. Epidemiology of burns in the Tel Aviv area. Burns. 1993;19(4):352-7. PMID: 8357485 DOI: http://dx.doi.org/10.1016/0305-4179(93)90127-T
21. Brusselares N, Juhász I, Erdei I, Monstrey S, Blot S. Evaluation of mortality following severe burns injury in Hungary: external validation of a prediction model developed on Belgian burn data. Burns. 2009;35(7):1009-14. DOI: http://dx.doi.org/10.1016/j.burns.2008.12.017
22. Burton KR, Sharma VK, Harrop R, Lindsay R. A population-based study of the epidemiology of acute adult burn injuries in the Calgary Health Region and factors associated with mortality and hospital length of stay from 1995 to 2004. Burns. 2009;35(4):572-9. DOI: http://dx.doi.org/10.1016/j.burns.2008.10.003
23. Coutinho BBA, Balbuena MB, Anbar RA, Anbar RA, Almeida KG, Almeida PYNG. Perfil epidemiológico de pacientes internados na enfermaria de queimados da Associação Beneficente de Campo Grande Santa Casa/MS. Rev Bras Cir Plást. 2010;25(4):600-3.
24. Machado THS, Lobo JA, Pimentel PCM, Serra MCVF. Estudo epidemiológico das crianças queimadas de 0-15 anos atendidas no Hospital Geral do Andaraí, durante o período de 1997 a 2007. Rev Bras Queimaduras. 2009;8(1):3-8.
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
2. Hospital de Urgências Governador Otávio Lage de
Siqueira, Goiânia, GO, Brazil.
Corresponding author: Fabiano Calixto Fortes de Arruda, Rua T 50 n, 540 - Setor Bueno - Goiânia, Goiás, Brazil. Zip Code 74215-200. E-mail: arrudafabiano@hotmail.com
Article received: December 14, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter