

Original Article - Year 2018 - Volume 33 -
Alar cartilage flap for projection of the nasal tip
Retalho de cartilagem alar para projeção da ponta nasal
ABSTRACT
Introduction: The nasal tip is a frequent object of study
by surgeons, since it is a common reason for pre- and
postoperative complaints. Thus, the tip should be thoroughly
evaluated to determine the best technique to be used. The
objective is to demonstrate an original alar cartilage flap
technique for projection of the nasal tip, performed alone
or in combination with other procedures for the same
purpose.
Method: A retrospective cross-sectional study of
22 patients submitted to open rhinoplasty with use of the
alar flap to project the nasal tip.
Results: A total of 22 open
rhinoplasties were performed on primary bulbous, fatty,
and under-projected tips. Among the patients in the study,
90% were black and 2% were white; 72.7% reported a high
degree of satisfaction with the operation, 18.1% considered
the result very good, and 9.2% considered the result
acceptable. There were no complications/reoperations.
Conclusion: The alar cartilage flap for projection of the nasal
tip is simple to perform and can be considered an excellent
supplemental method for use in treatment of the black nose.
Keywords: Rhinoplasty; Projection; Nasal cartilage; Nose; Surgical flaps
RESUMO
Introduction: The nasal tip is a frequent object of study by surgeons, since it is a common
reason for pre- and postoperative complaints. Thus, the tip should be
thoroughly evaluated to determine the best technique to be used. The
objective is to demonstrate an original alar cartilage flap technique for
projection of the nasal tip, performed alone or in combination with other
procedures for the same purpose.
Method: A retrospective cross-sectional study of 22 patients submitted to open
rhinoplasty with use of the alar flap to project the nasal tip.
Results: A total of 22 open rhinoplasties were performed on primary bulbous, fatty,
and under-projected tips. Among the patients in the study, 90% were black
and 2% were white; 72.7% reported a high degree of satisfaction with the
operation, 18.1% considered the result very good, and 9.2% considered the
result acceptable. There were no complications/reoperations.
Conclusion: The alar cartilage flap for projection of the nasal tip is simple to perform
and can be considered an excellent supplemental method for use in treatment
of the black nose.
Palavras-chave: Rinoplastia; Projeção; Cartilagens nasais; Nariz; Retalhos cirúrgicos
INTRODUCTION
In the past two decades, the preservation of function as well as the final esthetic result have become of primary importance in rhinoplasty. As a result, there has been a greater tendency to use open techniques that provide greater exposure of the anatomical elements, leading to new techniques and surgical strategies.
The origin of the pioneering techniques for nasal tip projection in rhinoplasty share a basic principle: sacrificing the integrity of the lateral cartilage to increase the medial crus and gain nasal projection. In the medium and long term, these techniques showed loss of the support mechanism of the nasal tip and resulted in undesirable postoperative effects, including complications such as clamping, asymmetry, and drooping of the nasal tip, in addition to creating an unattractive and stigmatized nasal appearance1-3.
Various reports (Beekhuis & Colton4,5, McCollough6,7, Petroff et al.8, Adams et al.9) reported the difficulties in achieving satisfactory nasal projection using only these methods. Projection may be difficult to achieve, especially in the black nose, in which projection of the tip is a difficult task due to the thick skin and hypotrophic skeleton. Thus, remodeling these nasal tips becomes a major challenge, solved in large part with cartilaginous grafts in the dome and columella.
This article presents another means for designing the nasal tip, using it as an isolated complementary procedure to other techniques that alone do not reach fully satisfactory results.
OBJECTIVE
To demonstrate a nasal tip projection technique using alar cartilage flaps, performed alone or in combination with other procedures with the same purpose.
METHOD
This was a retrospective cross-sectional study of the charts of patients submitted to rhinoplasty between March 2015 and April 2017, in which the nasal tip projection technique was applied using alveolar cartilage flaps at the Department of Plastic Surgery of Daher Lago Sul Hospital, in Brasília, DF.
Patients had noses with bulbous tips and thick skin, and were difficult to project using the usual techniques.
All patients provided signed informed consent authorizing use of records, information on treatment, and photographs for scientific purposes.
All procedures were performed by the same plastic surgeon, the senior author of this work.
The postoperative follow-up period was at least 1 year (ranging from 12 to 24 months).
The results were evaluated by a Full Member of the Brazilian Society of Plastic Surgery who was not part of the surgical team, using comparative analysis of preoperative and postoperative photographs (at least 6 months after surgery).
The present study followed the principles of the Declaration of Helsinki.
Description of the surgical technique
The alar cartilage flap for projection of the nasal tip uses an innovative approach that differs from the usual procedures for nasal tip projection described in the literature.
The development of the new technique was based on a fortuitous event in which there was difficulty in projecting the nasal tip, as well as other successive cases.
The flap is made with the use of cranial bands of alar cartilage, after release of the lateral portions, and the pedicled medial portion is maintained. The width of the base compared to the length of the dorsum determines the size of the flap and the projection to be created.
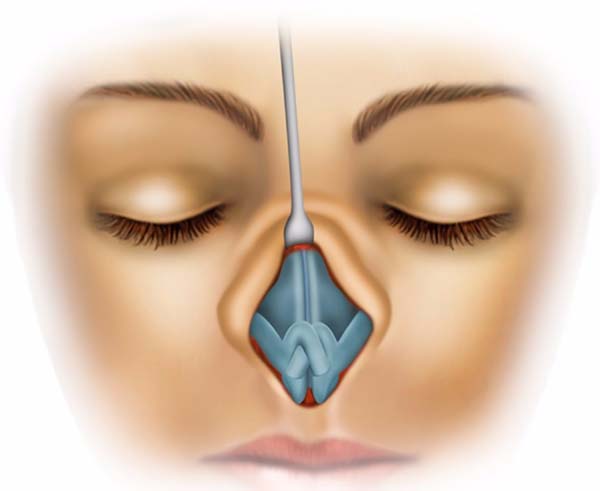
For better explanation of the technique, 5 steps are described:
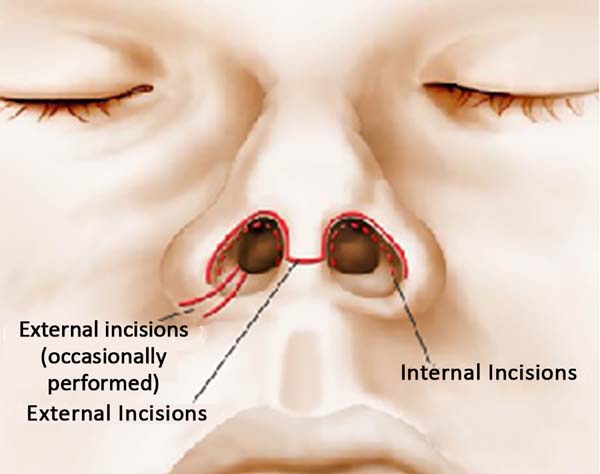
Step 1 - Incision and detachment
Open rhinoplasty technique, with columella incision at its narrowest point (Figures 1 and 2). Figures 1 and 2 illustrate the exposure of the alar cartilages.
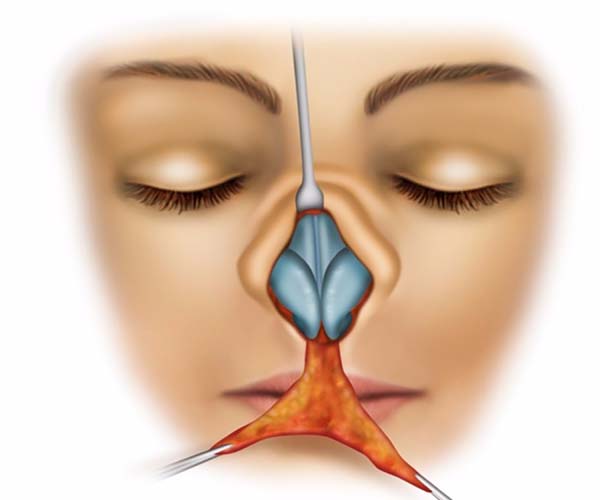
Step 2 - Defatting of the nasal tip
The dissection of the skin leaves the adipose tissue in a deep plane adherent to the superficial musculoaponeurotic system of the nasal tip and perichondrium. Defatting of the cartilage is thorough to avoid trauma (Figures 3 and 4).
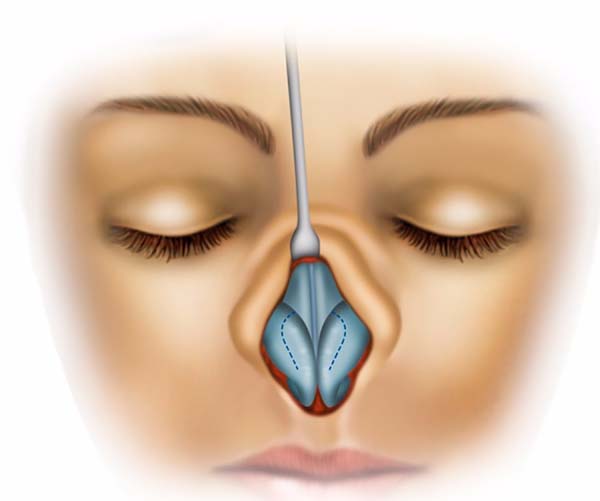
Step 3 - Design of cranial portions of the alar cartilage
After suture fixation for the best definition of the dome, design of the cranial portions of the alar cartilage was performed, prior to resection to construct the flaps (Figures 5 and 6).
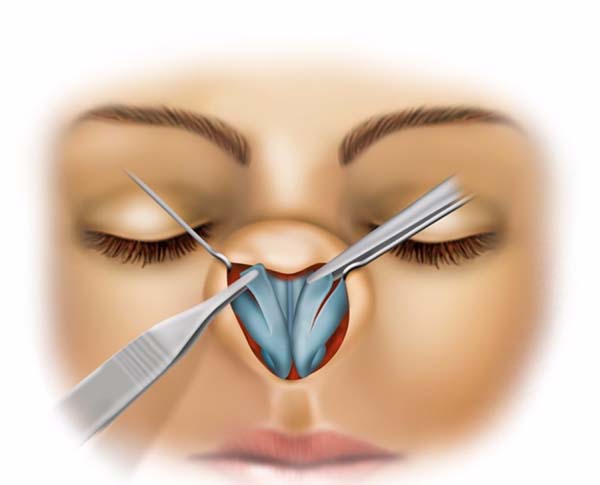
Step 4 - Release and resection of cranial portions of alar cartilage
Incisions were performed on the flaps in the cranial portions of the alar cartilage and pedicled at the dome, as shown in Figures 7 and 8.
Step 5 - Rotation of the cranial portion of the alar cartilage flap and final construction of the new nasal tip projection
Points A and B are rotated toward point C, and cross each other to form the main scaffold of the new nasal tip (Figures 9 and 10), while maintaining the dome of the pedicled ala. Simple sutures with nylon 6-0 were used for coaptation of the alar cartilage on the dome, and construction of the new nasal tip was then completed, as shown in Figures 9 and 10.
RESULTS
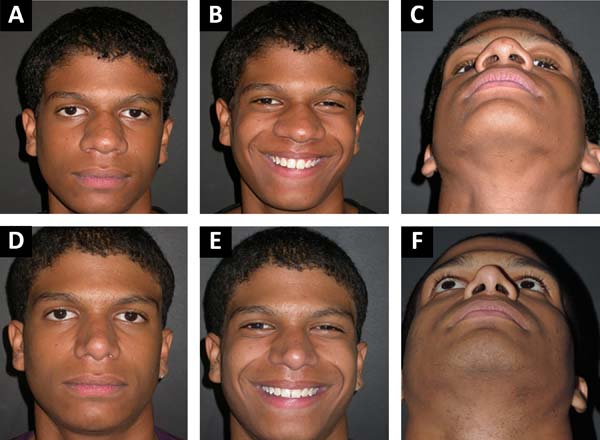
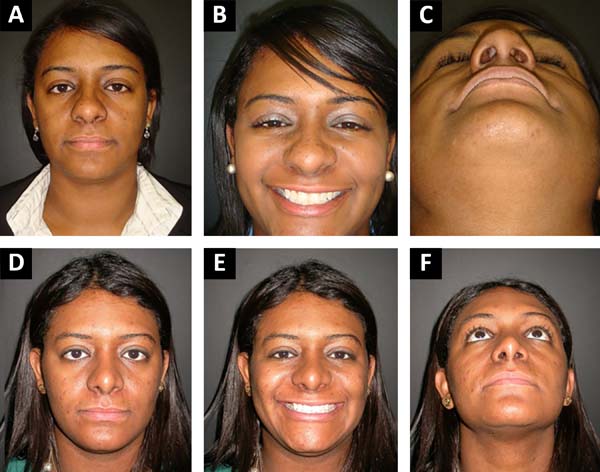
Twenty-two black patients with bulbous noses were submitted to rhinoplasty using the wing cartilage flap technique for projection of the nasal tip; all were primary rhinoplasties.
The mean age was 31.04 years and the follow-up ranged from 16 to 24 months.
The demographic data of the study patients and their characteristics are presented in Table 1.
| Number of Patients | 22 |
| Average age | 31.04 ± 1.22 |
| Sex | |
| Female | 10 |
| Male | 12 |
| Ethnicity | |
| White | 2 |
| Black | 20 |
| Type of rhinoplasty | |
| Primary | 22 |
| Secondary | 0 |
| Results | |
| Excellent | 16 |
| Good | 4 |
| Fair | 2 |
| Complications | None |
Figures 1 to 10 illustrate the surgical steps and the results of the original alar cartilage flap technique for projection of the nasal tip.
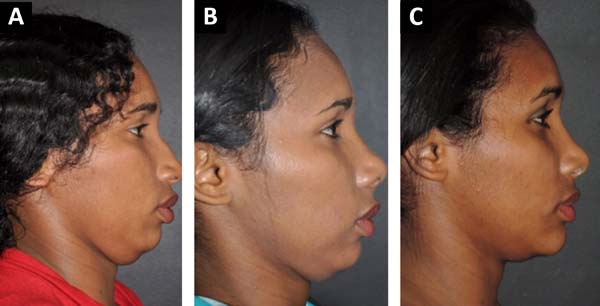
Figures 11 to 16 show examples of patients with typical black noses, with extended ala and bulbous nasal tip in the preoperative period and at one and two years of postoperative follow-up. The postoperative results show noses with narrower bases and tapered and raised nasal tips, and without a bulbous appearance. In all illustrated cases, the alar cartilage flap technique for projection of the nasal tip was used as an isolated technique or was combined with other techniques.
DISCUSSION
The literature is still somewhat controversial regarding the results of refinement of the nasal tip in rhinoplasty, with the main limitation being excessive loss of nasal projection over time. Thus, the evaluation of projection of the nasal tip is a critical point and a subject of discussion in rhinoplasty. Different techniques and materials are used for better esthetic results and maintenance of the nasal tip10,11.
The increased use of cartilage excision techniques in esthetic rhinoplasty has often resulted in rupture of the nasal tip components, promoting inconsistent and undesirable results in the medium and long term, with unsightly retraction and compromised function11.
Beekhuis & Colton4,5 believed that the strength of the alar cartilage and the septal angle are the factors that most affect the projection of the tip. McCollough6,7 emphasized that the ligament structures of the nasal tip are key components of the “tripod.” Petroff et al.8 recognized that the medial cartilage and its relationship with the septum are important for sustaining the tip. Adams et al.9 analyzed various support components for projection of the nasal tip in rhinoplasty and realized that greater loss in projection was observed in open approaches than with closed rhinoplasty.
Conservative surgery with minimal or no resection is preferred, but repositioning with precise sutures coupled with understanding of the dynamics when used alone or in combination with cartilage grafts is acceptable4-9.
With loss of projection of the nasal tip, changes in rotation and length of the nose can occur secondary to the loss of adequate support of the nasal cartilage. Irregularities of the nasal tip, the dorsal contour, and alar retraction are often caused by the loss of cartilage dynamics7,11.
The septal cartilage is considered a good graft donor area for the correction of nasal deformities in non-primary rhinoplasty, for use in the preparation of dorsal and projection grafts, struts, tip definition, and nasal length. Auricular or costal cartilage may be alternative donors. However, even with the availability of these resources, this new technique can be used as a single point projection procedure or in combination with other procedures that alone did not achieve complete projection as planned or desired11.
This original nasal tip projection technique using an alar cartilage flap has the advantages of being a local flap, absence of observed complications, and good maintenance of long-term shape and projection.
The simplicity of the technique still permits surgical flexibility and creativity. While the flaps of the alar cartilage are being prepared, the surgeon can rotate and fix them in the contralateral or ipsilateral cartilage. The nasal tip is structured after the cartilaginous loops are formed with separate sutures, according to individual requirements in each case.
This report presents a simple, easy-to-execute, and reliable technique that produces a natural nasal appearance with maintenance of long-term tip projection. It should be understood that this method is proposed as an additional resource for projection of the tip when the desired result is not obtained using the usual dome repositioning methods or cartilage grafts, as is commonly observed in the black nose12,13.
CONCLUSION
This original alar cartilage flap technique for projection of the nasal tip has been very effective. The employment of this technique has provided satisfactory results for projection of the nasal tip.
The technique is simple to execute, without significant complications, and is a viable option for nasal tip projection in selected patients, especially in combination with other procedures. The technique is of great value in surgery on the bulbous or black nose.
COLLABORATIONS
|
JCD |
Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
MCAG |
Analysis and/or interpretation of data; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
LGM |
Analysis and/or interpretation of data; completion of surgeries and/or experiments. |
|
LMCD |
Analysis and/or interpretation of data; completion of surgeries and/or experiments. |
|
IRJ |
Analysis and/or interpretation of data. |
|
GCS |
Analysis and/or interpretation of data. |
|
LDPB |
Analysis and/or interpretation of data; completion of surgeries and/or experiments. |
|
CADCF |
Analysis and/or interpretation of data; completion of surgeries and/or experiments. |
REFERENCES
1. Lee MR. Discussion: Anatomical Study of the Medial Crura and the Effect on Nasal Tip Projection in Open Rhinoplasty. Plast Reconstr Surg. 2013;132(4):794-5. PMID: 24076671 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182a01550
2. Han SK, Lee DG, Kim JB, Kim WK. An anatomic study of nasal tip supporting structures. Ann Plast Surg. 2004;52(2):134-9. PMID: 14745261 DOI: http://dx.doi.org/10.1097/01.sap.0000095439.98488.e6
3. Janeke JB, Wright WK. Studies on the support of the nasal tip. Arch Otolaryngol. 1971;93(5):458-64. DOI: http://dx.doi.org/10.1001/archotol.1971.00770060704004
4. Beekhuis GJ, Colton JJ. Nasal tip support. Arch Otolaryngol Head Neck Surg. 1986;112(7):726-8. PMID: 3707733 DOI: http://dx.doi.org/10.1001/archotol.1986.03780070038008
5. Colton JJ, Beekhuis GJ. Rhinoplasty analysis. Otolaryngol Clin North Am. 1987;20(4):675-98.
6. McCollough EG, English JL. A new twist in nasal tip surgery. An alternative to the Goldman tip for the wide or bulbous lobule. Arch Otolaryngol. 1985;111(8):524-9. PMID: 3896210 DOI: http://dx.doi.org/10.1001/archotol.1985.00800100072010
7. McCollough EG, Mangat D. Systematic approach to correction of the nasal tip in rhinoplasty. Arch Otolaryngol. 1981;107(1):12-6. PMID: 7469873 DOI: http://dx.doi.org/10.1001/archotol.1981.00790370014002
8. Petroff MA, McCollough EG, Hom D, Anderson JR. Nasal tip projection. Quantitative changes following rhinoplasty. Arch Otolaryngol Head Neck Surg. 1991;117(7):783-8. PMID: 1863446 DOI: http://dx.doi.org/10.1001/archotol.1991.01870190095020
9. Adams WP Jr, Rohrich RJ, Hollier LH, Minoli J, Thornton LK, Gyimesi I. Anatomic basis and clinical implications for nasal tip support in open versus closed rhinoplasty. Plast Reconstr Surg. 1999;103(1):255-61. DOI: http://dx.doi.org/10.1097/00006534-199901000-00040
10. Joseph J. Nasoplastik und Sonstige Gesichts Plastik Nebst Mammoplastik. Leipzig: Kurt Kabitzsch; 1931.
11. Daniel RK. The nasal tip: anatomy and aesthetics. Plast Reconstr Surg. 1992;89(2):216-24. DOI: http://dx.doi.org/10.1097/00006534-199202000-00002
12. Rohrich RJ, Bolden K. Ethnic rhinoplasty. Clin Plast Surg. 2010;37(2):353-70. DOI: http://dx.doi.org/10.1016/j.cps.2009.11.006
13. Momoh AO, Hatef DA, Griffin A, Brissett AE. Rhinoplasty: the african american patient. Semin Plast Surg. 2009;23(3):223-31. DOI: http://dx.doi.org/10.1055/s-0029-1224802
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
2. Hospital Daher Lago Sul, Brasília, DF,
Brazil.
Corresponding author: José Carlos Daher, SHIS QI7 Conjunto F - Lago Sul - Brasília, DF, Brazil. Zip Code 71615-570. E-mail: daher@hospitaldaher.com.br
Article received: December 18, 2016.
Article accepted: May 17, 2018.
Conflicts of interest: none.


























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter