

Articles - Year 1999 - Volume 14 -
Gluteal V-Y Flaps for Restoration of Sacral, Ischial and Trochanteric Ulcers without Transection or Sacrifice of the Gluteus Maximus Muscle
Retalhos Glúteos em V-Y para Reparação de Úlceras Sacras, Isquiáticas e Trocantéricas, sem Secção ou Sacrifício do Músculo Glúteo Máximo
ABSTRACT
The work aimed at presenting the employment of V-Y gluteal flaps without muscle de-insertion or transection to cover sacral, ischial and trochanteric ulcers. After ulcer excision, flaps were planned and dissected with incisions that comprehended skin, adipose layer, and fascia without reaching gluteus maximus muscle (GMM), and forming a fasciocutaneous block. Flaps had their nearest ends to the lesions detached at the plane between fascia and muscle in order to facilitate later advance and closing of bloody area. Twenty-two patients were operated, totalizing 24 ulcers, from which 12 were sacral, 7 ischial and 5 trochanteric; 26 flaps were employed, all of them showing to be feasible with no suffiring or significant complication. Lower surgical time, less bleeding, maintenance of GMM integrity so that it can be used for an eventual reintervention, as well as its function maintenance, which represents a great benefit as to its employment in patients without permanent neurological lesion, showed that the method is a advantageous alternative to complex injury restorations at the sites mentioned.
Keywords: Gluteal flaps; V-Y flaps; stress ulcers.
RESUMO
O trabalho objetivou apresentar o emprego de retalhos glúteos em V-Y, sem desinserção ou secção muscular, para cobertura de úlceras sacras, isquiáticas e trocantéricas. Após excisão das úlceras, os retalhos eram planejados e dissecados com incisões que abrangiam pele, panículo adiposo e fáscia, sem atingir o músculo glúteo máximo (MGM), constituindo um bloco fasciocutâneo. Os retalhos tiveram suas extremidades mais próximas às lesões descoladas no plano entre a fáscia e o músculo para facilitar o posterior avançamento e fechamento da área cruenta. Foram operados 22 pacientes, num total de 24 úlceras, das quais 12 eram sacras, 7 isquiáticas e 5 trocantéricas; sendo empregados 26 retalhos, com todos mostrando-se viáveis, sem qualquer sofrimento ou complicação significativa. Menor tempo cirúrgico, menor sangramento, manutenção da integridade do MGM, permitindo sua utilização em eventual reintervenção, assim como a permanência de sua função, o que representa enorme benefício quando imaginamos seu emprego em pacientes sem lesão neurológica permanente, demonstraram ser o método uma vantajosa alternativa na reparação de ferimentos complexos nas regiões mencionadas.
Palavras-chave: Retalhos glúteos; retalhos em V-Y; úlceras de pressão.
The plastic surgeon's work at a general hospital frequently makes him face the commonly dramatic picture of stress ulcers. The ill-fated eschars gain more complexity in the proportion they routinely occur in plurienjured, physically and emotionally depleted patients and not rare, let at their own fate. As worldwidely agreed upon, the multidisciplinary character(1, 2) of such patients' treatment is indispensable factor for them to be submitted to their lesion's restoration when they attain proper clinical and laboratory conditions.
Surgical treatment of stress ulcers was first reported by Davis in 1938, who used local flaps, but his study did not include paraplegic individuals. The World War II, that generated millions of victims, including those people that evolved to para or tetraplegia, constitutes the milestone from which a number of techniques developed aiming at treating ulcers, then called bedsores(1, 3). No doubt, as of the 70's, with Ger(4)introducing the principle of muscle transposition for the treatment of lower limb injuries and, more recently, with the advent of myocutaneous flaps(5, 6), the spectrum and safety of surgical alternatives employed were exceedingly enlarged , not only for the treatment of stress ulcers but also for the losses of substances coming from other sources and from the most diverse topographies.
This work aims at presenting the feasibility of using the V-Y gluteal flaps not only for the routionly performed closing of sacral ulcers, but also to ischial and trochanteric ulcers. The usual muscle-cutaneous elasticity of that region(7) and the GMM's reach vascular network(8) offer proper safery for planning and mobilization of these flaps that, as a major technical detail, are applied as fasciocutaneous units. With this approach, the muscle integrity, with no partial section or de-insertion, is maintained, preserving it for possible reoperations as unfortunately relapses are common when referring to stress ulcers. Still as an attractive to the method we have the muscle function maintenance, which gains an important meaning when indicated for healthy patients from the neurimotor point of view.
SURGICAL ANATOMY
Located at surface, the GMM shows itself wide, thick and with quadrilateral shape, characterized by gluteal prominence. It is originated at the ileum posterior gluteal line, sacral and coccyx posterior face, sacrotuberal ligament and aponeurosis that covers the middle gluteal muscle; its fibers go down and out, inserting into the ileum-tibial tract and femur greater trochanter(8). GMM's vascular supply has three sources: upper gluteal artery, coming from internal iliac artery that emerges above the pyriform muscle and irrigates the upper portion of GMM; lower gluteal artery, also a branch of internal iliac artery, that penetrates the region below the pyriform muscle, feeding the GMM lower half; and branches of femoral system, from femur circumflex lateral and middle arteries and lower gluteal artery, forming the so-called "cruciate anastomosis", that supplies the more distal portion of GMM. Innervation is achieved by the lower gluteal nerve only, formed by L5, Sl and S2 roots and reaches gluteus region below the pyriform muscle(9).
GMM's main action is located at the thigh and pelvis extension, exerting a co-operating role at side rotation of the hip joint and thigh adduction and abduction.
Due to this, muscle sacrifice in patients that normally stroll must be avoided, as such a procedure would lead to difficulties in executing some movements such as climbing stairs, walking on steep places and even running(6, 8).
MATERIAL AND METHODS
The study was carried out between February 1994 and October 1998 comprised 22 patients, from which 20 (90.9%) presented neurological disorders such as paraplegia (18 patients = 81.8%) and tetraplegia (2 patients = 9.1%), with 2 other (9.1%) that did not present any sequela. Twenty-four ulcers were restored, of which the source mechanisms were ischemia due to prolonged stress in 22 cases (91.7%) and burning by electrical bistoury plate in 2 other ones (8.3%).
From the total of patients, 14 were male (63.6%) and 8 female (36.4%); 10 were niger (45.5%), 7 were dark (31.8%) and 5 white (22.7%). Age ranged between 14 and 47 years old.
Ulcer location was in sacral region in 12 cases (50.0%) in ischial region in 7 (29.2%), and trochanteric region in 5 (20.8%) with dimensions that ranged from 3.5 x 4.0 cm to 8.0 x15.0 cm in sacral, 3.0 x 3.0 cm to 4.5 x 8.5 cm in ischial and 2.5 x 5.0 cm to 5.0 x 8.0 cm in trochanteric region. Lack of accurate information prevented the adequate ascertainment of the period between the appearance of ulcer and its covering.
The lesions were never surgicaliy treated in 21 cases (87.5%) and showed to be relapses in 3 (12.5%) after procedures not described here; 2 patients (9.1%) presented simultaneous ulcers at sacral and trochanteric regions that were restored in different times; 2 sacral ulcers (8.3 %) of greater sizes (one measuring 7.0 x 12.5 cm and the other 8.5 x 15.0 em) needed concurrent employment of 2 flaps (7.7%) for the proper closing of a single lesion, which determined a total of 26 flaps for restoration of 24 ulcers.
SURGICAL TECHNIQUE
Once at operating room and after venous puncture by the anesthesiologist, the pátient was sedated with the associated purpose of minimizing lower limbs spastic contractions that all of thern presented in major or minor degree. At that moment, antibiotic prophylaxis was also instituted with 2 g cephalosporin, maintained for 48 hours.
With the patient in dorsal decubitus or, in case of trochanteric lesions, slightly lateral, the surgical procedure was initiated by ulcer and eventual neighboring pouches (bursas) excision, besides underlying bone eminence planing. In no case the enlarged bone excision was carried out. Strict hemostasis by electrocautery and apposition of physiological saline completed this preparation step of receptor area.
Following, V-Y flap was planned by having it with its larger axle (length) twice the ulcer size and its smaller axle (width) with size equal or slightly larger than that of the lesion (Fig. la) according to parameter. Actually, we did not stick to measures as the previous evaluation allowed us to analyze tegument elasticity of the region and how much the future flap could be advanced.
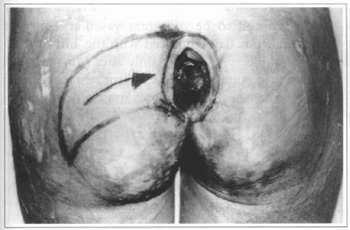
Fig. la - Sacral ulcer with lesion excision markings and planing of V-Y gluteus flap.
Then we proceeded with flap dissection, which implied a skin incision up to, and induding facial plane.
There were no incisions in musculature (Fig. 1b). A small segment of the flap end nearest to ulcer was detached between fascia and muscle in order to facilitate its advance; the same way, the flap's more distant end was also detached at subfascial layer in order to be better accommodated, the central piece remaining unharmed in order to preserve perforating arteries responsible for cutaneous site irrigation (Fig. lc). All surgical injuries were tubularly drained for four to five days (Fig. ld) and the sutures taken out after 15 days.
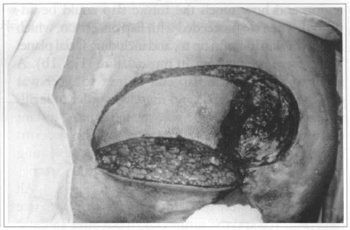
Fig. lb - Sacral area to be restored ready to receive the already incised flap.
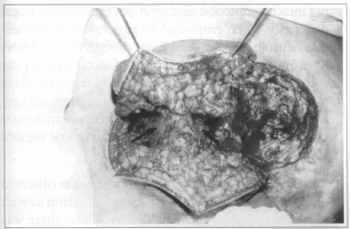
Fig. lc - Detail of V-Y flap showing its end detachment between the fascia and the muscle without reaching the central part in order to preserve perforating arteries. Note maintenance of the gluteus maximum muscle integrity (arrows) that does not undergo section or de-insertion by this approach.
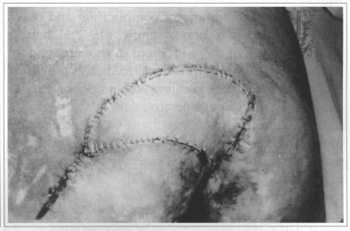
Fig. ld - Immediate postoperative showing ample advance of fasciocutaneous block with plain coverage of sacral lesion. Tubular drainage by donor area incision.
RESULTS
No suffering or losses of any flap occurred at any time, with all of them showing to be fully feasible (Figs. 2a and 4b), with no significant complication and only tiny dehiscences in 5 surgical injuries (19.2%), being 3 sacral (25.0% of those localized in this site) and 2 trochanteric (40.0% of those localized in this site) that evolved to spontaneous healing with proper dressings between 10 and 15 postoperative days, without prejudice restoration. These intercurrences were attributed to more intense spastic contractions presented by these patients in spite of benzodiazepinics having been maintained for all of them up to the 15th postoperative day. Patients not bearing neurological disturbances strolled normally without showing any degree of functional deficiency.

Fig. 2a - Sacral ulcer that presented itself with 5.0 x 4.5 em after preparation. Central area flap markings that will not be shifted at subfascial plane in order to preserve perforating arteries.
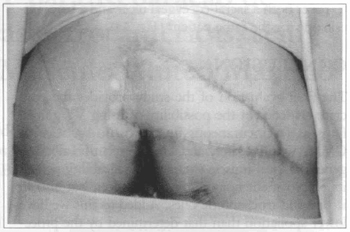
Fig. 2b - Two month postoperative.
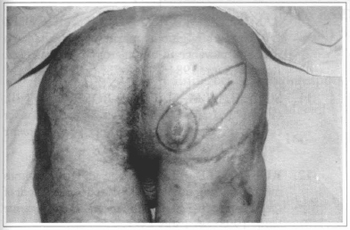
Fig. 3a - Ischial ulcer relapsed with 6.5 x 5.0 cm.
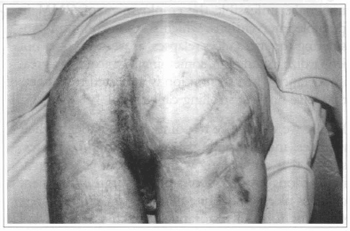
Fig. 3b - Four month postoperative.
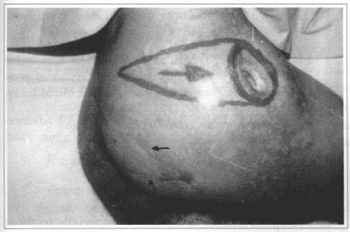
Fig. 4a - Trochanteric ulcer with 4.5 x 6.0 cm. This patient had already been submitted to sacral-coccygeal ulcer restoration thtough similar flap at the same side (arrows).

Fig. 4b - Five month postoperative.
Due to the patients involved in the study come from other institutions the postoperative follow-up was not ideally conducted but those managed to be monitored after the 3rd month, with a total of 10 patients (45.45%) remained with no compromise of reconstitution or process relapse. It is important to point out that all 22 patients operated were followed-up up to the 2nd month following the procedure, which allowed us to observe the efficacy of the method described.
DISCUSSION
The use of cutaneous-adipose overlay from gluteal region to dose sacral injuries has for long constituted the primary option for recomposing such lesions(1, 3).
The introduction of myocutaneous flaps in the therapeutic arsenal of Plastic Surgery brought the possibility to plan and make larger and safer flaps, allowing even more extensive and hard-working restorations.
GMM turned to be the great vascular vector of myocutaneous flap employed with the aim of treating sacral ulcers(5, 6, 10, 13}, mainly after Minami's et al study(14). In spite of being excellent, the application of myocutaneous flaps imposes muscle de-insertions or transections according to several authors in Literature(2, 5, 6,10, 14). Thus, a greater blood loss is instituted with the consequent increase of operation time through a longer hemostasis, leading to a greater spoliation of the patient. Still as limitation, there is the minor or major harm to the muscle function(6, 7,10, 13, 14).
The method explained here, such as that described by Ohjimi et al(7) and also Park(15), supports the non-aggression to muscle integrity, preserving it as an capable unit in eventual reoperations and also maintaining intact its function aiming at not causing functional deficiency when employed in patients with no definite neurological sequela. Even though these authors have employed it for restoration of sacrallesions only, the great tegument mobility of gluteal region, even in patients that grew thin, makes feasible a large and easy advance of these flaps to several directions, making it possible to reach also ischial and trochanteric regions as a fasciocutaneous block.
Operative field limited to gluteal region was observed to bring an optimization of the surgical action as with reference to ischial and trochanteric ulcers there was no need of tissue handling in other topographies as it would be expected in case thigh flaps were used, an option frequently employed to restoration of such lesions(l, 2, 5, 6). The versatility of the proposed method is also evidenced by the possibility of employing it according to GMM's vascular pedicle(8), i.e., one V-Y flap may be planned for the lower half of gluteal region and another one for the upper one, for instance, to cover both a sacral-coccygeal ulcer and a trochanteric one for the sarne patient (Fig. 4a).
CONCLUSION
The final evaluation of the study provides the concrete evidence of the possibility of using V-Y gluteal flaps as fasciocutaneous unit with no sacrifice to GMM. Vascular safety and simple execution allied to generous local muscle-cutaneous malleability permit its employment not only in sacral ulcer, but also in ischial and trochanteric ones. Added to this we have lower spoliation than that determined by the procedure as it does not require muscle transections, presents lower bleeding and consequently lower operation time.
It should be reminded that the method for maintaining muscle integrity offers double benefit as it does not make unfeasible the employment of GMM in possible interventions, which is no uncommon considering the stress ulcer relapses, as well as it does not jeopardize its function, something that acquires a great importance when this option is indicated to patients that have not lost strolling capacity.
Finally ,we would like to point out the patients, their relatives' indispensable participation and/or professionals that carne along with them as well, concerning the long-lasting success of the surgical treatment of stress ulcers in definite neurological lesion bearers since any form of restoration in such situations will be failed in case daily care such as decubitus change and physiotherapy are not provided , which the patients will require during their lifetime.
REFERENCES
1. COLEN SR. Pressure sores. In: MCARTHY JG. Plastic Surgery. WB Saunders Company. 1990; 6:3797-3838.
2. LION PM, REBELLO C. Tratamento cirúrgico das úlceras de pressão. Rev. Col. Bras. Cir. 1993; 6:322-336.
3. CONWAY H, GRIFFITH BH. Plastic Surgery for closure of decubitus ulcers in patients with paraplegia based on experience with 1000 cases. Am. J. Surg. 1956; 91:946-974.
4. GER R. The surgical management of decubitus ulcers by muscle transposition. Surgery. 1971; 69:106-110.
5. MATHES SJ, NAHAI F. Clinical Atlas of Muscle and Musculocutaneous Flaps. St. Louis : The Mosby Company, 1979.
6. HOCHBERG J. Manual de Retalhos Miocutâneos. Porto Alegre: AMRIGS, 1984.
7. OHJIMI H, OGATA K, SETSU Y, HARAGA L. Modification of the gluteus maximus V-Y advancement flap for sacral ulcers: The gluteal fasciocutaneous flap method. Plast. Reconstr. Surg. 1996; 98:1247-1252.
8. NETTER FH. The Ciba Collection of Medical Illustration, Muskuloskelectal System - Part 1. 1987; 8:79-91.
9. NETTER FH.Atlas de Anatomia Humana. Porto Alegre: Artemed. 1998; p. 472.
10. RAMlREZ OM, ORLANDO JC, HURWITZ DJ. The sliding gluteus maximus myocutaneous flap: its relevance in ambulatory patients. Plast. Reconstr. Surg. 1984; 74:68-75.
11. SCHEFLAN M, NAHAI F, BOSTWICK J III. Gluteus maximus island musculocutaneous flap for closure of sacral and ischial ulcers. Plast. Reconstr. Surg. 1981; 68:533-538.
12. RUBAYI S, DOYLE BS. The gluteus maximus muscle-spliting myocutaneos flap for treatment of sacral and coccigeal pressure ulcers. Plast. Reconstr. Surg. 1995; 96:1366-1371.
13. PARRY SW, MATHES SJ. Bilateral gluteus maximus miocutaneous advancement flaps: sacral coverage for ambulatory patients. Ann. Plast. Surg. 1982; 8:443-445.
14. MINAMI RT, MILLS R, PARDOE R. Gluteus maximus myocutaneous flaps for repair of pressure sores. Plast. Reconstr. Surg. 1977; 60:242-249.
15. PARK C, PARK B. Fasciocutaneous V-Y advancement flap for repair of sacral defects. Ann. Plast. Surg. 1988; 21:23-26.
ACKNOWLEDGEMENTS
To Petrópolis School of Medicine, especially to those professionals of the Library and Computer Laboratory for the indispensable help in the working up of this work.
I - Senior Member of the Brazilian Society of Plastic Surgery.
II - Senior Member of SBC, chief of the Plastic Surgery Department of Hospital da Beneficência Portuguesa, Petrópolis, Rio de Janeiro, Brazil.
III - Aspiring Member of SBCP.
Address for correspondence:
Sérgio Cardoso Maciel, MD
R. Dom Pedro I,166
25620-010 - Petrópolis - RJ Brazil
Fone: (55-24) 245-4541 Fax: (55-24) 243-7181
e-mail cardosomaciel@cremerj.com.br
Work performed at the Plastic Surgery Department of Hospital Santa Teresa and Hospital da Beneficência Portuguesa, Petrópolis, Rio de Janeiro, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter