

Articles - Year 1999 - Volume 14 -
Uncommon Cases on Nose Surgery
Casos Incomuns na Cirurgia do Nariz
ABSTRACT
Three cases of nasal surgery requiring less used procedures in daily clinical practice are presented. In the first case, a tibial graft early carried out was rcused and associated to cartilaginous graft and inclusion of porous polyethylene. Converse flap was used for the second case and nasal dorsum tissue expansion was the resource adopted for the third case. The results obtained are shown and conduct in each case is discussed.
Keywords: Nose; rhinoplasty; nasal reconstruction
RESUMO
Apresentação de três casos de cirurgia nasal que necessitaram de procedimentos pouco utilizados na prática clínica diária. No primeiro caso, reaproveitou-se um enxerto tibial, realizado em tempo operatório prévio, associando-o a enxerto cartilaginoso e inclusão de polietileno poroso. O retalho de Converse foi usado no segundo caso e a expansão de tecido do dorso nasal foi o recurso adotado no terceiro caso. São mostrados os resultados obtidos e discutida a condução de cada caso.
Palavras-chave: Nariz; rinoplastia; reconstrução nasal
Treatment of rhinoplasty sequelae and nose reconstruction have arisen the plastic surgeon interest and allowed for a rich production of scientific papers.
Nasal reconstruction seemingly originated in India, in 3,000 B.C., using frontal region skin and, in other times and places, flaps for nasal reconstruction came from arm (Tagliacozzi, 1597), neck, abdomen and shoulder. More modern methods evolved to three basic lines: (1) Indian method, with the use of frontal median flap; (2) French method, using side flaps at nasolabial and face region, and (3) Italian method, involving brachial flap. Nowadays we also rely on microsurgical flaps and the use of dermoexpanders(1).
Converse proposed the performance of an axial cutaneous flap ("scalp flap") based on superficial temporal artery that uses frontal region tegument advancing to nasal region. This flap pedicle includes a scalp segment which, after integration period, is returned to its original position and the remaining bloody zone is repaired with skin free graft(2,3).
One of the difficulties found in clinical practice is the choice of the ideal organic or inorganic material to replace tissues and correct nasal defects. Sheen(4) presented extensive rationale for the use of nasal septum and auricular concha autogenous cartilage in secondary rhinoplasty and reported this one as the ideal material for reparation of substance and support structure loss with good results.
CASE STUDY
Three clinical cases of patients victims of accident with nasal traumatism and submitted to previous treatmentin other services are presented.
CASE #1
Female patient victim of automobile accident with multiple nose fractures and submirted to several surgical interventions performed by different surgeons aiming at repairing trauma lesions (Figs. 1 and 2).
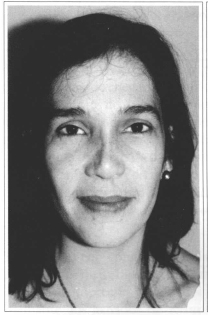
Fig. 1 - Preoperative photograph of case #1 patient, showing limits of glabella bone graft down to nasal tip.
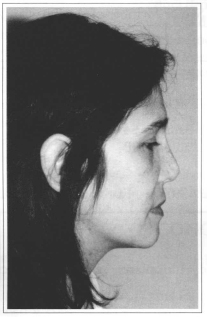
Fig. 2 - Preoperative photograph of case #1 patient, side view.
Among the previously carried out procedures, an autogenous bone grafting from a tibial segment for repairing nasal dorsum was carried out. The bone graft was introduced under pressure ("fastened with pegs") at glabella region and its lower end was situated at nasal tip (Figs. 3 and 4).
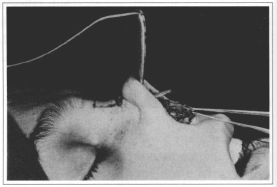
Fig. 3 - Case #1 intraoperative showing tibial bone graft reaching nasal tip region.

Fig. 4 - 3D-computerized tomography showing tibial bone graft surgically observed in Fig. 3.
The patient complained of non-esthetic aspect and nasal tip hardness. She was submitted to open sky treatment (open rhinoplasty) with graft section at its median portion, and distal fragment was transferred to right side of proximal fragment (fixed) in close contact to this and fixed by steel thread. Nose median third and tip regions were repaired with auricular cartilage autogenous graft, in such a way to achieve a esthetically better mobile tip. Despite the whole nasal dorsum being covered by temporal fascia graft, the patient presented nasal dorsum irregularities by the seven-month postoperative (Fig.5). It has been finally selected to use gutter-shape porous polyethylene (Medpor®) and, at the same surgical procedure, partially absorbed cartilaginous grafts were drawn achieving uniformity to the region (Fig. 6). Figures 7 and 8 present postoperative result 12 months after inclusion of porous polyethylene.
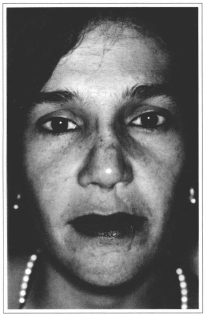
Fig. 5 - Photograph of case #1 patient presenting nasal dorsum irregularities seven months after last surgery.
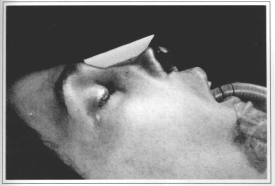
Fig. 6 - Case #1 intraoperative showing inclusion of canoe-shape porous polyethylene to be introduced at
nasal dorsum.
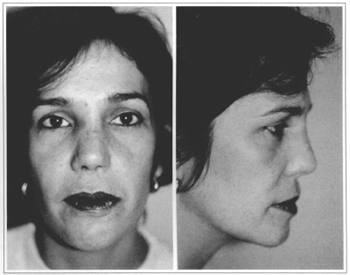
Figs. 7 & 8 - Photographs of case #1 patient in 12-month postoperative period after inclusion of porous polyethylene.
CASE #2
Patient victim of automobile accident with multiple facial wounds, including loss of the whole cutaneous coverage and nasal tip cartilages. At first care we carried out removal of all devitalized tissues and proceed to partial skin grafting for bloody area coverage and prevention of infection (Fig. 9).
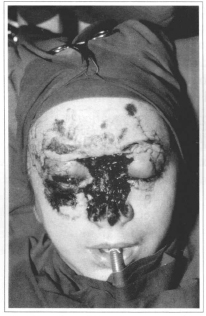
Fig. 9 - Case #2 patient presenting multiple face wounds and total loss of nasal coverage la days after trauma.
Emergency room surgeon report described a degloving at frontal region. This fact, associated to clinical examination of patient, showed vascular pedicle lesion and contraindicated execution of frontal median flap ("Indian flap"). For this reason, we chose to use Converse flap based on right superficial temporal artery with migration of frontal region medial portion to coat dorsum, tip and columella, carried out two month after skin graft. The cartilaginous losses were repaired with auricular cartilage autogenous grafts (Fig. 10). Figures 11, 12, 13 and 14 show the patient at 24-month postoperative period, waiting for orbitopalpebral reconstruction surgery.

Fig. 10 - Photograph of case #2 patient at posroperative twenty-first day after reconstruction with Converse flap upon pedicle release.
Figs. 11, 12 & 13 - Side, oblique and front view photographs of case #2 patient, at 24 month postoperative.
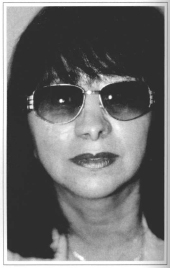
Fig. 14 - Photograph of case #2 patient wearing sun glasses for social life while awaiting for orbitopalpebral reconstruction surgery.
CASE #3
Patient victim of automobile accident with loss of part of the tip and lower third of nose. She was submitted to two other reparation attempts with two-sided. Converse flap that evolved to failure due to lack of proper vascular pedicle with necrosis and tegumental coverage loss at frontal region and scalp at head anterior portion. Figure 15 shows patient at three-week period after second attempt of Converse flap rotation during operating procedure for bloody area coverage.
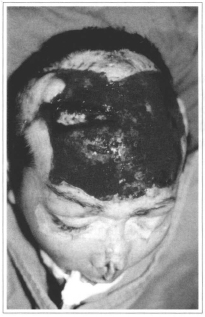
Fig. 15 - Photograph of case #3 patient showing frontal region and scalp anterior third tegumentary lesion.
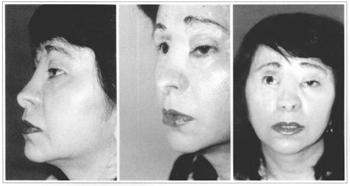
Lesions were first treated with partial skin autogenous graft for closing wounds and clinical improvement of patient (Fig. 16). At subsequent operative times, scalp expansion for head repairing and nasal dorsum expansion for tip correction were carried out (Fig. 17). Cartilaginous losses were repaired with auricular concha cartilage. Figure 18 shows partial result of reparation with correction of nasal wing junction remaining to be corrected with tip expanded tissue. Final result obtained at 20-day postoperative period is presented in Figures 19 and 20. Supplementary procedures may be carried out in a timely basis.

Fig. 16 - Photograph of case #3 patient, with skin graft integrated to frontal region. Nose presents nasal tip lesion with skin, cartilage and pad loss.
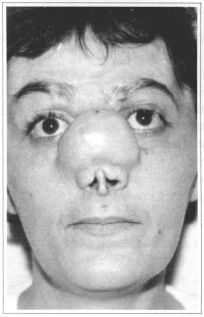
Fig. 17 - Photograph of case #3 patient in the cutaneous expansion period of nasal dorsum region, with frontal pileous region already reconstructed after great scalp expansion.

Fig. 18 - Photograph of case #3 patient showing expansion obtained, at 30-day postoperative period, awaiting for supplementary surgery.
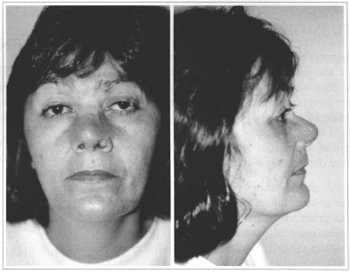
Figs. 19 & 20 - Photographs of case #3 patient at 20 day early postoperative period after last procedure.
DISCUSSION
Nose presents specific problems when any type of organic or alloplastic material is used as the thin skin and the region susceptible to strength action determine late irregularities and complications. Flexibility of the material employed is also an important issue as a too rigid tissue or a non-elastic inclusion determine the artificial appearance while too flexible materials may cause deformations in the long term(5).
In case #1, the thin skin of nasal region allowed observation of deformities arising from bone and cartilaginous grafts irregularity. Thus, we selected to use an inorganic material, gutter-shape porous polyethylene providing a regular nasal dorsum at its full extent.
Porous polyethylene (Medpor®) has been used in esthetic surgeries as well as for the correction of traumatic and congenital deformities. It is characterized by being such a material that allows for tissue growth into its pore inward and even bone tissue penetration(6,7)presenting low rates of complications.
Nasal tip reparation should not be carried out with rigid material and so auricular cartilage constitutes the ideal material to replace losses at this region. Peer(8), Jovanovic & Berghaus(9) et al. emphasized the long survival of cartilaginous autogenous draft, its availability and, its possibility of being sculptured.
The use of cutaneous flaps to substitute nasal tegument losses must always give priority to the neighboring tissues that have proper coloration and thickness to cover nose. Execution of flaps with axial pedicles requires anatomical knowledge and technical skills of the surgeon as the failures in these surgeries lead to hard resolution sequelae.
In case #2, the impossibility of performing frontal median flap ("Indian") led us to indicate Converse flap. The advantage of this flap is that it has sufficient tissue to reconstruct the nose lobule portion and columella and in addition, its length provides attainment of proper size and projection of nasal tip. The ideal cutaneous coverage should respect the nose esthetic unit.
The use of expanders of nasal dorsum tissue has a very limited indication but, in case #3, seemed to be the best option as the other alternatives would add scars to nasolabial regions or would imply the use of flaps at distance with less favorable esthetic results.
REFERENCES
1. BARTON JR FE, BYRD HS. Acquired deformities of the nose. In: MCCARTHY JG. Plastic Surgery. Vol. 3, Philadelphia : WB Saunders, 1990. p. 1924-1987.
2. CONVERSE JM. New forehead flap for nasal reconstruction. Proc. R. Soc. Med. 1942;35:811-812.
3. CONVERSE JM, MCCARTHY JG. The scalping forehead flap revisited. Clin. Plast. Surg. 1981;8(3):413-34.
4. SHEEN JH. Problems in secondary rhinoplasty. In: Aesthetic Rhinoplasty. 2. ed. Missouri : CV Mosby, 1987. p. 1135-1188.
5. GOODMAN WS, GILBERT RW. Augmentation in rhinoplasty - a personal view. J. Otolaryngol. 1985;14:107-112.
6. WELLISZ T. Clinical experience with the Medpor porous polyethylene implant. Aesth. Plast. Surg. 1993;17:339-344.
7. MINAMI E, FERREIRA JCR, FADUL JRR, FERREIRA LM. Estudo experimental e clínico do polietileno poroso em cirurgia plástica. In: XXXIV Congresso Brasileiro de Cirurgia Plástica, São Paulo, 1997. p. 40.
8. PEER LA. Cartilage grafting. Surg. Clin. North America. 1944;24:404-419.
9. JOVANOVIC S, BERGHAUS A. Autogenous auricular conchal cartilage transplant in corrective rhinoplasty. Practical hints and critical remarks. Rhinology. 1991;29:273-280.
I - MD and Master Degree on Plastic Surgery by Universidade Federal de São Paulo, Plastic Surgery Department - Escola Paulista de Medicina. Senior Member of Brazilian Society of Plastic Surgery. General Secretary of Brazilian Society of Craniomaxilofacial Surgery.
II - Postgraduated, with Doctor and Master Degree on Plastic Surgery by Universidade Federal de São Paulo - Escola Paulista de Medicina. Senior Member of the Brazilian Society of Plastic Surgery.
Address for correspondence:
José Carlos R. Ferreira, MD
Rua Dr. Guilherme Bannitz, 54
04532-060 - São Paulo - SP Brazil
Phone: (55 11) 829-7977
Fax: (55 11) 822-8123


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter