

Original Article - Year 2018 - Volume 33 -
Cleft lip and palate: evaluation of the psychological impact using the Rosenberg self-esteem scale
Fissura labiopalatina: avaliação do impacto psicológico utilizando a Escala de Autoestima de Rosenberg
ABSTRACT
Introduction: Cleft lip and palate is the most frequent malformation of the head region and
affects more than 10 million people worldwide. This study aims at evaluating
the self-esteem in patients with cleft lip and palate and comparing that
with the self-esteem of non-affected individuals during follow-up at the
Department of Craniomaxillofacial Plastic Surgery of the Hospital de
Clínicas of Porto Alegre.
Methods: This is a cross-sectional, contemporary study with 160 participants,
comprising 80 patients with cleft lip and palate who have already undergone
surgical procedures for correcting the condition and 80 non-affected
students and employees of the public-school system as a control group. We
used a questionnaire to characterize the group and the Rosenberg self-esteem
scale for data collection.
Results: There was a significant difference between groups in terms of marital status,
schooling, and school retention. Patients with a cleft lip and palate had
lower levels of self-esteem than non-affected individuals. Among them, the
individuals with bilateral clefts or complete clefts; female gender;
economic strata of D/E; low level of schooling; families reconstituted
during childhood; and with unsatisfactory results concerning communication,
dentition, and lip scar also showed lower levels of self-esteem.
Conclusion: There was a significant relationship between cleft lip and palate and low
self-esteem.
Keywords: Cleft lip; Mental health; Congenital abnormalities; Self-image; Nursing
RESUMO
Introdução: A fissura labiopalatina é a malformação mais frequente da região da cabeça e
afeta mais de 10 milhões de pessoas no mundo. O objetivo do estudo foi
avaliar a autoestima em pacientes portadores de fissura labiopalatina em
acompanhamento no Serviço de Cirurgia Plástica Craniomaxilofacial do
Hospital de Clínicas de Porto Alegre, comparando-os com indivíduos não
fissurados.
Métodos: Estudo transversal contemporâneo, com 160 participantes, sendo 80 pacientes
com fissura labiopalatina já submetidos a procedimentos cirúrgicos
relacionados à afecção e, como grupo controle, 80 alunos e funcionários da
rede pública de ensino. Um questionário para caracterizar o grupo e a escala
de autoestima de Rosenberg foram utilizados para a coleta de dados.
Resultados: Houve diferença significativa entre os grupos quanto ao estado civil,
escolaridade e repetência escolar. Os pacientes com fissura labiopalatina
apresentam níveis de autoestima menores em relação a indivíduos não
afetados. Dentre eles, os subgrupos dos indivíduos com fissura bilateral,
fissura completa, do gênero feminino, classe econômica D/E, baixa
escolaridade, situação familiar reconstituída na infância e com resultados
não satisfatórios em relação à comunicação, dentição e cicatriz de lábio
também mostraram níveis de autoestima menores.
Conclusão: Houve relação significativa entre fissura labiopalatina e baixa
autoestima.
Palavras-chave: Fenda labial; Saúde mental; Anormalidades congênitas; Autoimagem; Enfermagem
INTRODUCTION
Cleft lip and palate (CLP) is a congenital anomaly that affects approximately one in every 700 live births1. These deformities can cause functional problems in the dental arch, chewing, breathing, and hearing2. The difficulty in efficient communication and the compromise of the physical appearance make individuals with CLP a possible target of derogatory adjectives in social groups. These physical and functional changes may lead to other potential damages in patients’ lives: the psychosocial ones3.
Facial appearance has a profound influence on social environments, personality development, and educational progress. People with CLP may present unfavorable levels of anxiety, depression, social phobia, self-esteem, and quality of life4.
The measurement of self-esteem has been conducted worldwide via the Rosenberg self-esteem scale (RSES), which can classify self-esteem in adolescents, adults, and the elderly5.
The importance of the topic and the limited number of studies using reliable assessment tools justify our interest in this subject.
OBJECTIVE
We aim to evaluate the self-esteem of individuals with CLP compared with individuals not affected by the condition, to determine possible factors that influence the self-esteem of these patients, and to identify the most affected subgroups.
METHODS
This cross-sectional, contemporary study comprised 160 individuals of both genders aged between 12 and 50 years. The study participants were equally divided into two groups. The G1 or exposed group consisted of patients with CLP, who had already undergone a surgery related to the condition, followed by craniomaxillofacial plastic surgery at the Hospital de Clínicas of Porto Alegre, RS, (HCPA). The G2 or control group consisted of individual students and employees of the public-school system in the same city without CLP.
The minimum age of individuals for inclusion in the study was determined to be 12 years to ensure ability to understand the issues of self-esteem.
The exclusion criteria for both groups were the presence of any type of central hearing syndromes or dysfunctions. The individuals or legal guardians who did not provide consent for their inclusion by signing the informed consent form (ICF) or who did not adequately fill out the questionnaire were excluded from the study.
The G1 group consisted of patients who attended the appointment at the Cleft Lip and Palate Ambulatory. Patients and/or family members were informed about the study and presented with the ICF. Subsequently, self-esteem tests using RSES and a structured questionnaire, formulated specifically for this study, were conducted. Data were also compiled from the medical records. The G2 individuals were selected from the municipality’s Education Department of a public school.
All students and school staff received sealed envelopes with the study cover letter, the structured questionnaire, and the ICF. For the inclusion of students under the age of 18 years, documentation for parents or guardians was sent. After the return of the documentation, a draw of 50 students under the age of 18 years and 30 individuals over the age of 18 years was conducted. At the school, in a reserved room, the self-esteem was tested using RSES for all included individuals.
Data collection was carried out from August to December 2012.
For data collection, a questionnaire was prepared for each research group. For the G2 group, the questionnaire included questions about personal information and questions related to schooling, school retention, economic class, and family situation. For the G1 group, in addition to the parameters mentioned above, questions related to CLP classification, surgical procedures, and healthcare institutions where they were when selected were also included.
The results were evaluated in terms of communication, dentition, functionality, and aesthetics of lips and nose with the help of an assisting team including a speech therapist, dentist, otorhinolaryngologist, and plastic surgeon, respectively. Patients were asked about their opinions on the results.
RSES used in this study is a scale developed for the evaluation of self-esteem and is used globally. RSES consists of 10 items with questions regarding the feelings of self-respect and self-acceptance. It was adapted to Portuguese with good psychometric indices. The sum of the scores for the 10 items provided the final score on the scale, which ranged from 10 to 40. The results were categorized as high, normal, and low self-esteem6.
This study and the ICF were approved by the Research and Post-Graduation Group of HCPA and its Committee of Research Ethics under protocol number 11-0021. Authorization was requested from the Education Department of Porto Alegre to conduct the research at the school. No permit was required for using RSES.
RESULTS
Initially, we characterized the sample as presented in Table 1. The sample was mostly homogeneous with unpaired groups. There was a significant difference only between groups with regard to marital status, schooling, and school repetition.
| Variables | Total sample (n = 160) |
Cleft Lip and Palate Group (n = 80) |
Control Group (n = 80) |
p value* |
|---|---|---|---|---|
| Age group (years) | ||||
| 12–18 | 103 (64.4) | 53 (66.3) | 50 (62.5) | 0.741 |
| ≥19 | 57 (35.6) | 27 (33.8) | 30 (37.5) | |
| Gender | ||||
| Male | 75 (46.9) | 42 (52.5) | 33 (41.3) | 0.205 |
| Female | 85 (53.1) | 38 (47.5) | 47 (58.8) | |
| Marital status | ||||
| Not married | 128 (80.0) | 71 (88.8) † | 57 (71.3) | 0.015 |
| Married | 25 (15.6) | 8 (10.0) | 17 (21.3) † | |
| Divorced/Widowed | 7 (4.4) | 1 (1.3) | 6 (7.5) | |
| Education | ||||
| Incomplete elementary | 71 (44.4) | 50 (62.5) † | 21 (26.3) | <0.001 |
| Complete elementary | 32 (20.0) | 10 (12.5) | 22 (27.5) † | |
| High school/College | 57 (35.6) | 20 (25.0) | 37 (46.3) † | |
| School retention | ||||
| Yes | 59 (36.9) | 41 (51.3) | 18 (22.5) | <0.001 |
| No | 101 (63.1) | 39 (48.8) | 62 (77.5) | |
| Economic strata | ||||
| E | 36 (22.5) | 17 (21.3) | 19 (23.8) | 0.730 |
| D | 48 (30.0) | 22 (27.5) | 26 (32.5) | |
| C | 69 (43.1) | 38 (47.5) | 31 (38.8) | |
| B | 7 (4.4) | 3 (3.8) | 4 (5.0) | |
| Family situation in childhood | ||||
| Nuclear | 106 (66.3) | 59 (73.8) | 47 (58.8) | 0.133 |
| Reconstituted | 44 (27.5) | 17 (21.3) | 27 (33.8) | |
| Others | 10 (6.3) | 4 (5.0) | 6 (7.5) | |
| Current family situation | ||||
| Nuclear | 88 (55.0) | 48 (60.0) | 40 (50.0) | 0.203 |
| Reconstituted | 53 (33.1) | 25 (31.3) | 28 (35.0) | |
| Others | 10 (6.3) | 2 (2.5) | 8 (10.0) | |
| Living alone | 9 (5.6) | 5 (6.3) | 4 (5.0) |
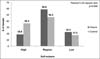
A significant association was observed between CLP and self-esteem (p = 0.046). The CLP group had a significantly higher proportion of individuals with normal and low self-esteem, as can be seen in Figure 1.
In the analysis of the CLP group shown in Table 2, the variables that were found to be associated with low self-esteem in the CLP group were female gender, incomplete elementary education or complete elementary education, D/E strata, and reconstituted family during childhood.
| Variables | Normal self-esteem | Low self-esteem | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) |
p value | Adjusted OR (95% CI) |
p value | |
| CLP group | 2.20 (0.90-5.40) |
0.085 | 3.86 (1.15-12.9) |
0.028 |
| Women | 1.82 (0.80-4.13) |
0.153 | 3.18 (1.07-9.50) |
0.038 |
| Level of schooling | ||||
| Incomplete elementary | 1.70 (0.63-4.55) |
0.293 | 4.74 (1.11-20.2) |
0.035 |
| Complete elementary | 1.01 (0.33-3.13) |
0.989 | 5.29 (1.16-24.1) |
0.032 |
| With school retention | 1.53 (0.56-4.16) |
0.405 | 0.64 (0.18-2.27) |
0.491 |
| Class of D/E | 1.35 (0.59-3.08) |
0.483 | 4.44 (1.40-14.1) |
0.012 |
| Childhood family situation | ||||
| Nuclear | 1.0 | 1.0 | ||
| Reconstituted | 1.63 (0.58-4.56) |
0.353 | 4.19 (1.16-15.1) |
0.029 |
| Other | 0.38 (0.07-1.97) |
0.250 | 1.08 (0.18-6.63) |
0.934 |
Table 3 shows the group under study. With regard to the classification of the cleft, 64 (80.0%) individuals had lip and palate clefts, 56 (70.0%) had unilateral clefts, and 65 (81.2%) had complete clefts. With regard to treatment location for CLP, 47 individuals (58.8%) were operated by the plastic surgery service only at HCPA, whereas 14 (17.5%) underwent all surgeries at other institution(s) but were referred to the Cleft Lip and Palate Ambulatory for further assistance; 19 (23.8%) patients underwent surgical procedures at other institution(s) and the plastic surgery service.
| Variables | Total sample (n = 80) |
|---|---|
| Classification of the cleft | |
| Lip and palate | 64 (80.0) |
| Lip | 12 (15.0) |
| Palate | 4 (5.0) |
| Unilateral | 56 (70.0) |
| Bilateral | 24 (30.0) |
| Complete | 65 (81.2) |
| Incomplete | 15 (18.8) |
| Repair surgery | |
| Lip surgery only | 12 (15.0) |
| Palatal surgery only | 4 (5.0) |
| Lip + palatal surgery | 64 (80.0) |
| Treatment | |
| Only at HCPA | 47 (58.8) |
| Other institution(s) and HCPA | 33 (41.2) |
| Evaluation of the results by the assisting team regarding the following: | |
| Communication | |
| Good | 31 (38.8) |
| Fair | 19 (23.8) |
| Bad | 30 (37.5) |
| Dentition | |
| Good | 36 (45.0) |
| Fair | 12 (15.0) |
| Bad | 32 (40.0) |
| Lip | |
| Good | 39 (48.8) |
| Fair | 21 (26.3) |
| Bad | 20 (25.0) |
| Nose | |
| Good | 53 (66.3) |
| Fair | 13 (16.3) |
| Bad | 14 (17.5) |
| Patient outcome | |
| Pleased | 20 (25.0) |
| Dissatisfied | 60 (75.0) |
| What do they want to change? | |
| Communication | 21 (26.3) |
| Teeth | 35 (43.8) |
| Lip | 31 (38.8) |
| Nose | 17 (21.3) |
According to the assisting team for patients with CLP, the communication skills of 31 (38.8%) patients was considered to be good, and 30 (37.5%) were assessed to have poor communication skills. With regard to dentition, 36 (45.0%) were evaluated to have good dentition, and 32 (40.0%) were found to have poor dentition. Furthermore, according to the team, the lip aesthetics of 39 (48.8%) individuals were considered to be good, whereas nose aesthetics were considered to be good in 53 (66.3%) of the affected individuals.
Of the patients with CLP, 60 (75.0%) were dissatisfied with one or more of the evaluated items, and dentition presented the highest indices for dissatisfaction, 35 individuals (43.8%), followed by lip aesthetics with 31 (38.8%) dissatisfied individuals. The number of complaints concerning communication and nose aesthetics was lower, as shown in Table 3.
Table 4 describes the association between low self-esteem and fissure classification (p = 0.026). Patients who had undergone only lip surgery (for cleft lip) were associated with higher self-esteem than others (p = 0.047). Further, an association between the quality of communication and dentition and self-esteem (p < 0.001 and p = 0.031, respectively) was also observed.
| Variables | High self-esteem (n = 15) |
Normal self-esteem (n = 47) |
Low self-esteem (n = 18) |
p value |
|---|---|---|---|---|
| Classification of the cleft | ||||
| Lip and palate | 10 (66.7) | 39(83.0) | 15 (83.3) | 0.241 |
| Lip | 5 (33.3) | 5 (10.6) | 2 (11.1) | |
| Palate | 0 (0.0) | 3 (6.4) | 1 (5.6) | |
| Unilateral | 12 (80.0) | 36 (76.6) | 8 (44.4) | 0.026 |
| Bilateral | 3 (20.0) | 11 (23.4) | 10 (55.6) | |
| Complete | 11 (73.3) | 38 (80.9) | 16 (88.9) | 0.519 |
| Incomplete | 4 (26.7) | 9 (19.1) | 2 (11.1) | |
| Repair surgery | ||||
| Lip | 6 (40.0) | 4 (8.5) | 2 (11.1) | 0.047 |
| Palate | 0 (0.0) | 3 (6.4) | 1 (5.6) | |
| Lip + Palate | 9 (60.0) | 40 (85.1) | 15 (83.3) | |
| Evaluation of the results by the supporting team regarding: | ||||
| Communication | ||||
| Good | 11 (73.3) | 18 (38.3) | 2 (11.1) | < 0.001 |
| Fair | 3 (20.0) | 14 (29.8) | 2 (11.1) | |
| Bad | 1 (6.7) | 15 (31.9) | 14 (77.8) | |
| Dentition | ||||
| Good | 11 (73.3) | 18 (38.3) | 7 (38.9) | 0.031 |
| Fair | 0 (0.0) | 11 (23.4) | 1 (5.6) | |
| Bad | 4 (26.7) | 18 (38.3) | 10 (55.6) | |
| Lip | ||||
| Good | 12 (80.0) | 22 (46.8) | 5 (27.8) | 0.052 |
| Fair | 2 (13.3) | 12 (25.5) | 7 (38.9) | |
| Bad | 1 (6.7) | 13 (27.7) | 6 (33.3) | |
| Nose | ||||
| Good | 13 (86.7) | 31 (66.0) | 9 (50.0) | 0.112 |
| Fair | 1 (6.7) | 6 (12.8) | 6 (33.3) | |
| Bad | 1 (6.7) | 10 (21.3) | 3 (16.7) | |
| Patient Outcome | ||||
| Pleased | 10 (66.7) | 10 (21.3) | 0 (0.0) | < 0.001 |
| Dissatisfied | 5 (33.3) | 37 (78.7) | 18 (100) | |
| What do they want to change | ||||
| Communication | 0 (0.0) | 9 (19.1) | 12 (66.7) | < 0.001 |
| Teeth | 3 (20.0) | 21 (44.7) | 11 (61.1) | 0.059 |
| Lip | 1 (6.7) | 19 (40.4) | 11 (61.1) | 0.006 |
| Nose | 2 (13.3) | 10 (21.3) | 5 (27.8) | 0.600 |
Individuals who wanted to improve communication and lip aesthetics were more likely to have a low self-esteem (p < 0.001 and p = 0.006, respectively). Finally, all those who were affected and had a low self-esteem wanted to improve their results (p < 0.001).
DISCUSSION
Patients’ perception of CLP with regard to its impact on their life is recognized as an important health indicator. There is a notable consensus in the reports from CLP patients concerning the difficulties faced by them and the set of negative emotions involved, such as anxiety, fear of social assessment, low self-esteem, unfavorable body image, and social phobia7,8.
Self-esteem is considered an important indicator of mental health9 and one of the factors that interferes the most with human relations, educational progress, and psychosocial development. RSES is currently the most widely used instrument for the evaluation of self-esteem worldwide6 and is widely accepted in the scientific community.
The results of this study indicate that single status, low educational level, and school repetition are seen in a higher proportion in patients with CLP than in non-affected individuals.
Some studies10,11 have indicated on the association of CLP with school performance of affected individuals. Consequently, these individuals also present higher rates of school retention. The emotional aspects of children with CLP interfere with their learning ability in early school years. There is no report associating facial deformity with intellectual deficit; on the contrary, children with CLP have intellectual conditions similar to those of children considered normal for good school performance.
A school is a child’s first non-family contact with the society, and facial aesthetics form the first impression one makes of an individual. Children with CLP are not spared criticism by their peers, which in turn negatively affects their academic, social, and emotional lives. School failure may also be related to changes in auditory function and/or communication, which are essential for the learning process.
We observed that young adults with CLP feel greater difficulty in an interpersonal and affective relationship, in accordance with previous results12. This fact is evident in adolescence, as it is during this phase that a greater concern with physical appearance arises. If individuals do not feel satisfied with their appearance, they develop a feeling of inferiority and become insecure.
In the self-esteem analysis in this study, significant indices of low self-esteem were observed in women. Studies indicate that women express a greater dissatisfaction level with their appearance; this feeling is justified given the society pressure on women to have an attractive appearance13,14. Thus, women with CLP feel inferior, making it difficult for them to have social and affective interactions.
In the analysis concerning family structure, we observed low self-esteem in patients with CLP whose families during childhood did not include a father and a mother. The experience of parental separation or non-cohabitation of one of the parents causes psycho-emotional damage with varying degrees of intensity in all children.
Experiencing parental separation may have a more negative repercussion in individuals with CLP because in addition to living with the difficulties related to the condition, the lack of a family structure causes the feelings of insecurity. A family structure during childhood represents a significant maker for the affected patients as parents play an important role in the treatment.
CLP is also associated with the socioeconomic status of the individuals affected in the adult phase15. The results of this study show that the most disadvantaged economic classes (strata D/E) have a higher index of low self-esteem.
Individuals with CLP who experience social exclusion, along with the abovementioned problems, have difficulties with professional success because besides requiring technical and emotional competence, the professional industry seeks people with leadership and good communication skills.
An association between bilateral clefts of the lip and/or palate and low self-esteem was observed while evaluating factors related to affection. Bilateral clefts cause greater aesthetic damage, and it is more difficult to achieve satisfactory results in these patients. Concerning the classification of clefts, most individuals who underwent lip surgery without compromising the palate had a high self-esteem.
Patients who expressed dissatisfaction with lip aesthetics and phonation were more likely to have low self-esteem. All patients with low self-esteem wanted to improve their results with regard to aesthetics, lip, nose, or dentition, or functional aspects of communication.
These results agree with the results of other studies on this topic as all issues faced by the patients with CLP with regard to communication, scar of the lip, and dentition are shown to be directly related to their self-esteem.
CONCLUSION
Individuals with CLP have low levels of self-esteem compared with non-affected individuals.
Among patients with CLP, the subgroup of individuals with bilateral clefts, complete clefts, female gender, economic strata D/E, low educational level, families reconstituted during childhood, and with dissatisfaction with treatment results concerning communication, dentition, and scar further have lower rates of self-esteem.
Individuals with CLP have significant psycho-emotional fragility that should be considered during their treatment. In addition to medical, speech, and dental care, nurses, and geneticists, they need psychological support throughout their growth, development, and rehabilitation periods for the condition.
COLLABORATIONS
|
AG |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
|
SSC |
Analysis and/or interpretation of data; conception and design of the study; writing the manuscript or critical review of its contents. |
|
MVMC |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; writing the manuscript or critical review of its contents. |
REFERENCES
1. Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12(3):167-78. DOI: http://dx.doi.org/10.1038/nrg2933
2. Tannure PN, Oliveira CA, Maia LC, Vieira AR, Granjeiro JM, Costa Mde C. Prevalence of dental anomalies in nonsyndromic individuals with cleft lip and palate: a systematic review and meta-analysis. Cleft Palate Craniofac J. 2012;49(2):194-200. DOI: http://dx.doi.org/10.1597/10-043
3. Chuo CB, Searle Y, Jeremy A, Richard BM, Sharp I, Slator R. The continuing multidisciplinary needs of adult patients with cleft lip and/or palate. Cleft Palate Craniofac J. 2008;45(6):633-8. PMID: 18956932 DOI: http://dx.doi.org/10.1597/07-048.1
4. Coutinho ALF, Lima MC, Kitamura MAP, Ferreira Neto J, Pereira RM. Perfil epidemiológico dos portadores de fissura orofaciais atendidos em um Centro de Referência do Nordeste do Brasil. Rev Bras Saúde Matern Infant. 2009;9(2):149-56. DOI: http://dx.doi.org/10.1590/S1519-38292009000200004
5. Santos P, Maia J. Análise factorial confirmatória e validação preliminar de uma versão portuguesa da escala de auto-estima de Rosenberg. Psicol Teor Invest Prát. 2003;2:253-68.
6. Sbicigo JB, Bandeira DR, Dell’Aglio DD. Rosenberg Self-Esteem Scale (RSS): factorial validity and internal consistency. Psico-USF. 2010;15(3):395-403. DOI: http://dx.doi.org/10.1590/S1413-82712010000300012
7. Bastos PRHO, Gardenal M, Bogo D. The Social Adjustment of Bearers of Craniofacial Abnormalities and the Humanist Praxis. Int Arch Otorhinolaryngol. 2008;12(2):280-8.
8. Noor SN, Musa S. Assessment of patients’ level of satisfaction with cleft treatment using the Cleft Evaluation Profile. Cleft Palate Craniofac J. 2007;44(3):292-303. PMID: 17477746 DOI: http://dx.doi.org/10.1597/05-151
9. Roberts RM, Mathias JL. Psychosocial functioning in adults with congenital craniofacial conditions. Cleft Palate Craniofac J. 2012;49(3):276-85. DOI: http://dx.doi.org/10.1597/10-143
10. Broder HL, Richman LC, Matheson PB. Learning disability, school achievement, and grade retention among children with cleft: a two-center study. Cleft Palate Craniofac J. 1998;35(2):127-31. PMID: 9527309 DOI: http://dx.doi.org/10.1597/1545-1569(1998)035<0127:LDSAAG>2.3.CO;2
11. Domingues ABC, Picolini MM, Lauris JRP, Maximino LP. Desempenho escolar de alunos com fissura labiopalatina no julgamento de seus professores. Rev Soc Bras Fonoaudiol. 2011;16(3):310-6. DOI: http://dx.doi.org/10.1590/S1516-80342011000300012
12. Ribeiro EM, Moreira ASCG. Atualização sobre o tratamento multidisciplinar das fissuras labiais e palatinas. Rev Bras Promoç Saúde. 2005;18(1):31-40.
13. Andrade D, Angerami ELS. A auto-estima em adolescentes com e sem fissuras de lábio e/ou de palato. Rev Latinoam Enferm. 2001;9(6):37-41. DOI: http://dx.doi.org/10.1590/S0104-11692001000600007
14. Singh VP, Moss TP. Psychological impact of visible differences in patients with congenital craniofacial anomalies. Prog Orthod. 2015;16:5. DOI: http://dx.doi.org/10.1186/s40510-015-0078-9
15. Chan RK, McPherson B, Whitehill TL. Chinese attitudes toward cleft lip and palate: effects of personal contact. Cleft Palate Craniofac J. 2006;43(6):731-9. PMID: 17105325 DOI: http://dx.doi.org/10.1597/05-111
1. Hospital de Clínicas de Porto Alegre, Porto
Alegre, RS, Brazil.
2. Faculdade de Medicina, Universidade Federal do
Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author: Alesandra
Glaeser
Rua João Ernesto Schmidt, 251/701
Porto Alegre, RS, Brazil
Zip Code 91210-125
E-mail: aglaeser@hcpa.edu.br
Article received: November 10, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter