

Original Article - Year 2018 - Volume 33 -
Liposuction Practices among Brazilian Surgeons
Condutas em lipoaspiração entre cirurgiões brasileiros
ABSTRACT
Introduction: Since the 1980s, with Illouz, liposuction has gained popularity and
represents one of the most commonly performed procedures in the world today.
Some of the complications are serious and potentially lethal. Nevertheless,
uniformity in its practice or the manner in which it is taught does not
exist. Evaluating techniques employed by plastic surgeons may be the start
toward standardization.
Methods: A questionnaire on liposuction was given to plastic surgeons of different age
groups and from regions of Brazil who were present at the 52nd
Brazilian Conference for Plastic Surgery.
Results: Two hundred forty-three questionnaires were filled out (n = 243). The average
number of incisions was 9 (2-16). Two hundred forty-one surgeons (99%) made
incisions along the anterior median/paramedian line, and 236 (97%) made
incisions on the posterior median/paramedian line. Approximately half of
those surveyed utilized general anesthesia. Two hundred nine surgeons (86%)
placed the patient in the prone position during the procedure. One hundred
forty-six (60%) interviewees performed superficial liposuction, with 22 (9%)
performing liposuction only on this adipose layer. Eighty-five (35%)
participants reported controlling the apparatus's pressure during the
procedure.
Conclusion: Liposuction procedures performed in Brazil have significant technical
variations. This finding encourages us to reflect on the need to standardize
liposuction practice and the manner in which it is taught so as to increase
control over the procedure and its safety.
Keywords: Lipectomy; Subcutaneous abdominal fat; Dorsal; Patient positioning; Anesthesia
RESUMO
Introdução: Desde a década de 1980, com Illouz, a lipoaspiração ganhou popularidade e
representa hoje um dos procedimentos mais realizados no mundo. Algumas de
suas complicações são graves e potencialmente letais. Não existe, contudo,
uma uniformidade em sua prática ou no seu ensino. A avaliação das técnicas
empregadas por cirurgiões plásticos pode ser o início de uma
padronização.
Métodos: Foi aplicado um questionário sobre lipoaspiração no 52º Congresso Brasileiro
de Cirurgia Plástica para cirurgiões plásticos de diferentes faixas etárias
e regiões do Brasil, presentes no evento.
Resultados: Foram contabilizados 243 questionários preenchidos (n = 243). O número médio
de incisões foi de 9 (2 - 16). Duzentos e quarenta e um cirurgiões (99%)
realizam incisões na linha mediana/paramediana anteriormente e 236 (97%)
incisam na linha mediana/paramediana na região posterior. Aproximadamente
metade dos questionados utilizam a anestesia geral. Duzentos e nove
cirurgiões (86%) posicionam o paciente em decúbito ventral durante o
procedimento. A lipoaspiração superficial é realizada por 146 (60%)
entrevistados, sendo que 22 (9%) fazem a aspiração apenas desta camada
adiposa. Oitenta e cinco (35%) participantes relatam controlar a pressão do
aparelho durante o procedimento.
Conclusão: A lipoaspiração realizada no Brasil apresenta grande variação técnica. Essa
constatação nos faz refletir sobre a necessidade de uma uniformização de sua
prática e ensino a fim de aumentar o controle e a segurança do
procedimento.
Palavras-chave: Lipectomia; Gordura subcutânea abdominal; Dorso; Posicionamento do paciente; Anestesia
INTRODUCTION
Charles Dujarier first performed liposuction in the 1920s by curettage of adipose tissues1. At the time, it presented a great number of complications.
In 1982, Illouz2 revolutionized the procedure by using a rhombus instrument connected to a suction device. This technique gained considerable popularity for drastically reducing complications. Today, it is the best treatment for adipose tissue. In the 1990s, Klein3 introduced the tumescent liposuction method, and Zocchi4 reported the use of ultrasound-assisted liposuction.
In 2015, it was the second most commonly performed plastic surgery in the world, with 1,394,588 cases according to the International Society for Aesthetic Plastic Surgery (ISAPS). In Brazil, it was the most commonly performed plastic surgery, with 182,765 cases5.
The Brazilian Society of Plastic Surgery exhibits similar numbers, with liposuction accounting for one-third (32%) of all procedures performed by surgical specialists in the country6. Nearly 16.07% of the legal cases in plastic surgery are due to liposuction6.
Despite its importance, a standard for conducting the procedure7 still does not exist, much less a uniformity in teaching surgeons in training.
Liposuction has potentially lethal complications. Grazer and Jong8 reported that the cause in 23% of the deaths was pulmonary thromboembolism, followed by abdominal perforation in 14.6% of cases.
A study on standardization may reduce these complications and increase the patients’ safety.
METHODS
A questionnaire (Annex 1) was given to surgeons of different age groups and from regions of Brazil who were registered and present at the 52nd Brazilian Conference for Plastic Surgery, which took place on November 12-15, 2015 in Belo Horizonte, Minas Gerais. The study followed the principles of the Declaration of Helsinki during its elaboration, and the participants authorized publication of the results.
RESULTS
A total of two hundred forty-three (n = 243) questionnaires were filled out and received.
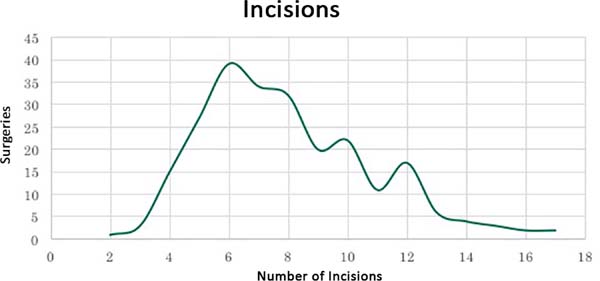
Each interviewee was asked to perform a liposuction procedure on the anterior and posterior torso (Figure 1). The number of incisions varied from 2 to 16, with an average of 9 incisions per surgery (Figure 2). Two hundred twenty-eight (94%) surgeons preferred to position the incisions in locations covered by underwear or swimwear. One hundred eighty-five (76%) made incisions on the umbilical scar. One hundred ninety-four (80%) surgeons positioned the scar on the median/paramedian line and 18 (7.5%) made an incision on the lateral region between the anterior and posterior axillary lines.
Regarding movement vectors, most of the surgeons conduct movements in the medial region to both the anterior and posterior lateral regions (99% and 97%, respectively). Movement of the lateral areas to the medial region was performed by 5% and 11% of the surgeons, respectively.
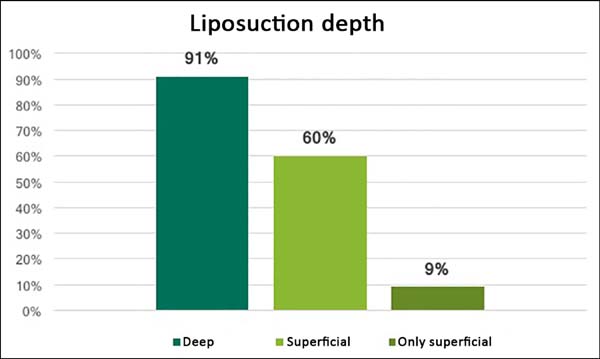
Given that a large volume of fat was to be removed, 219 (90%) surgeons affirmed that they performed deep liposuction under Scarpa’s fascia. At the same time, 143 (59%) surgeons advocated superficial liposuction for better body contours (Figure 3).
Nearly half of the interviewees administered general anesthesia to perform the procedure. One hundred seven (44%) surgeons used epidural anesthesia, and 15 (6%) used spinal anesthesia.
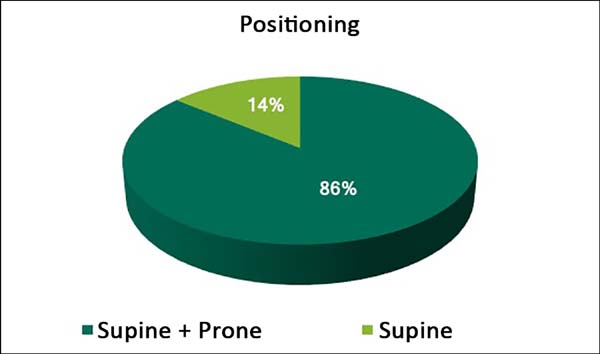
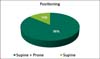
Two hundred nine (86%) surgeons changed the patient’s position during surgery using both the prone and supine positions. Just 34 (14%) surgeons performed liposuction only in the supine position (Figure 4).
One hundred twenty-six (52%) surgeons observed the pressure on the liposuction apparatus; 87 (36%) surgeons performed the procedure under controlled pressure.
DISCUSSION
A large quantitative and qualitative variation in incisions was observed. The number varied nearly by 800%. The literature defends performing the least amount of incisions possible that can allow appropriate liposuction of the desired area and the perpendicular crisscross subcutaneous tunnels9. Correct positioning of the incisions also means reducing the exposure of the resulting scars9, which has been observed in 94% of the cases.
Most surgeons provide access for the liposuction from the median/paramedian line, both in the anterior and posterior regions (99% and 97% respectively). This median/paramedian access might explain why a significant number of professionals (86%) need to change the patient’s position for dorsal liposuction.
Liposuction with the patient in the prone position must be performed with an emphasis on adequate monitoring of the patient, in order to avoid potential complications such as cervical lesions, ocular lesions, air embolism, venous thromboembolism10, bradycardia, and cardiac arrest10,11. In this questionnaire, complications related to position change were 5%; however, they were all systemic and potentially serious.
Most of the interviewees (90%) performed deep liposuction, in order words, under Scarpa’s fascia. Although the literature argues that superficial liposuction increases the chances of local complications such as scar contractures, skin dyschromia, and abrasions12, nearly 60% of the specialists still utilize this technique. A small portion (9%) of surgeons defended superficial liposuction only due to apprehensions regarding cavity perforation.
No anesthetic technique was predominant. The anesthesia technique administered depended on the preference of the surgeon or that of the center where the procedure was performed. However, in large-volume liposuctions, the use of general anesthesia was advised due to the important risks of vasodilation and hypertension11. General anesthesia allows more control over the utilization of drugs, the patient’s movements, and the handling of air passageways13. In Brazil, we verified that the majority of the procedures were performed with general anesthesia, followed by the use of epidural anesthesia, with a considerable portion of the procedures utilizing it.
The surgeons demonstrated little preoccupation (35%) with observing and/or controlling the pressure on the liposuction apparatus. The lack of a definition of an ideal pressure in the literature to this very day leaves an important variable open. There are already authors that defend low-pressure liposuction, which would reduce blood loss and local trauma14. This fact was recently corroborated in works on lipografting that demonstrates cellular damage at elevated negative pressures (≥13.5 PSI)15. If there is a correlation among negative pressure, tissue damage, and systemic inflammatory response in the postoperative phase, controlling the pressure must be considered a routine part of the surgeons’ practice.
CONCLUSION
In conclusion, liposuction practice in Brazil presents a great diversity of techniques and little standardization.
There is a need for further studies on the most performed plastic surgery procedure in Brazil. Further studies are required to improve knowledge and standardize its practice, as well as identify ideal methods of teaching it, with the objective of reducing the number of intercurrences and increasing patient safety.
COLLABORATIONS
|
GMCS |
Analysis and/or interpretation of data; statistical analyses; conception and design of the study; completion of surgeries and/ or experiments; writing the manuscript or critical review of its contents. |
|
SMC |
Final approval of the manuscript; conception and design of the study |
|
MHLR |
Analysis and/or interpretation of data; statistical analyses; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
CSS |
Analysis and/or interpretation of data; final approval of the manuscript. |
|
LMF |
Analysis and/or interpretation of data; final approval of the manuscript. |
REFERENCES
1. Fodor PB. Reflections on lipoplasty: history and personal experience. Aesthet Surg J. 2009;29(3):226-31. DOI: http://dx.doi.org/10.1016/j.asj.2009.02.007
2. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7. PMID: 6622564 DOI: http://dx.doi.org/10.1097/00006534-198311000-00001
3. Klein JA. The tumescent technique. Anesthesia and modified liposuction technique. Dermatol Clin. 1990;8(3):425-37.
4. Zocchi M. Ultrasonic-assisted lipoplasty. Adv Plast Reconstr Surg. 1998;11:197-221.
5. International Society for Aesthetic Plastic Surgery (ISAPS). ISAPS International Survey on Aesthetic/Cosmetic. Hanover (NH): ISAPS; 2015 [acesso 2018 Maio 29]. Disponível em: https://www.isaps.org/wp-content/uploads/2017/10/2016-ISAPS-Results-1.pdf
6. Cirurgia Plástica Segura. Revista Brasileira de Cirurgia Plástica - Edição Especial 2016.
7. Khanna A, Filobbos G. Avoiding unfavorable outcomes in liposuction. Indian J Plast Surg. 2013;46(2):393-400. DOI: http://dx.doi.org/10.4103/0970-0358.118618
8. Grazer FM, Jong RH. Fatal outcomes from liposuction: census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105(1):436-46. DOI: http://dx.doi.org/10.1097/00006534-200001000-00072
9. Shiffman MA. Prevention and treatment of liposuction complications. In: Shiffman MA, Di Giuseppe A, eds. Liposuction - Principles and Practice. 1st ed. New York: Springer; 2006. p. 333-41.
10. Edgcombe H, Carter K, Yarrows S. Anaesthesia in the prone position. Br J Anaesth. 2008;100(2):165-83. DOI: http://dx.doi.org/10.1093/bja/aem380
11. Brown J, Rogers J, Soar J. Cardiac arrest during surgery and ventilation in the prone position: a case report and systematic review. Resuscitation. 2001;50(2):233-8. DOI: http://dx.doi.org/10.1016/S0300-9572(01)00362-8
12. Kim YH, Cha SM, Naidu S, Hwang WJ. Analysis of postoperative complications for superficial liposuction: a review of 2398 cases. Plast Reconstr Surg. 2011;127(2):863-71. PMID: 21285789 DOI: http://dx.doi.org/10.1097/PRS.0b013e318200afbf
13. American Society of Plastic Surgeons (ASAPS). Practice Advisory on Liposuction: Executive Summary; Arlington Heights: ASAPS; 2003 [acesso 2018 Maio 29]. Disponível em: https://www.plasticsurgery.org/documents/medical-professionals/health-policy/key-issues/Executive-Summary-on-Liposuction.pdf
14. Elam MV, Packer D, Schwab J. Reduced negative pressure liposuction (RNPL): Could less be more? Int J Aesth Restor Surg. 1997;5:101-4.
15. Shiffman MA, Mirrafati S. Fat transfer techniques: the effect of harvest and transfer methods on adipocyte viability and review of the literature. Dermatol Surg. 2001;27(9):819-26.
Questionnaire.
| Name:
___________________________________________________________________________________________________________ E mail: ___________________________________________________ Aspiring: _____ Specialist: _____ Official:_____ 1 - Do you work with liposuction? ( ) YES ( ) NO 2 - Have you ever had a case of death related to liposuction? ( ) YES ( ) NO 3 - If yes, what was the primary problem? 4 - Have you ever had a systemic complication in liposuction? ( ) YES ( ) NO 5 - If so, what was it? 6 - What was the outcome/sequela? 7 - What type of anesthesia do you prefer for liposuction? 8 - Do you change the patient's position to the prone position to perform dorsal liposuction? ( ) YES ( ) NO 9 - Have you ever had a specific complication arise from this moment? What was it? 10 - What incision do you make to perform liposuction in the thoracic dorsal region? 11 - What incision do you make to perform liposuction in the sacral lumbar region? 12 - What incision do you make to perform liposuction in the abdomen? 13 - What incision do you make to perform liposuction in the flank? 14 - If you have had a case of perforation, where was it located? What was the incision? 15 - Do you perform deep liposuction? Why? 16 - Do you perform superficial liposuction? Why? 17 - Have you ever had local complications in liposuction? What were they? 18 - Do you know the negative pressure value of your liposuction apparatus? ( ) YES ( ) NO 19 - Do you regulate or control the pressure on the apparatus during the procedure? ( ) YES ( ) NO 20 - If so, what do you consider to be the ideal liposuction pressure? |
1. Hospital Felício Rocho, Belo Horizonte, MG,
Brazil.
2. Universidade Federal de São Paulo, São Paulo,
SP, Brazil.
Corresponding author: Gustavo Moreira Costa
de Souza
Rua Timbiras, 3642/504 - Barro Preto
Belo Horizonte, MG,
Brazil Zip Code 30140-062
E-mail: gustavomcsouza@gmail.com
Article received: June 27, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter