

Original Article - Year 2018 - Volume 33 - Issue 2
Perception of breast cancer and breast reconstruction in medical school students
Percepção dos internos de uma faculdade de medicina sobre o câncer de mama e reconstrução mamária
ABSTRACT
Introduction: Breast cancer is the most common type of cancer among women in the world and
in Brazil, after non-melanoma skin cancer. Our objective was to evaluate the
medical students' perception of breast cancer and breast reconstruction.
Methods: This is a cross-sectional pilot study composed of students from the fifth and
sixth year of medical school, in May 2016.
Results: We questioned whether there is a possibility of breast reconstruction after
mastectomy, and the response was unanimous (100%). For a better
characterization, we asked if the reconstruction could be done at the same
time as the mastectomy, and 69 (57.5%) students said yes and 51 (42.5%)
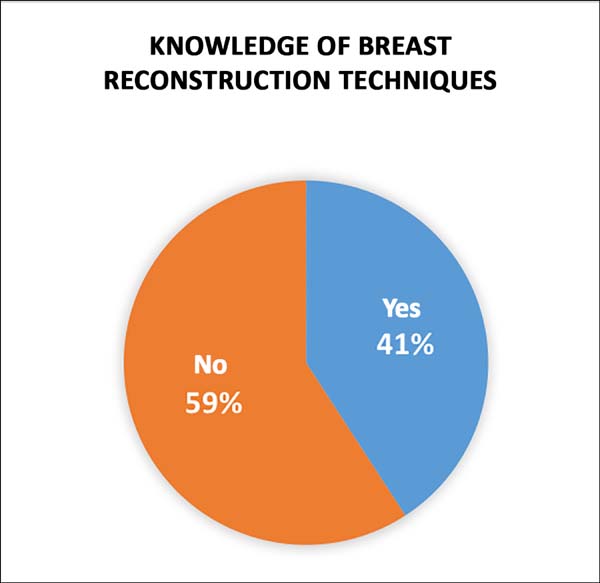
denied. In the analysis of surgical knowledge, we asked whether they knew
any breast reconstruction technique, and 49 (40.83%) answered yes and 71
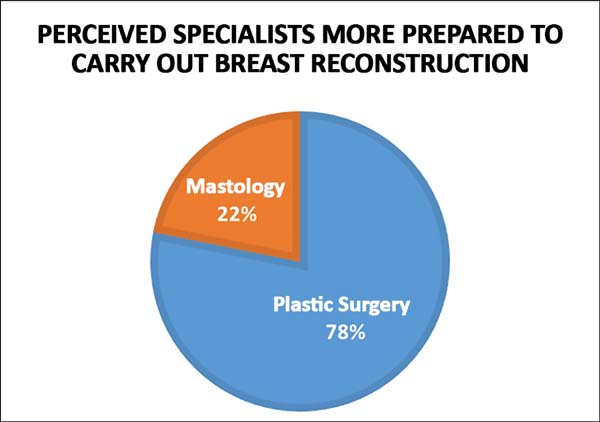
(59.16%) denied knowing. With regard to referral to a medical specialist who
was better prepared to follow and perform breast reconstruction, 93 (77.5%)
students chose plastic surgery and 26 (21.66%) chose mastology. Regarding
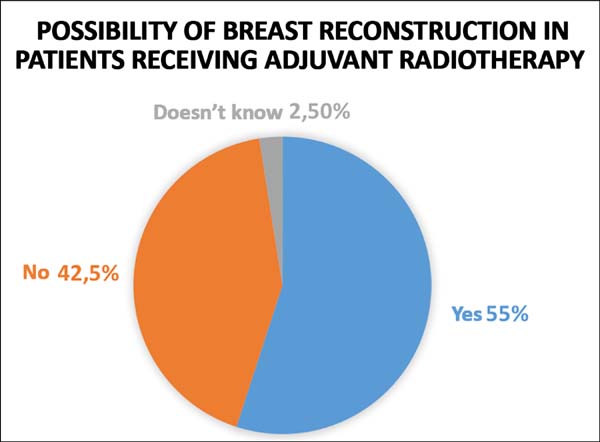
the possibility of breast reconstruction in patients who need to undergo
adjuvant radiotherapy, 66 (55%) answered yes, 51 (42.5%) did not answer, and
three (2.5%) did not know how to respond. Regarding this possibility in
patients with silicone implants, 59 (49.16%) answered yes, three (2.5%)
answered no, and 58 (48.33%) said they did not know about the subject.
Conclusion: We conclude that mastology has been gaining immense interest in the field of
breast reconstruction, including in the academic world, based on the high
percentage of respondents who stated that they are better prepared for this
procedure than for plastic surgery for breast reconstruction.
Keywords: Inflammatory breast neoplasms; Mammaplasty; Reconstructive surgical procedures; Mastectomy, segmental; Disease prevention
RESUMO
Introdução: O câncer de mama é o tipo mais comum entre as mulheres no mundo e no Brasil,
depois do câncer de pele não melanoma. O objetivo é avaliar a percepção dos
estudantes de medicina sobre o câncer de mama e reconstrução mamária.
Métodos: Trata-se de estudo transversal piloto composto por alunos do 5º e 6º ano de
curso de medicina, realizado de maio de 2016.
Resultados: Foi questionado se há possibilidade de reconstrução mamária após a
mastectomia, sendo que de forma unânime 100% foi sim. Para melhor
caracterização, foi perguntado se a reconstrução pode ser feita no mesmo
momento da mastectomia, 69 (57,5%) estudantes marcaram sim e 51 (42,5%)
negaram. Em análise aos conhecimentos cirúrgicos, foi perguntado se os
mesmos conhecem alguma técnica de reconstrução mamária, sendo que 49
(40,83%) responderam que sim e 71 (59,16%) negaram conhecer. Em relação ao
encaminhamento à especialidade médica mais preparada para acompanhar e
realizar a reconstrução mamária, 93 (77,5%) discentes elegeram a cirurgia
plástica e 26 (21,66%) a mastologia. Quanto à possibilidade de reconstrução
de mama em pacientes que farão radioterapia adjuvante, 66 (55%) responderam
sim, 51 (42,5%) não e 3 (2,5%) não souberam responder. Quanto a esta
possibilidade mesmo em pacientes com implantes de silicone, 59 (49,16%)
responderam sim, 3 (2,5%) responderam não e 58 (48,33%) afirmaram não saber
sobre o assunto.
Conclusão: Observou-se que a Mastologia vem ganhando espaço na reconstrução de mama,
inclusive no meio acadêmico, devido ao alto percentual de resposta de que a
mesma seria mais preparada do que a Cirurgia Plástica para reconstrução
mamária.
Palavras-chave: Neoplasias inflamatórias mamárias; Mamoplastia; Procedimentos cirúrgicos reconstrutivos; Mastectomia segmentar; Prevenção de doenças
INTRODUCTION
According to the National Cancer Institute (INCA) database, breast cancer is the most common type of cancer among women in the world and in Brazil, after non-melanoma skin cancer. Breast cancer accounts for about 25% of the new cancer cases each year.
Data from the international literature are similar to those of our country, which demonstrate that mortality rates increase with age. According to data from the American Cancer Society, between 2002 and 2006, 95% of new cases and 97% of deaths due to breast cancer occurred in women aged 40 years or older1. During the same year, the mean age at diagnosis was 61 years. As for ethnicity, white women were seen to be at higher risk of developing breast cancer than African-American women2.
Through identifying groups at risk of developing cancer and tracing the genetic profile of a particular tumor, we can classify the cancer and outline different treatment strategies. Thus, breast cancer can be divided into subtypes based on the molecular characteristics of its cells. Each of these subtypes has different clinical properties, clinical behavior, and survival characteristics1,3.
The main types of breast cancer are ductal carcinoma in situ, invasive ductal carcinoma, and invasive lobular carcinoma. In situ ductal carcinoma is an early stage breast cancer, is unable to metastasize in its early stages. Invasive ductal carcinoma, is the most common type of breast cancer and has the capacity to metastasize. Invasive lobular carcinoma is the second most common type of breast cancer and is related to the risk of developing cancer in other breast and ovary-associated tissues, in addition to posing a high risk of metastasis.
However, it is important to emphasize that there are certain types of breast lesions that can predispose a patient to cancer, such as lobular carcinoma in situ or lobular neoplasm, atypical ductal hyperplasia, and atypical lobular hyperplasia.
As a result of these genetic disorders, one can infer the main signs and symptoms of breast cancer, which include fixed nodules or lumps of hardened and painless consistency, a reddish or retracted appearance of the skin, changes in the nipple, small nodules in the axillary region or neck, and papillary discharge. The early detection of breast cancer exponentially increases the chances of successful treatment outcomes. Once the tumor is diagnosed in its early stages, either during the process of tumorigenesis or at the very initial stage, a curative treatment is possible.
To foster the need and importance of prevention, the month of October was elected as the epicenter for the intensification of a campaign against breast cancer. October Rosa is a campaign to raise awareness among the general population and especially women about the importance of breast cancer prevention and its early diagnosis.
In a historical moment, the movement was initiated in 1990 as Race for the Cure, which was held in New York and has now been held continually in the city. The name of the movement indicates towards the color of the tie that symbolizes, globally, the fight against breast cancer and stimulates the participation of companies, entities, and the world population.
Despite the process of globalization, which allows media coverage throughout the world and enables statistical measurements with respect to the incidence rates of breast cancer by the Ministry of Health, a significant number of people still lack comprehensive knowledge about this subject. For this, it is imperative to conduct research to determine the degree of knowledge among medical students.
As they constitute the class of future professionals and opinion-formers, the importance of specific knowledge is emphasized, not only with regard to the prevention and identification of breast cancer, but also with respect to reception, counseling, and referral to different medical specialists who are qualified to provide different levels of attention and treatment in correspondence with the type and stage of tumor, to improve survival rates and other related health indicators.
In view of the aspects mentioned above, it is essential to have prevention and early identification measures for breast cancer. Such measures include screening exams, which can detect the tumor before the appearance of symptoms or perception by the patient, especially mammography, which in some cases can be complemented with ultrasonography or magnetic resonance imaging of the breasts.
In addition, the information and execution of breast self-examinations in the knowledge of the body and in the detection of changes are extremely important. In Brazil, the Ministry of Health’s recommendation is to perform screening mammography (when there are no signs or symptoms) in women aged 50 to 69 years, every two years, according to the INCA database.
Regarding treatments, it is worth emphasizing the importance of a qualified professional for each stage of the disease. In this context, the specialists may be involved in multidisciplinary fields, for example mastologists, oncologists, radiotherapists, psychologists, physiotherapists, dentists, plastic surgeons, geneticists, and others.
The standard treatment for early stage breast cancer is surgery, wherein either specific breast segments are removed or radical mastectomy is performed. The success of the treatment is determined based on the psychological evaluation of the patient, which includes immediate breast reconstruction with social reintegration of the patient.
In a systematic review of the literature4, the rate of breast reconstruction was shown to be highly variable and related to doubts about adjuvant therapy, i.e. if the patient can undergo chemotherapy or radiotherapy after surgery and the indication and beliefs of the attending physician about the procedure.
Breast reconstruction involves multiple procedures that are performed in a number of stages, which can either be performed simultaneously with mastectomy or postponed until the end of cancer treatment. Among the techniques that have been described for breast reconstruction, we highlight the use of autologous tissues and implants. Of the autologous tissues, one procedure involves the use of myocutaneous flaps, where tissues from areas adjacent to where mastectomy has been performed are transferred. These areas may include the skin and subcutaneous cellular tissue and muscles, which are most commonly used, and the dorsal large muscle flap and the transverse rectus abdominis muscle.
Implant reconstructions can be performed in two stages, with the aid of expanders, when there is a need for a skin “gain” after radical non-skin sparing mastectomies, followed by replacement of the expander with silicone implants in a second surgery.
Despite efforts to popularize preventive measures through the media, much of the population remains unclear about many aspects of the disease and the medical specialties to go to for appropriate treatment. In order to effectively educate the world population about this disease, it is first necessary to train health professionals, mainly medical students and general practitioners, so that they can correctly refer to the competent medical specialties at each stage of treatment. This is the underlying motivation for the present study.
OBJECTIVE
The overall objective was to assess medical students’ perceptions of breast cancer and breast reconstruction. Among the specific objectives, we aimed to evaluate the degree of knowledge about the importance of breast examinations, the recognition of risk factors for breast cancer, the perception about the indication of methods for diagnosing and treating breast cancer, and their applicability. We also proposed measures to guide the specialists involved in breast cancer diagnosis and treatment.
METHODS
This is a cross-sectional pilot study composed of fifth and sixth year students from our private higher education medical institution in Brasília - DF, held in May 2016. One hundred and twenty volunteers were enrolled in the study, from a total of 160 students, 40 of whom were excluded from the study due to a lack of response.
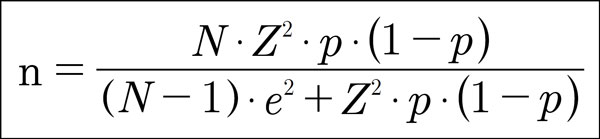
The sample size to estimate the proportion of a given characteristic in a population was based on two parameters: the margin of error and confidence level. For the present study, the margin of error and the confidence level were set at 5% and 95%, respectively.
For these parameters, the sample size required for the study, from a total of 160 students who were enrolled in the boarding school (5th and 6th year) of the research institution was 114 students, which was calculated by the formula (Figure 1):
Where:
N = the sample size to be calculated
N = Total size (total number of students enrolled in grades 5 and 6)
Z = was the deviation from the mean value, accepted to reach the desired confidence level. As a function of the ideal confidence level (95%), the value was determined by the Gauss probability distribution form, with Z = 1.96.
E = was the maximum allowed error margin, 5%.
P = was the proportion that we expected to find in the population. In this study, since there is no expected proportion, it was assumed to be p = 50%, and consequently, (1-p) = 50%.
The instrument used in this study was the self-administered questionnaire, with questions that were elaborated by the researchers. It consisted of the following themes:
Knowledge of breast self-examinations;
Risk factors for breast cancer;
Types of complementary diagnostic tests;
Indication of complementary examinations by age/predisposition;
Medical specialties involved in this area, both in follow-up and treatment;
Types of treatments;
Professionals responsible for performing breast reconstruction.
These questionnaires were applied anonymously, and participants signed informed consent.
The questionnaire was applied within the classrooms of the institution, for the above mentioned students of the medical course, because in the case of personal questions, this application method increased the chances of the information being anonymous and valid.
RESULTS
Of the 120 students interviewed in the fifth and sixth years, 58 (48.3%) were women and 62 (51.3%) were men.
The majority of the students 95 (79.16%) were between the ages of 22 and 28 years. Ninety-eight (81.66%) were unmarried, 22 (18.3%) were married, and 17 (14.16%) had previously completed an advanced degree.
Of the total number of students interviewed, 40 (33.33%) stated that they performed breast self-examinations and 80 (66.66%) denied it. Of those who reported self-examinations of the breasts, 36 (90%) were women. Among the students who affirmed to perform breast self-examinations, 21 (52.5%) performed monthly examinations, 10 (25%) performed annual examinations, eight (20%) performed weekly examinations, and one (2.5%) performed daily examinations. Among those who refused to perform breast self-examinations (n = 80), 16 (20%) did not consider them to be important and 64 (80%) claimed other reasons.
In the questionnaire about the significance of breast self-examinations, the following results were obtained: 74 (61.66%) responded for prevention/diagnosis of breast cancer, 28 (23.33%) responded for knowledge of one’s own body, six (5%) stated that it is not important, and 12 (10%) responded that it has another meaning. Subsequently, the clinical breast examination questionnaire was administered, and of the 120 interviewees, 53 (44.16%) had already undergone clinical breast examinations, of whom 47 (88.67%) were women, 34 (64.15%) performed examinations at annually, eight (15.09%) semiannually, three (5.66%) performed once per two years, and eight (15.09%) performed once per three years.
Among these students, for 38 (71.60%) the exams were performed by a gynecologist, for eight (15.09) by a general practitioner, for five (9.43%) by a mastologist, for one (1.88%) by a plastic surgeon, and for one (1.88%) by another specialist. Sixty-seven students (55.83%) denied having been examined.
Due to the incidence of breast cancer, volunteers were questioned whether they could have breast cancer at some time in their lives, and 109 (90.83%) answered yes and 11 (9.16%) denied the possibility. In the analysis of the risk factors related to breast cancer, 102 (85%) students affirmed a family history in first-degree relatives, life habits, advanced age, and nulliparity; 11 (9.16%) students admitted only to having a family history in first-degree relatives, three (2.5%) admitted to the life habits category, one (0.83%) to advanced age, and three (2.5%) to other factors.
On the other hand, we questioned if breast cancer had a cure and unanimously (100%), the answer was yes. Next, we questioned a good method to discover breast cancer early, while the cancer was very small, and the following responses were obtained: 93 (77.5%) chose mammography, 13 (10.83%) self -examination, 11 (9.16%) ultrasonography, and three (2.5%) clinical examination. The best age for mammography for an examination in patients who were at increased risk for breast cancer, with a family history in first-degree relatives, was enquired about and 78 (65%) students answered from the age of 35, 31 (25.83%) answered before the age of 35, and 11 (9.16%) answered over 40 years.
In a questionnaire on the medical specialty that was better prepared to follow and treat patients with breast cancer, 65 (54.16%) students said mastology, 43 (35.83%) said oncology, eight (6.66%) said plastic surgery, three (2.5%) said gynecology, and one (0.83%) said other specialties. For the interviewees, the best perceived treatment for breast cancer was asked for, and 67 (55.84%) stated mastectomy, 22 (18.33%) quadrantectomy, 14 (11.66%) chemotherapy and radiotherapy, and 17 (14.16%) said none of the above.
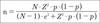
In order to evaluate the degree of knowledge of diagnosis and treatment, we questioned whether there is a possibility of breast reconstruction after the mastectomy, and the answer was unanimously yes (100% of the respondents). For better characterization, we asked if the reconstruction could be performed at the same time as the mastectomy, and 69 (57.5%) students scored yes and 51 (42.5%) denied the possibility (Figure 2). In the surgical part, we asked whether they were aware of any breast reconstruction technique, and 49 (40.83%) said yes and 71 (59.16%) said no (Figure 3).
With regards to referral to medical specialists who are better prepared to follow and perform breast reconstruction, 93 (77.5%) students chose plastic surgery and 26 (21.66%) chose mastology (Figure 4). We asked whether there is a possibility of breast reconstruction in patients who are supposed to undergo radiotherapy after surgery (adjuvant radiotherapy) and 66 (55%) students answered yes, 51 (42.5%) answered no, and three (2.5%) could not answer. In a more objective question, we asked whether this possibility exists in patients with silicone implants, and 59 (49.16%) answered yes, three (2.5%) answered no, and 58 (48.33%) said that they did not know.
We evaluated whether breast reconstruction would have a positive impact on the quality of life of women who underwent mastectomy, and unanimously (100%), the respondents answered yes. Therefore, they were asked if they knew someone who had breast reconstruction, and 23 (19.16%) said yes and 97 (80.83%) said no. In the group of people who stated that they knew someone who had undergone breast reconstruction, 17 (73.91%) reported that it had been performed by a plastic surgeon, three (13.04%) reported by mastologist, and three (13.04%) jointly by a mastologist and plastic surgeon.
DISCUSSION
The present study is one of the pioneering works in national literature that evaluates the perception of health professionals, especially of medical students.
As to the level of knowledge of medical students about the importance of breast examination, more than half (66.66%) of the respondents did not undergo breast self-examinations, and 20% did not consider them important. The literature shows the importance of this easy and inexpensive exam. It can be performed by a trained doctor or nurse and presents 57-83% sensitivity among women between 50 and 59 years of age and around 71% among those who are between 40 and 49, according to data from INCA, 2016.
Regarding the recognition of risk factors for breast cancer, most students knew that they are important and should be evaluated along with the clinical history of their patients.
Regarding the perception about the indication of diagnostic and treatment methods for breast cancer and their applicability, the students recognized the importance of mammography as a method of choice in the screening, prevention, and diagnosis of breast cancer, as well as the age and periodicity of the examination. About 57% of the students recognized the possibility of immediate breast reconstruction after mastectomy. Concerning breast reconstruction techniques, only 49 (40.83%) students had already heard about the subject, which may be the focus of the measures of the Brazilian Society of Plastic Surgery, in order to guide these techniques and the specialists who are most prepared to carry them out.
The students recognized that the most suitable medical specialty to accompany and perform breast reconstruction is plastic surgery (77.5%) against mastology (21.66%). However, we can assume that mastology has been gaining interest in the field of breast reconstruction, especially in the academic environment, due to the high percentage of responses that indicated that such specialists would be better prepared than plastic surgeons for breast reconstruction.
All students acknowledged breast reconstruction as an option after mastectomy, but a large part (42.5%) believed that it is not possible to perform the mastectomy simultaneously, and more than half (59.16%) of the interviewees were unaware of breast reconstruction techniques. In addition, many (42.5%) were unaware of the possibility of post-reconstruction radiotherapy, including reconstructions with silicone prostheses.
A study by Maluf et al.5 revealed that 68% of the patients submitted to immediate reconstruction were very satisfied with the aesthetic result of the surgery. Conversely in the late reconstruction group, a great degree of psychological suffering and relegation of the psychological functions were seen due to low self-esteem.
It is also known that the complete treatment of patients with breast reconstruction contributes to an improved quality of life, the preservation of self-image, increases the sense of femininity, improves sexual relationships, and provides a less traumatic rehabilitation process in these women6. Therefore, it is important that undergraduates understand the subject in order to properly guide patients in their search for specialists who can offer appropriate treatment.
CONCLUSION
Students in the fifth and sixth year of medical school in the Federal District showed a good perception of breast cancer, regarding physical and imaging exams, risk factors, and therapeutic possibilities. However, these students need to be more educated and better guidance is required with respect to questions regarding breast reconstruction after mastectomy and the specialties involved, so that they can effectively guide their future patients and refer them to the appropriate professionals who have a positive perception about the possibilities of treatment that may improve the quality of life of patients with breast cancer.
Additional studies are needed, but this work provides a basis to encourage the Brazilian Society of Plastic Surgery with informative measures and medical students with information about the important role of plastic surgery in breast reconstruction.
COLLABORATIONS
|
LDPB |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
DBP |
Final approval of the manuscript. |
|
VSD |
Completion of surgeries and/or experiments. |
|
JRN |
Conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
GCS |
Writing the manuscript or critical review of its contents. |
|
DASS |
Writing the manuscript or critical review of its contents. |
REFERENCES
1. American Cancer Society. Breast Cancer Facts & Figures 2009-2010 [acesso 2018 Maio 25]. Disponível em: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2009-2010.pdf
2. Allred DC. Assessment of Prognostic and Predictive Factors in Breast Cancer by Immunohistochemistry ER. Breast, p. 2005- 2006, 2005.
3. Fukutomi T, Akashi-Tanaka S. Prognostic and predictive factors in the adjuvant treatment of breast cancer. Breast Cancer. 2002;9(2):95-9.
4. Brennan ME, Spillane AJ Uptake and predictors of post-mastectomy reconstruction in women with breast malignancy--systematic review. Eur J Surg Oncol. 2013;39(6):527-41. DOI: 10.1016/j.ejso.2013.02.021
5. Maluf MFM, Jo Mori L, Barros ACSD. O impacto psicológico do câncer de mama. Rev Bras Cancerol. 2005;51(2):149-54.
6. Almeida RA. Impacto da mastectomia na vida da mulher. Rev SBPH. 2006;9(2):99-113.
1. Hospital Daher Lago Sul, Brasília, DF,
Brazil.
Corresponding author: Diogo Borges
Pedroso
SEP/ Sul, 709/909, Centro Médico Julio Adnet, Clínica 20
Brasília, DF, Brazil Zip Code 70390-095
E-mail: dpedroso@gmail.com
Article received: November 20, 2016.
Article accepted: May 17, 2018.
Conflicts of interest: none.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter